Aneurisma da aorta abdominal
- Visão geral
- Teoria
- Diagnóstico
- Tratamento
- ACOMPANHAMENTO
- Recursos
Algoritmo de tratamento
Observe que as formulações/vias e doses podem diferir entre nomes e marcas de medicamentos, formulários de medicamentos ou localidades. As recomendações de tratamento são específicas para os grupos de pacientes:ver aviso legal
aneurisma da aorta abdominal (AAA) roto
medidas de ressuscitação padrão
Medidas de ressuscitação padrão devem ser iniciadas imediatamente. Isso inclui: manejo das vias aéreas (oxigênio suplementar ou intubação endotraqueal e ventilação assistida se o paciente estiver inconsciente); obtenção de acesso intravenoso (cateter venoso central); cateter arterial e cateter urinário; garantir a disponibilidade de hemoderivados (eritrócitos concentrados, plaquetas e plasma fresco congelado) e transfusão para ressuscitação, anemia grave e coagulopatia; e notificação da equipe de anestesistas, da unidade de terapia intensiva (UTI) e da equipe cirúrgica.
A intensa reposição de fluidos pode causar coagulopatia dilucional e hipotérmica e ruptura secundária de coágulos em função do aumento do fluxo sanguíneo, aumento da pressão de perfusão e redução da viscosidade sanguínea, exacerbando assim o sangramento.[121]Roberts K, Revell M, Youssef H, et al. Hypotensive resuscitation in patients with ruptured abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2006 Apr;31(4):339-44. http://www.ncbi.nlm.nih.gov/pubmed/16388972?tool=bestpractice.com [122]Ohki T, Veith FJ. Endovascular grafts and other image-guided catheter-based adjuncts to improve the treatment of ruptured aortoiliac aneurysms. Ann Surg. 2000 Oct;232(4):466-79. http://www.ncbi.nlm.nih.gov/pubmed/10998645?tool=bestpractice.com Recomenda-se tentar alcançar pressão arterial sistólica (PAS) de 50 a 70 mmHg e supressão de fluidos no pré-operatório.[121]Roberts K, Revell M, Youssef H, et al. Hypotensive resuscitation in patients with ruptured abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2006 Apr;31(4):339-44. http://www.ncbi.nlm.nih.gov/pubmed/16388972?tool=bestpractice.com [122]Ohki T, Veith FJ. Endovascular grafts and other image-guided catheter-based adjuncts to improve the treatment of ruptured aortoiliac aneurysms. Ann Surg. 2000 Oct;232(4):466-79. http://www.ncbi.nlm.nih.gov/pubmed/10998645?tool=bestpractice.com As diretrizes do American College of Cardiology/American Heart Association (ACC/AHA) recomendam a hipotensão permissiva para reduzir o sangramento.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com No entanto, as metas recomendadas variam, e não há consenso entre os grupos de diretrizes globais.
Como inserir um tubo traqueal em adulto usando um laringoscópio.
Como usar um aparato reanimador manual autoinflável para fornecer suporte ventilatório a adultos. Vídeo de demonstração da técnica de duas pessoas.
reparo cirúrgico urgente
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
O American College of Cardiology/American Heart Association (ACC/AHA) recomendam a tomografia computadorizada (TC) em pacientes que apresentam AAA roto e estão hemodinamicamente estáveis para avaliar se o AAA é passível de reparo endovascular.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com Essa recomendação tem o suporte dos resultados do ensaio clínico randomizado e controlado multicêntrico IMPROVE, que sugere que, para a maioria dos pacientes, a TC confirmatória não causou atrasos significativos ao tratamento e facilitou o planejamento pré-operatório adequado.[110]Powell JT, Hinchcliffe RJ, Thompson MM, et al; IMPROVE Trial Investigators. Observations from the IMPROVE trial concerning the clinical care of patients with ruptured abdominal aortic aneurysm. Br J Surg. 2014 Feb;101(3):216-24. https://bjssjournals.onlinelibrary.wiley.com/doi/full/10.1002/bjs.9410 http://www.ncbi.nlm.nih.gov/pubmed/24469620?tool=bestpractice.com
Se a anatomia for adequada, o ACC/AHA recomendam o reparo endovascular em vez do reparo por via aberta para reduzir o risco de morbidade e mortalidade.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com Em pacientes com AAA roto confirmado, a mortalidade em 3 anos foi menor entre aqueles randomizados para reparo de aneurisma endovascular (EVAR) do que em uma estratégia de reparo aberto (48% vs. 56%; razão de riscos de 0.57, IC de 95% 0.36 a 0.90).[111]IMPROVE Trial Investigators. Comparative clinical effectiveness and cost effectiveness of endovascular strategy v open repair for ruptured abdominal aortic aneurysm: three year results of the IMPROVE randomised trial. BMJ. 2017 Nov 14;359:j4859. https://www.bmj.com/content/359/bmj.j4859.long http://www.ncbi.nlm.nih.gov/pubmed/29138135?tool=bestpractice.com A diferença entre os grupos de tratamento não foi mais evidente após 7 anos de acompanhamento (razão de riscos de 0.92, IC de 95% 0.75 a 1.13). As taxas de nova intervenção não foram significativamente diferentes entre os grupos randomizados em 3 anos (razão de riscos de 1.02, IC de 95% 0.79 a 1.32).[111]IMPROVE Trial Investigators. Comparative clinical effectiveness and cost effectiveness of endovascular strategy v open repair for ruptured abdominal aortic aneurysm: three year results of the IMPROVE randomised trial. BMJ. 2017 Nov 14;359:j4859. https://www.bmj.com/content/359/bmj.j4859.long http://www.ncbi.nlm.nih.gov/pubmed/29138135?tool=bestpractice.com Existem algumas evidências que sugerem que a estratégia endovascular para reparo do AAA roto pode reduzir a mortalidade mais efetivamente em mulheres do que em homens.[111]IMPROVE Trial Investigators. Comparative clinical effectiveness and cost effectiveness of endovascular strategy v open repair for ruptured abdominal aortic aneurysm: three year results of the IMPROVE randomised trial. BMJ. 2017 Nov 14;359:j4859. https://www.bmj.com/content/359/bmj.j4859.long http://www.ncbi.nlm.nih.gov/pubmed/29138135?tool=bestpractice.com [112]Sweeting MJ, Balm R, Desgranges P, et al; Ruptured Aneurysm Trialists. Individual-patient meta-analysis of three randomized trials comparing endovascular versus open repair for ruptured abdominal aortic aneurysm. Br J Surg. 2015 Sep;102(10):1229-39. https://bjssjournals.onlinelibrary.wiley.com/doi/full/10.1002/bjs.9852 http://www.ncbi.nlm.nih.gov/pubmed/26104471?tool=bestpractice.com
Há evidências que sugerem que o modo de anestesia para reparo cirúrgico do AAA afeta os desfechos.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [113]Armstrong RA, Squire YG, Rogers CA, et al. Type of anesthesia for endovascular abdominal aortic aneurysm repair. J Cardiothorac Vasc Anesth. 2019 Feb;33(2):462-71. http://www.ncbi.nlm.nih.gov/pubmed/30342821?tool=bestpractice.com Em 2024, a European Society for Vascular Surgery (ESVS) emitiu uma recomendação fraca favorecendo a anestesia local em vez da anestesia geral em cenários eletivos, com base na potencial redução no tempo do procedimento, internações na UTI e permanência hospitalar pós-operatória.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [114]Liu Y, Wang T, Zhao J, et al. Influence of anesthetic techniques on perioperative outcomes after endovascular aneurysm repair. Ann Vasc Surg. 2021 May;73:375-84. http://www.ncbi.nlm.nih.gov/pubmed/33383135?tool=bestpractice.com [115]Zottola ZR, Kruger JL, Kong DS, et al. Locoregional anesthesia is associated with reduced hospital stay and need for intensive care unit care of elective endovascular aneurysm repair patients in the Vascular Quality Initiative. J Vasc Surg. 2023 Apr;77(4):1061-9. https://www.jvascsurg.org/article/S0741-5214(22)02534-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/36400363?tool=bestpractice.com [116]Kothandan H, Haw Chieh GL, Khan SA, et al. Anesthetic considerations for endovascular abdominal aortic aneurysm repair. Ann Card Anaesth. 2016 Jan-Mar;19(1):132-41. https://pmc.ncbi.nlm.nih.gov/articles/PMC4900395 http://www.ncbi.nlm.nih.gov/pubmed/26750684?tool=bestpractice.com O ensaio clínico randomizado e controlado multicêntrico IMPROVE detectou uma mortalidade em 30 dias consideravelmente reduzida em pacientes que realizaram reparo endovascular (EVAR) com anestesia local isolada, em comparação com a anestesia geral (RC ajustada de 0.27, 0.1 a 0.7).[110]Powell JT, Hinchcliffe RJ, Thompson MM, et al; IMPROVE Trial Investigators. Observations from the IMPROVE trial concerning the clinical care of patients with ruptured abdominal aortic aneurysm. Br J Surg. 2014 Feb;101(3):216-24. https://bjssjournals.onlinelibrary.wiley.com/doi/full/10.1002/bjs.9410 http://www.ncbi.nlm.nih.gov/pubmed/24469620?tool=bestpractice.com Uma metanálise separada que comparou o modo de anestesia para o reparo endovascular de AAA roto replicou esses achados ou melhorou os desfechos com EVAR com anestesia local.[117]Harky A, Ahmad MU, Santoro G, et al. Local versus general anesthesia in nonemergency endovascular abdominal aortic aneurysm repair: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2020 Apr;34(4):1051-9. http://www.ncbi.nlm.nih.gov/pubmed/31473112?tool=bestpractice.com No entanto, outra revisão sistemática não mostrou nenhum benefício de mortalidade com a anestesia local, mas demonstrou menor tempo de internação hospitalar.[118]Deng J, Liu J, Rong D, et al. A meta-analysis of locoregional anesthesia versus general anesthesia in endovascular repair of ruptured abdominal aortic aneurysm. J Vasc Surg. 2021 Feb;73(2):700-10. https://www.doi.org/10.1016/j.jvs.2020.08.112 http://www.ncbi.nlm.nih.gov/pubmed/32882348?tool=bestpractice.com Dados do Registro Vascular Nacional do Reino Unido (9783 pacientes que receberam um EVAR infrarrenal padrão eletivo; anestesia geral, n = 7069; anestesia regional, n = 2347; anestesia local, n = 367) mostraram uma menor taxa de mortalidade em 30 dias após anestesia regional em comparação à anestesia geral.[119]Dovell G, Rogers CA, Armstrong R, et al. The effect of mode of anaesthesia on outcomes after elective endovascular repair of abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2020 May;59(5):729-38. https://www.ejves.com/article/S1078-5884(20)30118-0/fulltext http://www.ncbi.nlm.nih.gov/pubmed/32291124?tool=bestpractice.com O estudo multicêntrico internacional Endurant Stent Graft Natural Selection Global Post-Market Registry (ENGAGE) examinou os desfechos de 1231 pacientes submetidos a EVAR sob anestesia geral (62% dos pacientes), regional (27%) e local (11%).[120]Broos PP, Stokmans RA, Cuypers PW, et al. Effects of anesthesia type on perioperative outcome after endovascular aneurysm repair. J Endovasc Ther. 2015 Oct;22(5):770-7. http://www.ncbi.nlm.nih.gov/pubmed/26276553?tool=bestpractice.com O tipo de anestesia não teve influência na mortalidade ou morbidade perioperatória, mas o uso de anestesia local ou regional durante o EVAR pareceu ser benéfico na redução do tempo do procedimento, da necessidade de internação na UTI e da duração da permanência hospitalar pós-operatória.[120]Broos PP, Stokmans RA, Cuypers PW, et al. Effects of anesthesia type on perioperative outcome after endovascular aneurysm repair. J Endovasc Ther. 2015 Oct;22(5):770-7. http://www.ncbi.nlm.nih.gov/pubmed/26276553?tool=bestpractice.com
antibioticoterapia perioperatória
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
A antibioticoterapia é indicada para pacientes submetidos a um reparo de emergência de AAA roto para tratamento contra organismos Gram-positivos e Gram-negativos (ou seja, Staphylococcus aureus, Staphylococcus epidermidis e bacilos Gram-negativos entéricos), bem como para evitar a infecção do enxerto.
O tratamento com antibióticos de amplo espectro é adaptado ao quadro clínico do paciente e culturas, e de acordo com os protocolos locais.
tratamento das causas infecciosas/inflamatórias
Tratamento adicional recomendado para ALGUNS pacientes no grupo de pacientes selecionado
Quando o paciente estiver estável e o reparo cirúrgico urgente para a ruptura tiver sido priorizado, a etiologia infecciosa ou inflamatória deve ser abordada.
Se houver suspeita de aneurisma infeccioso no paciente, o diagnóstico precoce e o tratamento imediato são essenciais para aprimorar os desfechos.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com Muitas vezes, o desbridamento extensivo é necessário durante o reparo cirúrgico urgente nesses pacientes. Há alto risco de complicações infecciosas secundárias, e uma cirurgia adicional pode ser necessária para novas lesões infecciosas. Culturas intraoperatórias devem ser realizadas para orientar de maneira precisa a antibioticoterapia subsequente; no entanto, muitas vezes são administrados antibióticos empíricos, pois hemoculturas periféricas e culturas de amostras cirúrgicas são negativas em uma grande proporção de pacientes.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A antibioticoterapia prolongada (de 4-6 semanas de duração até a vida toda) pode ser indicada, dependendo do patógeno específico, do tipo de reparo operatório e do estado imunológico do paciente[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
A aortite inflamatória (causada, por exemplo, por arterite de Takayasu ou arterite de células gigantes) é tratada com corticosteroide em altas doses e cirurgia.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [205]Ben Jmaà H, Karray R, Jmal H, et al. Surgical and endoluminal management of the inflammatory aortitis: a Tunisian center experience [in French]. J Med Vasc. 2017 Jul;42(4):213-20. http://www.ncbi.nlm.nih.gov/pubmed/28705339?tool=bestpractice.com
aneurisma da aorta abdominal (AAA) sintomático não roto
reparo cirúrgico urgente
Em pacientes com aneurisma da aorta sintomático, o reparo urgente é indicado independente do diâmetro.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [78]National Institute for Health and Care Excellence. Abdominal aortic aneurysm: diagnosis and management. Mar 2020 [internet publication]. https://www.nice.org.uk/guidance/ng156 [127]Mazzolai L, Teixido-Tura G, Lanzi S, et al; ESC Committee for Practice Guidelines. 2024 ESC guidelines for the management of peripheral arterial and aortic diseases. Eur Heart J. 2024 Sep 29;45(36):3538-700. https://academic.oup.com/eurheartj/article/45/36/3538/7738955 O desenvolvimento de dor nova ou o agravamento da dor pode sinalizar expansão do aneurisma e ruptura iminente. É melhor, portanto, tratar com urgência o aneurisma sintomático não roto.[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2. https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com Em algumas circunstâncias, a intervenção pode ser protelada por várias horas para otimizar as condições e garantir o sucesso do reparo; estes pacientes devem ser monitorados de perto na unidade de terapia intensiva.[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2. https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com
O reparo endovascular do aneurisma (EVAR) é cada vez mais usado no tratamento de pacientes com AAA sintomático.[128]De Martino RR, Nolan BW, Goodney PP, Chang CK, et al; Vascular Study Group of Northern New England. Outcomes of symptomatic abdominal aortic aneurysm repair. J Vasc Surg. 2010 Jul;52(1):5-12.e1. https://www.jvascsurg.org/article/S0741-5214(10)00259-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/20471771?tool=bestpractice.com [129]Chandra V, Trang K, Virgin-Downey W, et al. Management and outcomes of symptomatic abdominal aortic aneurysms during the past 20 years. J Vasc Surg. 2017 Dec;66(6):1679-85. http://www.ncbi.nlm.nih.gov/pubmed/28619644?tool=bestpractice.com Em estudos observacionais, as taxas de mortalidade a curto prazo por todas as causas não diferiu entre o reparo endovascular e aberto do AAA sintomático.[128]De Martino RR, Nolan BW, Goodney PP, Chang CK, et al; Vascular Study Group of Northern New England. Outcomes of symptomatic abdominal aortic aneurysm repair. J Vasc Surg. 2010 Jul;52(1):5-12.e1. https://www.jvascsurg.org/article/S0741-5214(10)00259-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/20471771?tool=bestpractice.com [129]Chandra V, Trang K, Virgin-Downey W, et al. Management and outcomes of symptomatic abdominal aortic aneurysms during the past 20 years. J Vasc Surg. 2017 Dec;66(6):1679-85. http://www.ncbi.nlm.nih.gov/pubmed/28619644?tool=bestpractice.com [130]Ten Bosch JA, Willigendael EM, Kruidenier LM, et al. Early and mid-term results of a prospective observational study comparing emergency endovascular aneurysm repair with open surgery in both ruptured and unruptured acute abdominal aortic aneurysms. Vascular. 2012 Apr;20(2):72-80. http://www.ncbi.nlm.nih.gov/pubmed/22454547?tool=bestpractice.com
redução do risco cardiovascular pré-operatório
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
O controle dos fatores de risco cardiovascular modificáveis no pré-operatório melhora a sobrevida de longo prazo após o reparo do AAA.[196]Khashram M, Williman JA, Hider PN, et al. Management of modifiable vascular risk factors improves late survival following abdominal aortic aneurysm repair: a systematic review and meta-analysis. Ann Vasc Surg. 2017 Feb;39:301-11. http://www.ncbi.nlm.nih.gov/pubmed/27666804?tool=bestpractice.com
O treinamento pré-operatório reduziu as complicações cardíacas pós-cirúrgicas em um pequeno ensaio clínico randomizado e controlado (ECRC) com pacientes submetidos a reparo de AAA aberto ou endovascular, embora uma revisão Cochrane e uma revisão sistemática separada de pré-reabilitação (exercícios) antes da cirurgia de AAA não tenham mostrado nenhum benefício em relação ao desfecho.[197]Barakat HM, Shahin Y, Khan JA, et al. Preoperative supervised exercise improves outcomes after elective abdominal aortic aneurysm repair: a randomized controlled trial. Ann Surg. 2016 Jul;264(1):47-53. http://www.ncbi.nlm.nih.gov/pubmed/26756766?tool=bestpractice.com [198]Fenton C, Tan AR, Abaraogu UO, et al. Prehabilitation exercise therapy before elective abdominal aortic aneurysm repair. Cochrane Database Syst Rev. 2021 Jul 8;7(7):CD013662. https://www.doi.org/10.1002/14651858.CD013662.pub2 http://www.ncbi.nlm.nih.gov/pubmed/34236703?tool=bestpractice.com [199]Bonner RJ, Wallace T, Jones AD, et al. The content of pre-habilitative interventions for patients undergoing repair of abdominal aortic aneurysms and their effect on post-operative outcomes: a systematic review. Eur J Vasc Endovasc Surg. 2021 May;61(5):756-65. https://www.doi.org/10.1016/j.ejvs.2021.01.043 http://www.ncbi.nlm.nih.gov/pubmed/33678532?tool=bestpractice.com Embora a prática de exercícios pré-operatórios possa ser benéfica para pacientes submetidos ao reparo de AAA, são necessárias investigações adicionais com ECRCs antes que possa ser recomendada mais amplamente.[200]Wee IJY, Choong AMTL. A systematic review of the impact of preoperative exercise for patients with abdominal aortic aneurysm. J Vasc Surg. 2020 Jun;71(6):2123-31.e1. https://www.doi.org/10.1016/j.jvs.2018.09.039 http://www.ncbi.nlm.nih.gov/pubmed/30606665?tool=bestpractice.com
O uso de estatina perioperatória desacelera o crescimento do aneurisma, reduz o risco de ruptura e diminui a mortalidade por reparo de AAA ou AAA roto.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A administração de estatinas deve ser iniciada pelo menos 1 mês antes da cirurgia, para reduzir a morbidade e a mortalidade cardiovascular, e deve ser mantida indefinidamente.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [141]Risum Ø, Sandven I, Sundhagen JO, et al. Editor's choice - effect of statins on total mortality in abdominal aortic aneurysm repair: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2021 Jan;61(1):114-20. https://www.doi.org/10.1016/j.ejvs.2020.08.007 http://www.ncbi.nlm.nih.gov/pubmed/32928667?tool=bestpractice.com
Pacientes com AAAs apresentam aumento do risco de eventos cardiovasculares adversos importantes. As evidências são limitadas, mas, na ausência de contraindicações, os pacientes com AAA devem receber terapia antiagregante plaquetária única (aspirina ou clopidogrel).[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [142]Aboyans V, Bauersachs R, Mazzolai L, et al. Antithrombotic therapies in aortic and peripheral arterial diseases in 2021: a consensus document from the ESC working group on aorta and peripheral vascular diseases, the ESC working group on thrombosis, and the ESC working group on cardiovascular pharmacotherapy. Eur Heart J. 2021 Oct 14;42(39):4013-24. https://www.doi.org/10.1093/eurheartj/ehab390 http://www.ncbi.nlm.nih.gov/pubmed/34279602?tool=bestpractice.com Isso deve ser mantido durante o período perioperatório.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
Deve-se controlar a hipertensão para reduzir a morbidade e a mortalidade cardiovascular.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
Não é recomendado o início do uso de betabloqueadores antes do reparo do AAA.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com No entanto, um betabloqueador pode ser mantido se o paciente já estiver tomando-o em uma dose apropriada.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com Grandes estudos em que betabloqueadores foram iniciados alguns dias antes da cirurgia indicaram ausência de benefício, ou mesmo prejuízo, do betabloqueio perioperatório.[201]Brady AR, Gibbs JS, Greenhalgh RM, et al; POBBLE Trial Investigators. Perioperative beta-blockade (Pobble) for patients undergoing infrarenal vascular surgery: results of a randomized double-blind controlled trial. J Vasc Surg. 2005 Apr;41(4):602-9. https://www.jvascsurg.org/article/S0741-5214(05)00189-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/15874923?tool=bestpractice.com [202]Devereaux PJ, Yang H, Yusuf S, et al; POISE Study Group. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008 May 31;371(9627):1839-47. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)60601-7/fulltext http://www.ncbi.nlm.nih.gov/pubmed/18479744?tool=bestpractice.com [203]Yang H, Raymer K, Butler R, et al. The effects of perioperative beta-blockade: results of the Metoprolol after Vascular Surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006 Nov;152(5):983-90. http://www.ncbi.nlm.nih.gov/pubmed/17070177?tool=bestpractice.com
antibioticoterapia perioperatória
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
Antibioticoterapia perioperatória é administrada. O tratamento com antibióticos de amplo espectro é necessário, de acordo com os protocolos locais.
tratamento das causas infecciosas/inflamatórias
Tratamento adicional recomendado para ALGUNS pacientes no grupo de pacientes selecionado
Quando o paciente estiver estável e o reparo cirúrgico urgente para AAA sintomático tiver sido priorizado, a etiologia infecciosa ou inflamatória deve ser abordada.
Se houver suspeita de aneurisma infeccioso no paciente, o diagnóstico precoce e o tratamento imediato são essenciais para aprimorar os desfechos.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com Muitas vezes, o desbridamento extensivo é necessário durante o reparo cirúrgico urgente nesses pacientes. Há alto risco de complicações infecciosas secundárias, e uma cirurgia adicional pode ser necessária para novas lesões infecciosas. Culturas intraoperatórias devem ser realizadas para orientar de maneira precisa a antibioticoterapia subsequente; no entanto, muitas vezes são administrados antibióticos empíricos, pois hemoculturas periféricas e culturas de amostras cirúrgicas são negativas em uma grande proporção de pacientes.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A antibioticoterapia prolongada (de 4-6 semanas de duração até a vida toda) pode ser indicada, dependendo do patógeno específico, do tipo de reparo operatório e do estado imunológico do paciente[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
A aortite inflamatória (causada, por exemplo, por arterite de Takayasu ou arterite de células gigantes) é tratada com corticosteroide em altas doses e cirurgia.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [205]Ben Jmaà H, Karray R, Jmal H, et al. Surgical and endoluminal management of the inflammatory aortitis: a Tunisian center experience [in French]. J Med Vasc. 2017 Jul;42(4):213-20. http://www.ncbi.nlm.nih.gov/pubmed/28705339?tool=bestpractice.com
achado incidental: AAA assintomático pequeno
vigilância
Quando o aneurisma da aorta abdominal (AAA) é detectado como um achado incidental, deve-se dar preferência à vigilância em relação ao reparo até que o risco teórico de ruptura seja superior ao risco estimado de mortalidade operatória.[4]Owens DK, Davidson KW, Krist AH, et al; US Preventive Services Task Force. Screening for abdominal aortic aneurysm: US Preventive Services Task Force recommendation statement. JAMA. 2019 Dec 10;322(22):2211-8. https://jamanetwork.com/journals/jama/fullarticle/2757234 http://www.ncbi.nlm.nih.gov/pubmed/31821437?tool=bestpractice.com
A cirurgia aberta precoce para o tratamento de AAAs menores não reduz a mortalidade por todas as causas ou específica do AAA.[4]Owens DK, Davidson KW, Krist AH, et al; US Preventive Services Task Force. Screening for abdominal aortic aneurysm: US Preventive Services Task Force recommendation statement. JAMA. 2019 Dec 10;322(22):2211-8.
https://jamanetwork.com/journals/jama/fullarticle/2757234
http://www.ncbi.nlm.nih.gov/pubmed/31821437?tool=bestpractice.com
[132]Ulug P, Powell JT, Martinez MA, et al. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2020 Jul 1;7(7):CD001835.
https://www.doi.org/10.1002/14651858.CD001835.pub5
http://www.ncbi.nlm.nih.gov/pubmed/32609382?tool=bestpractice.com
[  ]
How does immediate surgery compare with surveillance in people with asymptomatic abdominal aortic aneurysms (AAAs)?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.3227/fullMostre-me a resposta Uma revisão sistemática (4 estudos, 3314 participantes) encontrou evidências de alta qualidade para demonstrar que o reparo imediato de aneurisma da aorta abdominal pequeno (4.0 cm a 5.5 cm) não melhorou a sobrevida em longo prazo em comparação com a vigilância (razão de riscos ajustada de 0.88; IC de 95% 0.75 a 1.02, acompanhamento médio de 10 anos).[132]Ulug P, Powell JT, Martinez MA, et al. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2020 Jul 1;7(7):CD001835.
https://www.doi.org/10.1002/14651858.CD001835.pub5
http://www.ncbi.nlm.nih.gov/pubmed/32609382?tool=bestpractice.com
A falta de benefício atribuível à cirurgia imediata foi consistente independentemente da idade do paciente, diâmetro do aneurisma pequeno e se o reparo foi endovascular ou aberto.[132]Ulug P, Powell JT, Martinez MA, et al. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2020 Jul 1;7(7):CD001835.
https://www.doi.org/10.1002/14651858.CD001835.pub5
http://www.ncbi.nlm.nih.gov/pubmed/32609382?tool=bestpractice.com
]
How does immediate surgery compare with surveillance in people with asymptomatic abdominal aortic aneurysms (AAAs)?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.3227/fullMostre-me a resposta Uma revisão sistemática (4 estudos, 3314 participantes) encontrou evidências de alta qualidade para demonstrar que o reparo imediato de aneurisma da aorta abdominal pequeno (4.0 cm a 5.5 cm) não melhorou a sobrevida em longo prazo em comparação com a vigilância (razão de riscos ajustada de 0.88; IC de 95% 0.75 a 1.02, acompanhamento médio de 10 anos).[132]Ulug P, Powell JT, Martinez MA, et al. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2020 Jul 1;7(7):CD001835.
https://www.doi.org/10.1002/14651858.CD001835.pub5
http://www.ncbi.nlm.nih.gov/pubmed/32609382?tool=bestpractice.com
A falta de benefício atribuível à cirurgia imediata foi consistente independentemente da idade do paciente, diâmetro do aneurisma pequeno e se o reparo foi endovascular ou aberto.[132]Ulug P, Powell JT, Martinez MA, et al. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2020 Jul 1;7(7):CD001835.
https://www.doi.org/10.1002/14651858.CD001835.pub5
http://www.ncbi.nlm.nih.gov/pubmed/32609382?tool=bestpractice.com
O encaminhamento cirúrgico do AAA menor é geralmente reservado para crescimento rápido, ou uma vez que o diâmetro limiar para o reparo do aneurisma é atingido por ultrassonografia repetida.[4]Owens DK, Davidson KW, Krist AH, et al; US Preventive Services Task Force. Screening for abdominal aortic aneurysm: US Preventive Services Task Force recommendation statement. JAMA. 2019 Dec 10;322(22):2211-8. https://jamanetwork.com/journals/jama/fullarticle/2757234 http://www.ncbi.nlm.nih.gov/pubmed/31821437?tool=bestpractice.com
Entretanto, em pacientes com uma causa genética subjacente ou doenças do tecido conjuntivo, o diâmetro limite para considerar o reparo deve ser individualizado, dependendo das características anatômicas e da genética subjacente (o risco de ruptura é maior em diâmetros aórticos menores em algumas condições, e o reparo cirúrgico é mais desafiador em certas doenças devido a maior fragilidade e anatomia da parede arterial).[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
manejo agressivo de risco cardiovascular
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
O controle dos fatores de risco cardiovascular modificáveis no pré-operatório melhora a sobrevida de longo prazo após o reparo do AAA.[196]Khashram M, Williman JA, Hider PN, et al. Management of modifiable vascular risk factors improves late survival following abdominal aortic aneurysm repair: a systematic review and meta-analysis. Ann Vasc Surg. 2017 Feb;39:301-11. http://www.ncbi.nlm.nih.gov/pubmed/27666804?tool=bestpractice.com
Os pacientes devem ser incentivados a parar com o tabagismo e receber terapia medicamentosa (terapia de reposição de nicotina, nortriptilina e bupropiona) ou aconselhamento para ajudar, caso seja necessário.[1]Dehlin JM, Upchurch GR. Management of abdominal aortic aneurysms. Curr Treat Options Cardiovasc Med. 2005 Jun;7(2):119-30.
http://www.ncbi.nlm.nih.gov/pubmed/15935120?tool=bestpractice.com
[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482.
https://www.doi.org/10.1161/CIR.0000000000001106
http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
[13]Zankl AR, Schumacher H, Krumsdorf U, et al. Pathology, natural history and treatment of abdominal aortic aneurysms. Clin Res Cardiol. 2007 Mar;96(3):140-51.
http://www.ncbi.nlm.nih.gov/pubmed/17180573?tool=bestpractice.com
[15]Singh K, Bønaa H, Jacobsen BK, et al. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: the Tromsø Study. Am J Epidemiol. 2001 Aug 1;154(3):236-44.
https://academic.oup.com/aje/article/154/3/236/125840
http://www.ncbi.nlm.nih.gov/pubmed/11479188?tool=bestpractice.com
[22]Lederle FA, Johnson GR, Wilson SE, et al; Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative Study Group. Prevalence and associations of abdominal aortic aneurysm detected through screening. Ann Intern Med. 1997 Mar 15;126(6):441-9.
http://www.ncbi.nlm.nih.gov/pubmed/9072929?tool=bestpractice.com
[23]Wilmink TB, Quick CR, Day NE. The association between cigarette smoking and abdominal aortic aneurysms. J Vasc Surg. 1999 Dec;30(6):1099-105.
http://www.ncbi.nlm.nih.gov/pubmed/10587395?tool=bestpractice.com
[136]Hartmann-Boyce J, Chepkin SC, Ye W, et al. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst Rev. 2018 May 31;5:CD000146.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000146.pub5/full
http://www.ncbi.nlm.nih.gov/pubmed/29852054?tool=bestpractice.com
[137]Rigotti NA, Clair C, Munafò MR, et al. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2012 May 16;(5):CD001837.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001837.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/22592676?tool=bestpractice.com
[138]Howes S, Hartmann-Boyce J, Livingstone-Banks J, et al. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2020 Apr 22;(4):CD000031.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000031.pub5/full
http://www.ncbi.nlm.nih.gov/pubmed/32319681?tool=bestpractice.com
[  ]
What are the effects of adding bupropion or fluoxetine to other treatments compared with using other treatments alone for people trying to quit smoking?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.4337/fullMostre-me a resposta
]
What are the effects of adding bupropion or fluoxetine to other treatments compared with using other treatments alone for people trying to quit smoking?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.4337/fullMostre-me a resposta
O treinamento pré-operatório reduziu as complicações cardíacas pós-cirúrgicas em um pequeno ensaio clínico randomizado e controlado (ECRC) com pacientes submetidos a reparo de AAA aberto ou endovascular, embora uma revisão Cochrane e uma revisão sistemática separada de pré-reabilitação (exercícios) antes da cirurgia de AAA não tenham mostrado nenhum benefício em relação ao desfecho.[197]Barakat HM, Shahin Y, Khan JA, et al. Preoperative supervised exercise improves outcomes after elective abdominal aortic aneurysm repair: a randomized controlled trial. Ann Surg. 2016 Jul;264(1):47-53. http://www.ncbi.nlm.nih.gov/pubmed/26756766?tool=bestpractice.com [198]Fenton C, Tan AR, Abaraogu UO, et al. Prehabilitation exercise therapy before elective abdominal aortic aneurysm repair. Cochrane Database Syst Rev. 2021 Jul 8;7(7):CD013662. https://www.doi.org/10.1002/14651858.CD013662.pub2 http://www.ncbi.nlm.nih.gov/pubmed/34236703?tool=bestpractice.com [199]Bonner RJ, Wallace T, Jones AD, et al. The content of pre-habilitative interventions for patients undergoing repair of abdominal aortic aneurysms and their effect on post-operative outcomes: a systematic review. Eur J Vasc Endovasc Surg. 2021 May;61(5):756-65. https://www.doi.org/10.1016/j.ejvs.2021.01.043 http://www.ncbi.nlm.nih.gov/pubmed/33678532?tool=bestpractice.com Embora a prática de exercícios pré-operatórios possa ser benéfica para pacientes submetidos ao reparo de AAA, são necessárias investigações adicionais com ECRCs antes que possa ser recomendada mais amplamente.[200]Wee IJY, Choong AMTL. A systematic review of the impact of preoperative exercise for patients with abdominal aortic aneurysm. J Vasc Surg. 2020 Jun;71(6):2123-31.e1. https://www.doi.org/10.1016/j.jvs.2018.09.039 http://www.ncbi.nlm.nih.gov/pubmed/30606665?tool=bestpractice.com
O uso de estatina perioperatória desacelera o crescimento do aneurisma, reduz o risco de ruptura e diminui a mortalidade por reparo de AAA ou AAA roto.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A administração de estatinas deve ser iniciada pelo menos 1 mês antes da cirurgia, para reduzir a morbidade e a mortalidade cardiovascular, e deve ser mantida indefinidamente.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [141]Risum Ø, Sandven I, Sundhagen JO, et al. Editor's choice - effect of statins on total mortality in abdominal aortic aneurysm repair: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2021 Jan;61(1):114-20. https://www.doi.org/10.1016/j.ejvs.2020.08.007 http://www.ncbi.nlm.nih.gov/pubmed/32928667?tool=bestpractice.com
Pacientes com AAAs apresentam aumento do risco de eventos cardiovasculares adversos importantes. As evidências são limitadas, mas, na ausência de contraindicações, os pacientes com AAA devem receber terapia antiagregante plaquetária única (aspirina ou clopidogrel).[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [142]Aboyans V, Bauersachs R, Mazzolai L, et al. Antithrombotic therapies in aortic and peripheral arterial diseases in 2021: a consensus document from the ESC working group on aorta and peripheral vascular diseases, the ESC working group on thrombosis, and the ESC working group on cardiovascular pharmacotherapy. Eur Heart J. 2021 Oct 14;42(39):4013-24. https://www.doi.org/10.1093/eurheartj/ehab390 http://www.ncbi.nlm.nih.gov/pubmed/34279602?tool=bestpractice.com Isso deve ser mantido durante o período perioperatório.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
Deve-se controlar a hipertensão para reduzir a morbidade e a mortalidade cardiovascular.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
tratamento das causas infecciosas/inflamatórias
Tratamento adicional recomendado para ALGUNS pacientes no grupo de pacientes selecionado
A etiologia infecciosa ou inflamatória deve ser abordada.
Se houver suspeita de aneurisma infeccioso no paciente, o diagnóstico precoce, o tratamento imediato com antibióticos e o reparo cirúrgico urgente são essenciais para aprimorar os desfechos.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com Muitas vezes, o desbridamento extensivo é necessário durante o reparo cirúrgico urgente nesses pacientes. Há alto risco de complicações infecciosas secundárias, e uma cirurgia adicional pode ser necessária para novas lesões infecciosas. Culturas intraoperatórias devem ser realizadas para orientar de maneira precisa a antibioticoterapia subsequente; no entanto, muitas vezes são administrados antibióticos empíricos, pois hemoculturas periféricas e culturas de amostras cirúrgicas são negativas em uma grande proporção de pacientes.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A antibioticoterapia prolongada (de 4-6 semanas de duração até a vida toda) pode ser indicada, dependendo do patógeno específico, do tipo de reparo operatório e do estado imunológico do paciente[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
A aortite inflamatória (causada, por exemplo, por arterite de Takayasu ou arterite de células gigantes) é tratada com corticosteroide em altas doses e cirurgia.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [205]Ben Jmaà H, Karray R, Jmal H, et al. Surgical and endoluminal management of the inflammatory aortitis: a Tunisian center experience [in French]. J Med Vasc. 2017 Jul;42(4):213-20. http://www.ncbi.nlm.nih.gov/pubmed/28705339?tool=bestpractice.com
achado incidental: AAA grande assintomático
reparo cirúrgico eletivo
Em geral, o reparo é indicado para os pacientes com aneurisma da aorta abdominal assintomático grande (por exemplo, com um diâmetro superior a 5.5 cm em homens ou 5.0 cm em mulheres nos EUA, embora as decisões de tratamento baseadas no maior tamanho possam diferir em outros países).[78]National Institute for Health and Care Excellence. Abdominal aortic aneurysm: diagnosis and management. Mar 2020 [internet publication]. https://www.nice.org.uk/guidance/ng156 O reparo de aneurismas ≥5.5 cm oferece uma vantagem de sobrevivência.[1]Dehlin JM, Upchurch GR. Management of abdominal aortic aneurysms. Curr Treat Options Cardiovasc Med. 2005 Jun;7(2):119-30. http://www.ncbi.nlm.nih.gov/pubmed/15935120?tool=bestpractice.com [76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2. https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com [106]UK Small Aneurysm Trial Participants. Mortality results for randomized controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. Lancet. 1998 Nov 21;352(9141):1649-55. http://www.ncbi.nlm.nih.gov/pubmed/9853436?tool=bestpractice.com [107]Powell JT, Brady AR, Brown LC, et al; United Kingdom Small Aneurysm Trial Participants. Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med. 2002 May 9;346(19):1445-52. https://www.nejm.org/doi/full/10.1056/NEJMoa013527 http://www.ncbi.nlm.nih.gov/pubmed/12000814?tool=bestpractice.com [108]Powell JT, Brown LC, Forbes JF, et al. Final 12-year follow-up of surgery versus surveillance in the UK Small Aneurysm Trial. Br J Surg. 2007 Jun;94(6):702-8. http://www.ncbi.nlm.nih.gov/pubmed/17514693?tool=bestpractice.com
As decisões quanto ao reparo devem ser individualizadas, tendo em conta a preferência, idade, sexo, fatores de risco perioperatórios e anatômicos de risco do paciente. Deve-se ter cautela ao avaliar a qualidade de vida do paciente, com orientação cuidadosa sobre os riscos da cirurgia e subsequente qualidade de vida. Recomenda-se uma abordagem de tomada de decisão compartilhada, que leve em consideração os riscos e benefícios dos procedimentos.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [132]Ulug P, Powell JT, Martinez MA, et al. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2020 Jul 1;7(7):CD001835. https://www.doi.org/10.1002/14651858.CD001835.pub5 http://www.ncbi.nlm.nih.gov/pubmed/32609382?tool=bestpractice.com
Dados sugerem que, em pacientes com AAAs extensos (≥5.5 cm) submetidos ao reparo eletivo, o EVAR é equivalente ao reparo aberto em termos de sobrevida global, embora a taxa de intervenções secundárias seja maior para o EVAR.[143]Greenhalgh RM, Brown LC, Powell JT, et al; United Kingdom EVAR Trial Investigators. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010 May 20;362(20):1863-71. http://www.ncbi.nlm.nih.gov/pubmed/20382983?tool=bestpractice.com [144]Amato B, Fugetto F, Compagna R, et al. Endovascular repair versus open repair in the treatment of ruptured aortic aneurysms: a systematic review. Minerva Chir. 2019 Dec;74(6):472-80. http://www.ncbi.nlm.nih.gov/pubmed/29806754?tool=bestpractice.com O EVAR reduz a mortalidade relacionada com o AAA (mas não a sobrevida global a longo prazo) em pacientes com AAA extenso (≥5.5 cm) não elegíveis para o reparo aberto.[145]Greenhalgh RM, Brown LC, Powell JT, et al; United Kingdom EVAR Trial Investigators. Endovascular repair of aortic aneurysm in patients physically ineligible for open repair. N Engl J Med. 2010 May 20;362(20):1872-80. http://www.ncbi.nlm.nih.gov/pubmed/20382982?tool=bestpractice.com
Após o reparo, aneurismas da aorta abdominal maiores parecem estar associados a uma pior sobrevida tardia do que aneurismas menores (razão de riscos combinada 1.14 por aumento de 1 cm no diâmetro do aneurisma, IC de 95% 1.09 a 1.18; acompanhamento de 12.0 a 91.2 meses).[146]Khashram M, Hider PN, Williman JA, et al. Does the diameter of abdominal aortic aneurysm influence late survival following abdominal aortic aneurysm repair? A systematic review and meta-analysis. Vascular. 2016 Dec;24(6):658-67. http://www.ncbi.nlm.nih.gov/pubmed/27189809?tool=bestpractice.com A associação é mais pronunciada com o EVAR do que com o reparo aberto.
Para pacientes com AAA complexo e risco cirúrgico padrão, a cirurgia por via aberta ou EVAR deve ser considerado com base na aptidão, anatomia e preferência do paciente. Para pacientes com AAA complexo e alto risco cirúrgico, o EVAR com tecnologias fenestradas e ramificadas deve ser considerado como terapia de primeira linha. As endopróteses fenestradas e ramificadas tornaram-se o tratamento de primeira escolha para AAAs complexos na maioria dos centros de alto volume.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com Esses procedimentos são alternativas viáveis ao reparo por via aberta para AAA justarrenal e suprarrenal, ou para aqueles com AAA em que um pescoço curto ou doente impede o reparo convencional.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
redução do risco cardiovascular pré-operatório
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
O controle dos fatores de risco cardiovascular modificáveis no pré-operatório melhora a sobrevida de longo prazo após o reparo do AAA.[196]Khashram M, Williman JA, Hider PN, et al. Management of modifiable vascular risk factors improves late survival following abdominal aortic aneurysm repair: a systematic review and meta-analysis. Ann Vasc Surg. 2017 Feb;39:301-11. http://www.ncbi.nlm.nih.gov/pubmed/27666804?tool=bestpractice.com
Os pacientes devem ser incentivados a parar com o tabagismo e receber terapia medicamentosa (terapia de reposição de nicotina, nortriptilina e bupropiona) ou aconselhamento para ajudar, caso seja necessário.[1]Dehlin JM, Upchurch GR. Management of abdominal aortic aneurysms. Curr Treat Options Cardiovasc Med. 2005 Jun;7(2):119-30.
http://www.ncbi.nlm.nih.gov/pubmed/15935120?tool=bestpractice.com
[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482.
https://www.doi.org/10.1161/CIR.0000000000001106
http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
[13]Zankl AR, Schumacher H, Krumsdorf U, et al. Pathology, natural history and treatment of abdominal aortic aneurysms. Clin Res Cardiol. 2007 Mar;96(3):140-51.
http://www.ncbi.nlm.nih.gov/pubmed/17180573?tool=bestpractice.com
[15]Singh K, Bønaa H, Jacobsen BK, et al. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: the Tromsø Study. Am J Epidemiol. 2001 Aug 1;154(3):236-44.
https://academic.oup.com/aje/article/154/3/236/125840
http://www.ncbi.nlm.nih.gov/pubmed/11479188?tool=bestpractice.com
[22]Lederle FA, Johnson GR, Wilson SE, et al; Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative Study Group. Prevalence and associations of abdominal aortic aneurysm detected through screening. Ann Intern Med. 1997 Mar 15;126(6):441-9.
http://www.ncbi.nlm.nih.gov/pubmed/9072929?tool=bestpractice.com
[23]Wilmink TB, Quick CR, Day NE. The association between cigarette smoking and abdominal aortic aneurysms. J Vasc Surg. 1999 Dec;30(6):1099-105.
http://www.ncbi.nlm.nih.gov/pubmed/10587395?tool=bestpractice.com
[136]Hartmann-Boyce J, Chepkin SC, Ye W, et al. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst Rev. 2018 May 31;5:CD000146.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000146.pub5/full
http://www.ncbi.nlm.nih.gov/pubmed/29852054?tool=bestpractice.com
[137]Rigotti NA, Clair C, Munafò MR, et al. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2012 May 16;(5):CD001837.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001837.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/22592676?tool=bestpractice.com
[138]Howes S, Hartmann-Boyce J, Livingstone-Banks J, et al. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2020 Apr 22;(4):CD000031.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000031.pub5/full
http://www.ncbi.nlm.nih.gov/pubmed/32319681?tool=bestpractice.com
[  ]
What are the effects of adding bupropion or fluoxetine to other treatments compared with using other treatments alone for people trying to quit smoking?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.4337/fullMostre-me a resposta
]
What are the effects of adding bupropion or fluoxetine to other treatments compared with using other treatments alone for people trying to quit smoking?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.4337/fullMostre-me a resposta
O treinamento pré-operatório reduziu as complicações cardíacas pós-cirúrgicas em um pequeno ensaio clínico randomizado e controlado (ECRC) com pacientes submetidos a reparo de AAA aberto ou endovascular, embora uma revisão Cochrane e uma revisão sistemática separada de pré-reabilitação (exercícios) antes da cirurgia de AAA não tenham mostrado nenhum benefício em relação ao desfecho.[197]Barakat HM, Shahin Y, Khan JA, et al. Preoperative supervised exercise improves outcomes after elective abdominal aortic aneurysm repair: a randomized controlled trial. Ann Surg. 2016 Jul;264(1):47-53. http://www.ncbi.nlm.nih.gov/pubmed/26756766?tool=bestpractice.com [198]Fenton C, Tan AR, Abaraogu UO, et al. Prehabilitation exercise therapy before elective abdominal aortic aneurysm repair. Cochrane Database Syst Rev. 2021 Jul 8;7(7):CD013662. https://www.doi.org/10.1002/14651858.CD013662.pub2 http://www.ncbi.nlm.nih.gov/pubmed/34236703?tool=bestpractice.com [199]Bonner RJ, Wallace T, Jones AD, et al. The content of pre-habilitative interventions for patients undergoing repair of abdominal aortic aneurysms and their effect on post-operative outcomes: a systematic review. Eur J Vasc Endovasc Surg. 2021 May;61(5):756-65. https://www.doi.org/10.1016/j.ejvs.2021.01.043 http://www.ncbi.nlm.nih.gov/pubmed/33678532?tool=bestpractice.com Embora a prática de exercícios pré-operatórios possa ser benéfica para pacientes submetidos ao reparo de AAA, são necessárias investigações adicionais com ECRCs antes que possa ser recomendada mais amplamente.[200]Wee IJY, Choong AMTL. A systematic review of the impact of preoperative exercise for patients with abdominal aortic aneurysm. J Vasc Surg. 2020 Jun;71(6):2123-31.e1. https://www.doi.org/10.1016/j.jvs.2018.09.039 http://www.ncbi.nlm.nih.gov/pubmed/30606665?tool=bestpractice.com
O uso de estatina perioperatória desacelera o crescimento do aneurisma, reduz o risco de ruptura e diminui a mortalidade por reparo de AAA ou AAA roto.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A administração de estatinas deve ser iniciada pelo menos 1 mês antes da cirurgia, para reduzir a morbidade e a mortalidade cardiovascular, e deve ser mantida indefinidamente.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [141]Risum Ø, Sandven I, Sundhagen JO, et al. Editor's choice - effect of statins on total mortality in abdominal aortic aneurysm repair: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2021 Jan;61(1):114-20. https://www.doi.org/10.1016/j.ejvs.2020.08.007 http://www.ncbi.nlm.nih.gov/pubmed/32928667?tool=bestpractice.com
Pacientes com AAAs apresentam aumento do risco de eventos cardiovasculares adversos importantes. As evidências são limitadas, mas, na ausência de contraindicações, os pacientes com AAA devem receber terapia antiagregante plaquetária única (aspirina ou clopidogrel).[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [142]Aboyans V, Bauersachs R, Mazzolai L, et al. Antithrombotic therapies in aortic and peripheral arterial diseases in 2021: a consensus document from the ESC working group on aorta and peripheral vascular diseases, the ESC working group on thrombosis, and the ESC working group on cardiovascular pharmacotherapy. Eur Heart J. 2021 Oct 14;42(39):4013-24. https://www.doi.org/10.1093/eurheartj/ehab390 http://www.ncbi.nlm.nih.gov/pubmed/34279602?tool=bestpractice.com Isso deve ser mantido durante o período perioperatório.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
Deve-se controlar a hipertensão para reduzir a morbidade e a mortalidade cardiovascular.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
antibioticoterapia perioperatória
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
Antibioticoterapia perioperatória é administrada. O tratamento com antibióticos de amplo espectro é necessário, de acordo com os protocolos locais.
tratamento das causas infecciosas/inflamatórias
Tratamento adicional recomendado para ALGUNS pacientes no grupo de pacientes selecionado
A etiologia infecciosa ou inflamatória deve ser abordada.
Se houver suspeita de aneurisma infeccioso no paciente, o diagnóstico precoce, o tratamento imediato com antibióticos e o reparo cirúrgico urgente são essenciais para aprimorar os desfechos.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com Muitas vezes, o desbridamento extensivo é necessário durante o reparo cirúrgico urgente nesses pacientes. Há alto risco de complicações infecciosas secundárias, e uma cirurgia adicional pode ser necessária para novas lesões infecciosas. Culturas intraoperatórias devem ser realizadas para orientar de maneira precisa a antibioticoterapia subsequente; no entanto, muitas vezes são administrados antibióticos empíricos, pois hemoculturas periféricas e culturas de amostras cirúrgicas são negativas em uma grande proporção de pacientes.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A antibioticoterapia prolongada (de 4-6 semanas de duração até a vida toda) pode ser indicada, dependendo do patógeno específico, do tipo de reparo operatório e do estado imunológico do paciente[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
A aortite inflamatória (causada, por exemplo, por arterite de Takayasu ou arterite de células gigantes) é tratada com corticosteroide em altas doses e cirurgia.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [205]Ben Jmaà H, Karray R, Jmal H, et al. Surgical and endoluminal management of the inflammatory aortitis: a Tunisian center experience [in French]. J Med Vasc. 2017 Jul;42(4):213-20. http://www.ncbi.nlm.nih.gov/pubmed/28705339?tool=bestpractice.com
vazamento de reparo endovascular que requer tratamento
procedimento corretivo
Vazamento (endoleak) é o fluxo de sangue persistente fora do enxerto e dentro do saco do aneurisma.[206]Schurink GW, Aarts NJ, vanBockel JH. Endoleak after stent-graft treatment of abdominal aortic aneurysm: a meta-analysis of clinical studies. Br J Surg. 1999 May;86(5):581-7. http://www.ncbi.nlm.nih.gov/pubmed/10361173?tool=bestpractice.com [207]Veith FJ, Baum RA, Ohki T, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002 May;35(5):1029-35. http://www.ncbi.nlm.nih.gov/pubmed/12021724?tool=bestpractice.com Não é uma complicação após o reparo aberto.
A vigilância pós-operatória pode detectar grandes vazamentos (endoleaks) e a expansão do saco aneurismático. O risco após o reparo endovascular do aneurisma (EVAR) é de 24%.[206]Schurink GW, Aarts NJ, vanBockel JH. Endoleak after stent-graft treatment of abdominal aortic aneurysm: a meta-analysis of clinical studies. Br J Surg. 1999 May;86(5):581-7. http://www.ncbi.nlm.nih.gov/pubmed/10361173?tool=bestpractice.com Há cinco tipos de vazamento (endoleak).[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
Tipo I: vazamento no local de afixação (tipo IA na extremidade proximal da endoprótese ou oclusor da ilíaca; tipo IB na extremidade distal); geralmente imediatos, mas podem ocorrer vazamentos tardios.[Figure caption and citation for the preceding image starts]: Vazamento (endoleak) do tipo I na anastomose ilíaca esquerda distal (vazamento circulado)University of Michigan, mais especificamente os casos do Dr. Upchurch, representando os Departamentos de Cirurgia vascular e Radiologia [Citation ends].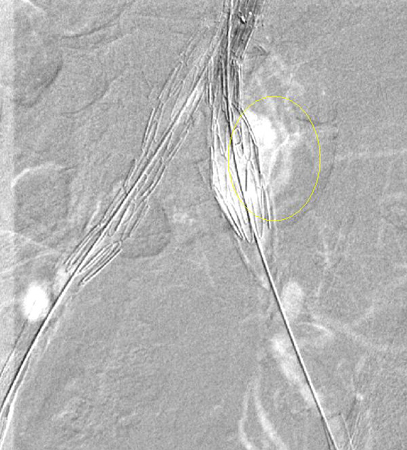 Deve-se fazer todo o esforço possível para reparar vazamentos (endoleaks) do tipo I antes de finalizar o procedimento (por exemplo, moldagem por balão da zona de vedação proximal, colocação de um manguito proximal, grampeamento interno, embolização líquida).[208]van Schaik TG, Meekel JP, Hoksbergen AWJ, et al. Systematic review of embolization of type I endoleaks using liquid embolic agents. J Vasc Surg. 2021 Sep;74(3):1024-32.
https://www.doi.org/10.1016/j.jvs.2021.03.061
http://www.ncbi.nlm.nih.gov/pubmed/33940072?tool=bestpractice.com
O vazamento (endoleak) persistente do tipo IA pode exigir conversão para reparo por via aberta, desde que o risco cirúrgico seja aceitável.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331.
https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2.
https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com
[209]Perini P, Bianchini Massoni C, Mariani E, et al. Systematic review and meta-analysis of the outcome of different treatments for type 1a endoleak after EVAR. Ann Vasc Surg. 2019 Oct;60:435-46.e1.
http://www.ncbi.nlm.nih.gov/pubmed/31200054?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Enxerto de endoprótese de extensão implantado para o mesmo vazamento (endoleak) do tipo I (circulado)University of Michigan, mais especificamente os casos do Dr. Upchurch, representando os Departamentos de Cirurgia vascular e Radiologia [Citation ends].
Deve-se fazer todo o esforço possível para reparar vazamentos (endoleaks) do tipo I antes de finalizar o procedimento (por exemplo, moldagem por balão da zona de vedação proximal, colocação de um manguito proximal, grampeamento interno, embolização líquida).[208]van Schaik TG, Meekel JP, Hoksbergen AWJ, et al. Systematic review of embolization of type I endoleaks using liquid embolic agents. J Vasc Surg. 2021 Sep;74(3):1024-32.
https://www.doi.org/10.1016/j.jvs.2021.03.061
http://www.ncbi.nlm.nih.gov/pubmed/33940072?tool=bestpractice.com
O vazamento (endoleak) persistente do tipo IA pode exigir conversão para reparo por via aberta, desde que o risco cirúrgico seja aceitável.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331.
https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2.
https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com
[209]Perini P, Bianchini Massoni C, Mariani E, et al. Systematic review and meta-analysis of the outcome of different treatments for type 1a endoleak after EVAR. Ann Vasc Surg. 2019 Oct;60:435-46.e1.
http://www.ncbi.nlm.nih.gov/pubmed/31200054?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Enxerto de endoprótese de extensão implantado para o mesmo vazamento (endoleak) do tipo I (circulado)University of Michigan, mais especificamente os casos do Dr. Upchurch, representando os Departamentos de Cirurgia vascular e Radiologia [Citation ends].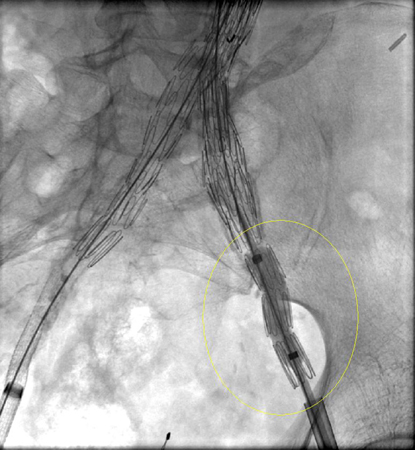 [Figure caption and citation for the preceding image starts]: Resolução do vazamento (endoleak) tipo I, revertido após extensão implantadaUniversity of Michigan, mais especificamente os casos do Dr. Upchurch, representando os Departamentos de Cirurgia vascular e Radiologia [Citation ends].
[Figure caption and citation for the preceding image starts]: Resolução do vazamento (endoleak) tipo I, revertido após extensão implantadaUniversity of Michigan, mais especificamente os casos do Dr. Upchurch, representando os Departamentos de Cirurgia vascular e Radiologia [Citation ends].
Tipo II: vazamento de ramo patente.[Figure caption and citation for the preceding image starts]: Vazamento (endoleak) tipo II (circundado) descoberto na tomografia computadorizada de seguimentoUniversity of Michigan, mais especificamente os casos do Dr. Upchurch, representando os Departamentos de Cirurgia vascular e Radiologia [Citation ends].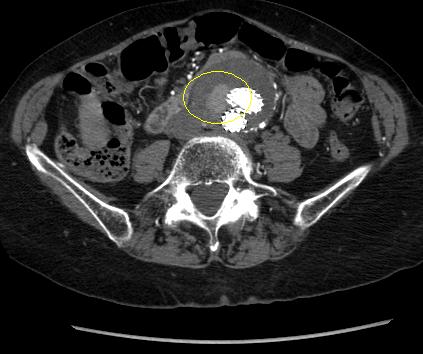 Pode ocorrer resolução espontânea, embora a persistência possa resultar em crescimento do saco.[210]Higashiura W, Greenberg RK, Katz E, et al. Predictive factors, morphologic effects, and proposed treatment paradigm for type II endoleaks after repair of infrarenal abdominal aortic aneurysms. J Vasc Interv Radiol. 2007 Aug;18(8):975-81.
http://www.ncbi.nlm.nih.gov/pubmed/17675614?tool=bestpractice.com
Se um vazamento (endoleak) tipo II ou outra anormalidade preocupante forem observados em TC com contraste 1 mês após o EVAR, recomenda-se imagiologia pós-operatória após 6 meses.[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2.
https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com
Aproximadamente 50% dos vazamentos (endoleaks) tipo II são diagnosticados antes de 30 dias de acompanhamento; 40% após 30 dias e 8% são diagnosticados após 12 meses de acompanhamento.[211]Charisis N, Bouris V, Conway AM, et al. A systematic review and pooled meta-analysis on the incidence and temporal occurrence of type II endoleak following an abdominal aortic aneurysm repair. Ann Vasc Surg. 2021 Aug;75:406-19.
http://www.ncbi.nlm.nih.gov/pubmed/33549794?tool=bestpractice.com
O tratamento permanece controverso e é recomendado caso o vazamento persista durante 6 a 12 meses ou se o tamanho do saco aneurismático aumentar de tal forma que as zonas de selamento proximal e/ou distal possam ser comprometidas.[212]Mansueto G, Cenzi D, Scuro A, et al. Treatment of type II endoleak with a transcatheter transcaval approach: results at 1-year follow-up. J Vasc Surg. 2007 Jun;45(6):1120-7.
http://www.ncbi.nlm.nih.gov/pubmed/17543674?tool=bestpractice.com
[213]Baum RA, Stavropoulos SW, Fairman RM, et al. Endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2003 Sep;14(9 Pt 1):1111-7.
http://www.ncbi.nlm.nih.gov/pubmed/14514802?tool=bestpractice.com
[214]Van Marrewijk CJ, Fransen G, Laheij RJ, et al. Is a type II endoleak after EVAR a harbinger of risk? Causes and outcome of open conversion and aneurysm rupture during follow-up. Eur J Vasc Endovasc Surg. 2004 Feb;27(2):128-37.
http://www.ncbi.nlm.nih.gov/pubmed/14718893?tool=bestpractice.com
[215]Harris PL, Vallabhaneni SR, Desgranges P, et al. Incidence and risk factors of late rupture, conversion, and death after endovascular repair of infrarenal aortic aneurysms: the EUROSTAR experience. J Vasc Surg. 2000 Oct;32(4):739-49.
http://www.ncbi.nlm.nih.gov/pubmed/11013038?tool=bestpractice.com
[216]Ultee KHJ, Büttner S, Huurman R, et al. Editor's choice - systematic review and meta-analysis of the outcome of treatment for type II endoleak following endovascular aneurysm repair. Eur J Vasc Endovasc Surg. 2018 Dec;56(6):794-807.
https://www.doi.org/10.1016/j.ejvs.2018.06.009
http://www.ncbi.nlm.nih.gov/pubmed/30104089?tool=bestpractice.com
[217]Smith T, Quencer KB. Best practice guidelines: imaging surveillance after endovascular aneurysm repair. AJR Am J Roentgenol. 2020 May;214(5):1165-74.
https://www.doi.org/10.2214/AJR.19.22197
http://www.ncbi.nlm.nih.gov/pubmed/32130043?tool=bestpractice.com
O tratamento de primeira escolha é a embolização com mola transarterial, embora ligadura laparoscópica de ramos colaterais, punção percutânea translombar direta do saco, embolização translombar e embolização transcaval transcateter tenham sido relatados.[207]Veith FJ, Baum RA, Ohki T, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002 May;35(5):1029-35.
http://www.ncbi.nlm.nih.gov/pubmed/12021724?tool=bestpractice.com
[212]Mansueto G, Cenzi D, Scuro A, et al. Treatment of type II endoleak with a transcatheter transcaval approach: results at 1-year follow-up. J Vasc Surg. 2007 Jun;45(6):1120-7.
http://www.ncbi.nlm.nih.gov/pubmed/17543674?tool=bestpractice.com
[213]Baum RA, Stavropoulos SW, Fairman RM, et al. Endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2003 Sep;14(9 Pt 1):1111-7.
http://www.ncbi.nlm.nih.gov/pubmed/14514802?tool=bestpractice.com
[214]Van Marrewijk CJ, Fransen G, Laheij RJ, et al. Is a type II endoleak after EVAR a harbinger of risk? Causes and outcome of open conversion and aneurysm rupture during follow-up. Eur J Vasc Endovasc Surg. 2004 Feb;27(2):128-37.
http://www.ncbi.nlm.nih.gov/pubmed/14718893?tool=bestpractice.com
[218]Steinmetz E, Rubin BG, Sanchez LA, et al. Type II endoleak after endovascular abdominal aortic aneurysm repair: a conservative approach with selective intervention is safe and cost-effective. J Vasc Surg. 2004 Feb;39(2):306-13.
http://www.ncbi.nlm.nih.gov/pubmed/14743129?tool=bestpractice.com
[219]Baum RA, Cope C, Fairman, et al. Translumbar embolization of type 2 endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2001 Jan;12(1):111-6.
http://www.ncbi.nlm.nih.gov/pubmed/11200344?tool=bestpractice.com
[220]Baum RA, Carpenter JP, Golden MA, et al. Treatment of type 2 endoleaks after endovascular repair of abdominal aortic aneurysms: comparison of transarterial and translumbar techniques. J Vasc Surg. 2002 Jan;35(1):23-9.
http://www.ncbi.nlm.nih.gov/pubmed/11802129?tool=bestpractice.com
[221]Schmid R, Gurke L, Aschwanden M, et al. CT-guided percutaneous embolization of a lumbar artery maintaining a type II endoleak. J Endovasc Ther. 2002 Apr;9(2):198-202.
http://www.ncbi.nlm.nih.gov/pubmed/12010100?tool=bestpractice.com
[222]Chin KM, Lee SQW, Lee HJ, et al. Preservation of stent graft after iatrogenic type III endoleak during open transperitoneal surgical intervention for complicated type II endoleak. Ann Vasc Surg. 2020 Jan;62:496.e1-496.e7.
http://www.ncbi.nlm.nih.gov/pubmed/31394250?tool=bestpractice.com
[223]Li Q, Hou P. Sac embolization and side branch embolization for preventing type II endoleaks after endovascular aneurysm repair: a meta-analysis. J Endovasc Ther. 2020 Feb;27(1):109-16.
https://www.doi.org/10.1177/1526602819878411
http://www.ncbi.nlm.nih.gov/pubmed/31566053?tool=bestpractice.com
[224]Akmal MM, Pabittei DR, Prapassaro T, et al. A systematic review of the current status of interventions for type II endoleak after EVAR for abdominal aortic aneurysms. Int J Surg. 2021 Nov;95:106138.
https://www.doi.org/10.1016/j.ijsu.2021.106138
http://www.ncbi.nlm.nih.gov/pubmed/34637951?tool=bestpractice.com
[225]Yu HYH, Lindström D, Wanhainen A, et al. Systematic review and meta-analysis of prophylactic aortic side branch embolization to prevent type II endoleaks. J Vasc Surg. 2020 Nov;72(5):1783-1792.e1.
https://www.doi.org/10.1016/j.jvs.2020.05.020
http://www.ncbi.nlm.nih.gov/pubmed/32442608?tool=bestpractice.com
[226]Zhang X, Ji L, Chen MY, et al. Transarterial embolization versus translumber embolization for type Ⅱ endoleak after endovascular abdominal aortic aneurysm repair: a meta-analysis. Chin Med Sci J. 2020 Jun 30;35(2):135-41.
https://www.doi.org/10.24920/003618
http://www.ncbi.nlm.nih.gov/pubmed/32684233?tool=bestpractice.com
Pode ocorrer resolução espontânea, embora a persistência possa resultar em crescimento do saco.[210]Higashiura W, Greenberg RK, Katz E, et al. Predictive factors, morphologic effects, and proposed treatment paradigm for type II endoleaks after repair of infrarenal abdominal aortic aneurysms. J Vasc Interv Radiol. 2007 Aug;18(8):975-81.
http://www.ncbi.nlm.nih.gov/pubmed/17675614?tool=bestpractice.com
Se um vazamento (endoleak) tipo II ou outra anormalidade preocupante forem observados em TC com contraste 1 mês após o EVAR, recomenda-se imagiologia pós-operatória após 6 meses.[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2.
https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com
Aproximadamente 50% dos vazamentos (endoleaks) tipo II são diagnosticados antes de 30 dias de acompanhamento; 40% após 30 dias e 8% são diagnosticados após 12 meses de acompanhamento.[211]Charisis N, Bouris V, Conway AM, et al. A systematic review and pooled meta-analysis on the incidence and temporal occurrence of type II endoleak following an abdominal aortic aneurysm repair. Ann Vasc Surg. 2021 Aug;75:406-19.
http://www.ncbi.nlm.nih.gov/pubmed/33549794?tool=bestpractice.com
O tratamento permanece controverso e é recomendado caso o vazamento persista durante 6 a 12 meses ou se o tamanho do saco aneurismático aumentar de tal forma que as zonas de selamento proximal e/ou distal possam ser comprometidas.[212]Mansueto G, Cenzi D, Scuro A, et al. Treatment of type II endoleak with a transcatheter transcaval approach: results at 1-year follow-up. J Vasc Surg. 2007 Jun;45(6):1120-7.
http://www.ncbi.nlm.nih.gov/pubmed/17543674?tool=bestpractice.com
[213]Baum RA, Stavropoulos SW, Fairman RM, et al. Endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2003 Sep;14(9 Pt 1):1111-7.
http://www.ncbi.nlm.nih.gov/pubmed/14514802?tool=bestpractice.com
[214]Van Marrewijk CJ, Fransen G, Laheij RJ, et al. Is a type II endoleak after EVAR a harbinger of risk? Causes and outcome of open conversion and aneurysm rupture during follow-up. Eur J Vasc Endovasc Surg. 2004 Feb;27(2):128-37.
http://www.ncbi.nlm.nih.gov/pubmed/14718893?tool=bestpractice.com
[215]Harris PL, Vallabhaneni SR, Desgranges P, et al. Incidence and risk factors of late rupture, conversion, and death after endovascular repair of infrarenal aortic aneurysms: the EUROSTAR experience. J Vasc Surg. 2000 Oct;32(4):739-49.
http://www.ncbi.nlm.nih.gov/pubmed/11013038?tool=bestpractice.com
[216]Ultee KHJ, Büttner S, Huurman R, et al. Editor's choice - systematic review and meta-analysis of the outcome of treatment for type II endoleak following endovascular aneurysm repair. Eur J Vasc Endovasc Surg. 2018 Dec;56(6):794-807.
https://www.doi.org/10.1016/j.ejvs.2018.06.009
http://www.ncbi.nlm.nih.gov/pubmed/30104089?tool=bestpractice.com
[217]Smith T, Quencer KB. Best practice guidelines: imaging surveillance after endovascular aneurysm repair. AJR Am J Roentgenol. 2020 May;214(5):1165-74.
https://www.doi.org/10.2214/AJR.19.22197
http://www.ncbi.nlm.nih.gov/pubmed/32130043?tool=bestpractice.com
O tratamento de primeira escolha é a embolização com mola transarterial, embora ligadura laparoscópica de ramos colaterais, punção percutânea translombar direta do saco, embolização translombar e embolização transcaval transcateter tenham sido relatados.[207]Veith FJ, Baum RA, Ohki T, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002 May;35(5):1029-35.
http://www.ncbi.nlm.nih.gov/pubmed/12021724?tool=bestpractice.com
[212]Mansueto G, Cenzi D, Scuro A, et al. Treatment of type II endoleak with a transcatheter transcaval approach: results at 1-year follow-up. J Vasc Surg. 2007 Jun;45(6):1120-7.
http://www.ncbi.nlm.nih.gov/pubmed/17543674?tool=bestpractice.com
[213]Baum RA, Stavropoulos SW, Fairman RM, et al. Endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2003 Sep;14(9 Pt 1):1111-7.
http://www.ncbi.nlm.nih.gov/pubmed/14514802?tool=bestpractice.com
[214]Van Marrewijk CJ, Fransen G, Laheij RJ, et al. Is a type II endoleak after EVAR a harbinger of risk? Causes and outcome of open conversion and aneurysm rupture during follow-up. Eur J Vasc Endovasc Surg. 2004 Feb;27(2):128-37.
http://www.ncbi.nlm.nih.gov/pubmed/14718893?tool=bestpractice.com
[218]Steinmetz E, Rubin BG, Sanchez LA, et al. Type II endoleak after endovascular abdominal aortic aneurysm repair: a conservative approach with selective intervention is safe and cost-effective. J Vasc Surg. 2004 Feb;39(2):306-13.
http://www.ncbi.nlm.nih.gov/pubmed/14743129?tool=bestpractice.com
[219]Baum RA, Cope C, Fairman, et al. Translumbar embolization of type 2 endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2001 Jan;12(1):111-6.
http://www.ncbi.nlm.nih.gov/pubmed/11200344?tool=bestpractice.com
[220]Baum RA, Carpenter JP, Golden MA, et al. Treatment of type 2 endoleaks after endovascular repair of abdominal aortic aneurysms: comparison of transarterial and translumbar techniques. J Vasc Surg. 2002 Jan;35(1):23-9.
http://www.ncbi.nlm.nih.gov/pubmed/11802129?tool=bestpractice.com
[221]Schmid R, Gurke L, Aschwanden M, et al. CT-guided percutaneous embolization of a lumbar artery maintaining a type II endoleak. J Endovasc Ther. 2002 Apr;9(2):198-202.
http://www.ncbi.nlm.nih.gov/pubmed/12010100?tool=bestpractice.com
[222]Chin KM, Lee SQW, Lee HJ, et al. Preservation of stent graft after iatrogenic type III endoleak during open transperitoneal surgical intervention for complicated type II endoleak. Ann Vasc Surg. 2020 Jan;62:496.e1-496.e7.
http://www.ncbi.nlm.nih.gov/pubmed/31394250?tool=bestpractice.com
[223]Li Q, Hou P. Sac embolization and side branch embolization for preventing type II endoleaks after endovascular aneurysm repair: a meta-analysis. J Endovasc Ther. 2020 Feb;27(1):109-16.
https://www.doi.org/10.1177/1526602819878411
http://www.ncbi.nlm.nih.gov/pubmed/31566053?tool=bestpractice.com
[224]Akmal MM, Pabittei DR, Prapassaro T, et al. A systematic review of the current status of interventions for type II endoleak after EVAR for abdominal aortic aneurysms. Int J Surg. 2021 Nov;95:106138.
https://www.doi.org/10.1016/j.ijsu.2021.106138
http://www.ncbi.nlm.nih.gov/pubmed/34637951?tool=bestpractice.com
[225]Yu HYH, Lindström D, Wanhainen A, et al. Systematic review and meta-analysis of prophylactic aortic side branch embolization to prevent type II endoleaks. J Vasc Surg. 2020 Nov;72(5):1783-1792.e1.
https://www.doi.org/10.1016/j.jvs.2020.05.020
http://www.ncbi.nlm.nih.gov/pubmed/32442608?tool=bestpractice.com
[226]Zhang X, Ji L, Chen MY, et al. Transarterial embolization versus translumber embolization for type Ⅱ endoleak after endovascular abdominal aortic aneurysm repair: a meta-analysis. Chin Med Sci J. 2020 Jun 30;35(2):135-41.
https://www.doi.org/10.24920/003618
http://www.ncbi.nlm.nih.gov/pubmed/32684233?tool=bestpractice.com
Tipo III: defeito do enxerto com vazamento através de rasgos no tecido, desconexão do enxerto ou desintegração do tecido.[206]Schurink GW, Aarts NJ, vanBockel JH. Endoleak after stent-graft treatment of abdominal aortic aneurysm: a meta-analysis of clinical studies. Br J Surg. 1999 May;86(5):581-7. http://www.ncbi.nlm.nih.gov/pubmed/10361173?tool=bestpractice.com [207]Veith FJ, Baum RA, Ohki T, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002 May;35(5):1029-35. http://www.ncbi.nlm.nih.gov/pubmed/12021724?tool=bestpractice.com [227]Kwon J, Dimuzio P, Salvatore D, et al. Incidence of stent graft failure from type IIIB endoleak in contemporary endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2020 Feb;71(2):645-53. https://www.doi.org/10.1016/j.jvs.2019.06.183 http://www.ncbi.nlm.nih.gov/pubmed/31466740?tool=bestpractice.com O reparo é indicado após a descoberta (extensão do enxerto por endoprótese endovascular).[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2. https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com [213]Baum RA, Stavropoulos SW, Fairman RM, et al. Endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2003 Sep;14(9 Pt 1):1111-7. http://www.ncbi.nlm.nih.gov/pubmed/14514802?tool=bestpractice.com [217]Smith T, Quencer KB. Best practice guidelines: imaging surveillance after endovascular aneurysm repair. AJR Am J Roentgenol. 2020 May;214(5):1165-74. https://www.doi.org/10.2214/AJR.19.22197 http://www.ncbi.nlm.nih.gov/pubmed/32130043?tool=bestpractice.com [228]Lowe C, Hansrani V, Madan M, et al. Type IIIb endoleak after elective endovascular aneurysm repair: a systematic review. J Cardiovasc Surg (Torino). 2020 Jun;61(3):308-16. http://www.ncbi.nlm.nih.gov/pubmed/29616524?tool=bestpractice.com
Tipo IV: vazamento pelos poros da parede do enxerto.[206]Schurink GW, Aarts NJ, vanBockel JH. Endoleak after stent-graft treatment of abdominal aortic aneurysm: a meta-analysis of clinical studies. Br J Surg. 1999 May;86(5):581-7. http://www.ncbi.nlm.nih.gov/pubmed/10361173?tool=bestpractice.com [207]Veith FJ, Baum RA, Ohki T, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002 May;35(5):1029-35. http://www.ncbi.nlm.nih.gov/pubmed/12021724?tool=bestpractice.com Esses vazamentos não são comuns com as novas endopróteses e são limitados.[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2. https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com [213]Baum RA, Stavropoulos SW, Fairman RM, et al. Endoleaks after endovascular repair of abdominal aortic aneurysms. J Vasc Interv Radiol. 2003 Sep;14(9 Pt 1):1111-7. http://www.ncbi.nlm.nih.gov/pubmed/14514802?tool=bestpractice.com
Tipo V (endotensão): endotensão é o aumento da pressão dentro do saco após EVAR sem visualização de vazamento (endoleak) em TCs com contraste tardias. É menos comum com os enxertos de nova geração.[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2. https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com Não existe um método padrão para medir a endotensão nem há consenso sobre a terapia indicada na ausência de aumento do aneurisma: no entanto, sugere-se o tratamento da endotensão para impedir a ruptura do aneurisma em pacientes selecionados com expansão contínua do aneurisma.[76]Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018 Jan;67(1):2-77.e2. https://www.jvascsurg.org/article/S0741-5214(17)32369-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/29268916?tool=bestpractice.com [207]Veith FJ, Baum RA, Ohki T, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002 May;35(5):1029-35. http://www.ncbi.nlm.nih.gov/pubmed/12021724?tool=bestpractice.com [217]Smith T, Quencer KB. Best practice guidelines: imaging surveillance after endovascular aneurysm repair. AJR Am J Roentgenol. 2020 May;214(5):1165-74. https://www.doi.org/10.2214/AJR.19.22197 http://www.ncbi.nlm.nih.gov/pubmed/32130043?tool=bestpractice.com
redução do risco cardiovascular pré-operatório
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
O controle dos fatores de risco cardiovascular modificáveis no pré-operatório melhora a sobrevida de longo prazo após o reparo do AAA.[196]Khashram M, Williman JA, Hider PN, et al. Management of modifiable vascular risk factors improves late survival following abdominal aortic aneurysm repair: a systematic review and meta-analysis. Ann Vasc Surg. 2017 Feb;39:301-11. http://www.ncbi.nlm.nih.gov/pubmed/27666804?tool=bestpractice.com
Os pacientes devem ser incentivados a parar com o tabagismo e receber terapia medicamentosa (terapia de reposição de nicotina, nortriptilina e bupropiona) ou aconselhamento para ajudar, caso seja necessário.[1]Dehlin JM, Upchurch GR. Management of abdominal aortic aneurysms. Curr Treat Options Cardiovasc Med. 2005 Jun;7(2):119-30.
http://www.ncbi.nlm.nih.gov/pubmed/15935120?tool=bestpractice.com
[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482.
https://www.doi.org/10.1161/CIR.0000000000001106
http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
[13]Zankl AR, Schumacher H, Krumsdorf U, et al. Pathology, natural history and treatment of abdominal aortic aneurysms. Clin Res Cardiol. 2007 Mar;96(3):140-51.
http://www.ncbi.nlm.nih.gov/pubmed/17180573?tool=bestpractice.com
[15]Singh K, Bønaa H, Jacobsen BK, et al. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: the Tromsø Study. Am J Epidemiol. 2001 Aug 1;154(3):236-44.
https://academic.oup.com/aje/article/154/3/236/125840
http://www.ncbi.nlm.nih.gov/pubmed/11479188?tool=bestpractice.com
[22]Lederle FA, Johnson GR, Wilson SE, et al; Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative Study Group. Prevalence and associations of abdominal aortic aneurysm detected through screening. Ann Intern Med. 1997 Mar 15;126(6):441-9.
http://www.ncbi.nlm.nih.gov/pubmed/9072929?tool=bestpractice.com
[23]Wilmink TB, Quick CR, Day NE. The association between cigarette smoking and abdominal aortic aneurysms. J Vasc Surg. 1999 Dec;30(6):1099-105.
http://www.ncbi.nlm.nih.gov/pubmed/10587395?tool=bestpractice.com
[136]Hartmann-Boyce J, Chepkin SC, Ye W, et al. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst Rev. 2018 May 31;5:CD000146.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000146.pub5/full
http://www.ncbi.nlm.nih.gov/pubmed/29852054?tool=bestpractice.com
[137]Rigotti NA, Clair C, Munafò MR, et al. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2012 May 16;(5):CD001837.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001837.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/22592676?tool=bestpractice.com
[138]Howes S, Hartmann-Boyce J, Livingstone-Banks J, et al. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2020 Apr 22;(4):CD000031.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000031.pub5/full
http://www.ncbi.nlm.nih.gov/pubmed/32319681?tool=bestpractice.com
[  ]
What are the effects of adding bupropion or fluoxetine to other treatments compared with using other treatments alone for people trying to quit smoking?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.4337/fullMostre-me a resposta
]
What are the effects of adding bupropion or fluoxetine to other treatments compared with using other treatments alone for people trying to quit smoking?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.4337/fullMostre-me a resposta
O treinamento pré-operatório reduziu as complicações cardíacas pós-cirúrgicas em um pequeno ensaio clínico randomizado e controlado (ECRC) com pacientes submetidos a reparo de AAA aberto ou endovascular, embora uma revisão Cochrane e uma revisão sistemática separada de pré-reabilitação (exercícios) antes da cirurgia de AAA não tenham mostrado nenhum benefício em relação ao desfecho.[197]Barakat HM, Shahin Y, Khan JA, et al. Preoperative supervised exercise improves outcomes after elective abdominal aortic aneurysm repair: a randomized controlled trial. Ann Surg. 2016 Jul;264(1):47-53. http://www.ncbi.nlm.nih.gov/pubmed/26756766?tool=bestpractice.com [198]Fenton C, Tan AR, Abaraogu UO, et al. Prehabilitation exercise therapy before elective abdominal aortic aneurysm repair. Cochrane Database Syst Rev. 2021 Jul 8;7(7):CD013662. https://www.doi.org/10.1002/14651858.CD013662.pub2 http://www.ncbi.nlm.nih.gov/pubmed/34236703?tool=bestpractice.com [199]Bonner RJ, Wallace T, Jones AD, et al. The content of pre-habilitative interventions for patients undergoing repair of abdominal aortic aneurysms and their effect on post-operative outcomes: a systematic review. Eur J Vasc Endovasc Surg. 2021 May;61(5):756-65. https://www.doi.org/10.1016/j.ejvs.2021.01.043 http://www.ncbi.nlm.nih.gov/pubmed/33678532?tool=bestpractice.com Embora a prática de exercícios pré-operatórios possa ser benéfica para pacientes submetidos ao reparo de AAA, são necessárias investigações adicionais com ECRCs antes que possa ser recomendada mais amplamente.[200]Wee IJY, Choong AMTL. A systematic review of the impact of preoperative exercise for patients with abdominal aortic aneurysm. J Vasc Surg. 2020 Jun;71(6):2123-31.e1. https://www.doi.org/10.1016/j.jvs.2018.09.039 http://www.ncbi.nlm.nih.gov/pubmed/30606665?tool=bestpractice.com
O uso de estatina perioperatória desacelera o crescimento do aneurisma, reduz o risco de ruptura e diminui a mortalidade por reparo de AAA ou AAA roto.[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com A administração de estatinas deve ser iniciada pelo menos 1 mês antes da cirurgia, para reduzir a morbidade e a mortalidade cardiovascular, e deve ser mantida indefinidamente.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [141]Risum Ø, Sandven I, Sundhagen JO, et al. Editor's choice - effect of statins on total mortality in abdominal aortic aneurysm repair: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2021 Jan;61(1):114-20. https://www.doi.org/10.1016/j.ejvs.2020.08.007 http://www.ncbi.nlm.nih.gov/pubmed/32928667?tool=bestpractice.com
Pacientes com AAAs apresentam aumento do risco de eventos cardiovasculares adversos importantes. As evidências são limitadas, mas, na ausência de contraindicações, os pacientes com AAA devem receber terapia antiagregante plaquetária única (aspirina ou clopidogrel).[5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com [142]Aboyans V, Bauersachs R, Mazzolai L, et al. Antithrombotic therapies in aortic and peripheral arterial diseases in 2021: a consensus document from the ESC working group on aorta and peripheral vascular diseases, the ESC working group on thrombosis, and the ESC working group on cardiovascular pharmacotherapy. Eur Heart J. 2021 Oct 14;42(39):4013-24. https://www.doi.org/10.1093/eurheartj/ehab390 http://www.ncbi.nlm.nih.gov/pubmed/34279602?tool=bestpractice.com Isso deve ser mantido durante o período perioperatório.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com
Deve-se controlar a hipertensão para reduzir a morbidade e a mortalidade cardiovascular.[3]Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2024 Feb;67(2):192-331. https://www.ejves.com/article/S1078-5884(23)00889-4/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38307694?tool=bestpractice.com [5]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. https://www.doi.org/10.1161/CIR.0000000000001106 http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
antibioticoterapia perioperatória
Tratamento recomendado para TODOS os pacientes no grupo de pacientes selecionado
Antibioticoterapia perioperatória é administrada. O tratamento com antibióticos de amplo espectro é necessário, de acordo com os protocolos locais.

Escolha um grupo de pacientes para ver nossas recomendações
Observe que as formulações/vias e doses podem diferir entre nomes e marcas de medicamentos, formulários de medicamentos ou localidades. As recomendações de tratamento são específicas para os grupos de pacientes. Ver aviso legal
O uso deste conteúdo está sujeito ao nosso aviso legal

