Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
all patients
treatment of underlying chronic liver disease and prevention of superimposed hepatic insult
As cirrhosis is the pathological end-stage of any chronic liver disease, it is essential to treat the underlying causative condition.
Oral direct-acting antivirals are considered a first-line treatment for chronic hepatitis C virus infection. One systematic review and meta-analysis found that early treatment with direct-acting antivirals reduced the recurrence of hepatocellular carcinoma, liver decompensation, and all-cause mortality, and prevented hepatocellular carcinoma in patients with compensated cirrhosis and without cirrhosis but did not prevent liver transplantation.[93]Yew KC, Tan QR, Lim PC, et al. Assessing the impact of direct-acting antivirals on hepatitis C complications: a systematic review and meta-analysis. Naunyn Schmiedebergs Arch Pharmacol. 2024 Mar;397(3):1421-31. http://www.ncbi.nlm.nih.gov/pubmed/37728622?tool=bestpractice.com Regimens depend on the genotype and presence or absence of cirrhosis.[94]American Association for the Study of Liver Diseases; Infectious Diseases Society of America. Hepatitis C guidance 2023 update: recommendations for testing, managing, and treating hepatitis C virus infection. Oct 2023 [internet publication]. https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciad319/7179952 Local guidance should be consulted. See Hepatitis C. Antivirals may be indicated for patients with chronic hepatitis B.[84]European Association for the Study of the Liver. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection. J Hepatol. 2017 Aug;67(2):370-98. https://www.journal-of-hepatology.eu/article/S0168-8278(17)30185-X/fulltext http://www.ncbi.nlm.nih.gov/pubmed/28427875?tool=bestpractice.com [95]Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018 Apr;67(4):1560-99. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5975958 http://www.ncbi.nlm.nih.gov/pubmed/29405329?tool=bestpractice.com See Hepatitis B.
Superimposed hepatic insult may be prevented through the avoidance of alcohol and other hepatotoxic drugs (e.g., non-steroidal anti-inflammatory drugs [NSAIDs] and high doses of paracetamol [>2-3 g/day]), immunisation against hepatitis A and B for susceptible patients, management of metabolic risk factors, maintenance of adequate nutrition, and regular exercise.
monitoring for complications
Treatment recommended for ALL patients in selected patient group
Cirrhosis is associated with serious complications including portal hypertension causing ascites (further complicated by spontaneous bacterial peritonitis and hepatic hydrothorax), gastro-oesophageal varices and portosystemic encephalopathy, acute kidney injury and hepatopulmonary syndromes, portopulmonary hypertension, hepatocellular carcinoma, and acute-on-chronic liver failure.
Prompt detection and treatment of these complications is essential in order to minimise related morbidity and mortality. Imaging tests include: abdominal ultrasound for the detection of ascites; upper gastrointestinal endoscopy in selected patients for the detection of gastro-oesophageal varices; and abdominal ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) for the detection of hepatocellular carcinoma.
Other specialised tests may be required depending on individual symptoms.
See Oesophageal varices, Spontaneous bacterial peritonitis, Hepatic encephalopathy, Hepatorenal syndrome, and Hepatocellular carcinoma.
supportive and palliative care
Treatment recommended for ALL patients in selected patient group
It is recommended that patients hospitalised with cirrhosis receive formal dietician assessment, and steps should be taken to minimise the fasting period prior to procedures (e.g., by giving them a pre-bedtime snack or early-morning snack if the procedure will be in the late afternoon).[138]Lai JC, Tandon P, Bernal W, et al. Malnutrition, frailty, and sarcopenia in patients with cirrhosis: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Sep;74(3):1611-44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9134787 http://www.ncbi.nlm.nih.gov/pubmed/34233031?tool=bestpractice.com Parenteral supplementation may be required for those who cannot meet their nutritional intake needs orally. Recommended protein intake for adults with cirrhosis is 1.2 to 1.5 g/kg (ideal body weight) per day, and 1.2 to 2 g/kg (ideal body weight) per day if critically ill.
As cirrhosis is a life-limiting condition, palliative care should be offered alongside other curative therapies, and may be relevant for patients with compensated cirrhosis and decompensated cirrhosis.[174]Tandon P, Walling A, Patton H, et al. AGA clinical practice update on palliative care management in cirrhosis: expert review. Clin Gastroenterol Hepatol. 2021 Apr;19(4):646-56. https://www.cghjournal.org/article/S1542-3565(20)31561-5/fulltext http://www.ncbi.nlm.nih.gov/pubmed/33221550?tool=bestpractice.com The American Gastroenterological Association and the American Association for the Study of Liver Disease have both published guidelines on palliative care in patients with cirrhosis. These promote advanced care planning, assessment and management of symptoms (including pain, breathlessness, muscle cramps, sexual dysfunction, insomnia, daytime sleepiness, fatigue, pruritus, anxiety, and depression), screening for carer needs, and early liaison with local palliative care teams.[174]Tandon P, Walling A, Patton H, et al. AGA clinical practice update on palliative care management in cirrhosis: expert review. Clin Gastroenterol Hepatol. 2021 Apr;19(4):646-56. https://www.cghjournal.org/article/S1542-3565(20)31561-5/fulltext http://www.ncbi.nlm.nih.gov/pubmed/33221550?tool=bestpractice.com [175]Rogal SS, Hansen L, Patel A, et al. AASLD practice guidance: palliative care and symptom-based management in decompensated cirrhosis. Hepatology. 2022 Sep;76(3):819-53. https://aasldpubs.onlinelibrary.wiley.com/doi/10.1002/hep.32378 http://www.ncbi.nlm.nih.gov/pubmed/35103995?tool=bestpractice.com Particular note is given to chronic pain management in the setting of diminished liver function and novel treatments for refractory ascites.[175]Rogal SS, Hansen L, Patel A, et al. AASLD practice guidance: palliative care and symptom-based management in decompensated cirrhosis. Hepatology. 2022 Sep;76(3):819-53. https://aasldpubs.onlinelibrary.wiley.com/doi/10.1002/hep.32378 http://www.ncbi.nlm.nih.gov/pubmed/35103995?tool=bestpractice.com
sodium restriction and diuretic therapy for ascites
Additional treatment recommended for SOME patients in selected patient group
Ascites is the most common complication of cirrhosis.
Every patient with new-onset ascites should undergo a diagnostic paracentesis: cell count with differential, albumin, and total protein should be measured in the ascitic fluid. Ascitic fluid should also be sent for culture and cytology.
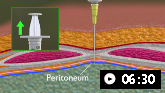
Demonstrates how to perform diagnostic and therapeutic abdominal paracentesis.
The serum-ascites albumin gradient (SAAG) should be calculated: a SAAG of ≥11 g/L with low ascitic fluid total protein is consistent with portal hypertension secondary to cirrhosis.
Treatment involves a no-added-salt diet (daily intake of not more than 5 to 6.5 g) and the use of diuretics.[101]Aithal GP, Palaniyappan N, China L, et al. Guidelines on the management of ascites in cirrhosis. Gut. 2021 Jan;70(1):9-29. https://gut.bmj.com/content/70/1/9.long http://www.ncbi.nlm.nih.gov/pubmed/33067334?tool=bestpractice.com First-line diuretic should be spironolactone due to its effects on aldosterone and maintaining normal serum potassium. Furosemide may be added to patients who do not respond to spironolactone.[101]Aithal GP, Palaniyappan N, China L, et al. Guidelines on the management of ascites in cirrhosis. Gut. 2021 Jan;70(1):9-29. https://gut.bmj.com/content/70/1/9.long http://www.ncbi.nlm.nih.gov/pubmed/33067334?tool=bestpractice.com Once-daily dosing is typically preferred. The doses of both oral diuretics can be increased simultaneously every 3-5 days (maintaining the 100 mg to 40 mg ratio) if weight loss and natriuresis are inadequate.[176]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48. https://aasldpubs.onlinelibrary.wiley.com/doi/10.1002/hep.31884 http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com Serum sodium, potassium, and creatinine should be monitored.
Non-steroidal anti-inflammatory drugs (NSAIDs), ACE inhibitors, and other nephrotoxins should be avoided in patients with ascites.[90]Flamm SL, Wong F, Ahn J, et al. AGA clinical practice update on the evaluation and management of acute kidney injury in patients with cirrhosis: expert review. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2707-16. https://www.cghjournal.org/article/S1542-3565(22)00829-1/fulltext http://www.ncbi.nlm.nih.gov/pubmed/36075500?tool=bestpractice.com
Primary options
spironolactone: 100 mg orally once daily initially, titrate as needed every 3-5 days, maximum 400 mg/day
OR
spironolactone: 100 mg orally once daily initially, titrate as needed every 3-5 days, maximum 400 mg/day
and
furosemide: 40 mg orally once daily initially, titrate as needed every 3-5 days, maximum 160 mg/day
liver transplantation
Patients who develop complications of cirrhosis such as hepatocellular carcinoma or signs of decompensation (ascites, jaundice, variceal haemorrhage, hepatopulmonary syndrome, hepatic hydrothorax, portal systemic encephalopathy, or hepatorenal syndrome) should be referred for liver transplant evaluation without delay. Transplant assessment may be a prolonged process and early referrals are preferable. Some patients with acute-on-chronic liver failure may benefit from early liver transplantation.[167]Bajaj JS, O'Leary JG, Lai JC, et al. Acute-on-chronic liver failure clinical guidelines. Am J Gastroenterol. 2022 Feb 1;117(2):225-52. https://www.doi.org/10.14309/ajg.0000000000001595 http://www.ncbi.nlm.nih.gov/pubmed/35006099?tool=bestpractice.com
Orthotopic liver transplantation remains the only curative treatment option for patients with decompensated cirrhosis.
A survival benefit from undergoing liver transplantation is seen when the Model of End-Stage Liver Disease (MELD) score is ≥15. [ MELDNa scores (for liver transplantation listing purposes, not appropriate for patients under age 12 years) (SI units) Opens in new window ]
transjugular intrahepatic portosystemic shunt (TIPS)
Patients not suitable for liver transplantation should be considered for TIPS placement.[103]Benmassaoud A, Freeman SC, Roccarina D, et al. Treatment for ascites in adults with decompensated liver cirrhosis: a network meta-analysis. Cochrane Database Syst Rev. 2020 Jan 16;1:CD013123. https://www.doi.org/10.1002/14651858.CD013123.pub2 http://www.ncbi.nlm.nih.gov/pubmed/31978257?tool=bestpractice.com
Meta-analyses indicate that TIPS is more effective than paracentesis for control of refractory ascites, but is associated with a higher incidence of hepatic encephalopathy.[103]Benmassaoud A, Freeman SC, Roccarina D, et al. Treatment for ascites in adults with decompensated liver cirrhosis: a network meta-analysis. Cochrane Database Syst Rev. 2020 Jan 16;1:CD013123.
https://www.doi.org/10.1002/14651858.CD013123.pub2
http://www.ncbi.nlm.nih.gov/pubmed/31978257?tool=bestpractice.com
[104]D'Amico G, Luca A, Morabito A, et al. Uncovered transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis. Gastroenterology. 2005 Oct;129(4):1282-93.
http://www.ncbi.nlm.nih.gov/pubmed/16230081?tool=bestpractice.com
[105]Saab S, Nieto JM, Lewis SK, et al. TIPS versus paracentesis for cirrhotic patients with refractory ascites. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD004889.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004889.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/17054221?tool=bestpractice.com
[106]Albillos A, Bañares R, González M, et al. A meta-analysis of transjugular intrahepatic portosystemic shunt versus paracentesis for refractory ascites. J Hepatol. 2005 Dec;43(6):990-6.
http://www.ncbi.nlm.nih.gov/pubmed/16139922?tool=bestpractice.com
[107]Salerno F, Cammà C, Enea M, et al. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007 Sep;133(3):825-34.
https://www.doi.org/10.1053/j.gastro.2007.06.020
http://www.ncbi.nlm.nih.gov/pubmed/17678653?tool=bestpractice.com
[108]Chen RP, Zhu Ge XJ, Huang ZM, et al. Prophylactic use of transjugular intrahepatic portosystemic shunt aids in the treatment of refractory ascites: metaregression and trial sequential meta-analysis. J Clin Gastroenterol. 2014 Mar;48(3):290-9.
http://www.ncbi.nlm.nih.gov/pubmed/24030734?tool=bestpractice.com
[109]Bai M, Qi XS, Yang ZP, et al. TIPS improves liver transplantation-free survival in cirrhotic patients with refractory ascites: an updated meta-analysis. World J Gastroenterol. 2014 Mar 14;20(10):2704-14.
https://www.doi.org/10.3748/wjg.v20.i10.2704
http://www.ncbi.nlm.nih.gov/pubmed/24627607?tool=bestpractice.com
Overall mortality does not appear to differ between the two interventions, but TIPS may confer a modest benefit with respect to transplant-free survival.[103]Benmassaoud A, Freeman SC, Roccarina D, et al. Treatment for ascites in adults with decompensated liver cirrhosis: a network meta-analysis. Cochrane Database Syst Rev. 2020 Jan 16;1:CD013123.
https://www.doi.org/10.1002/14651858.CD013123.pub2
http://www.ncbi.nlm.nih.gov/pubmed/31978257?tool=bestpractice.com
[104]D'Amico G, Luca A, Morabito A, et al. Uncovered transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis. Gastroenterology. 2005 Oct;129(4):1282-93.
http://www.ncbi.nlm.nih.gov/pubmed/16230081?tool=bestpractice.com
[105]Saab S, Nieto JM, Lewis SK, et al. TIPS versus paracentesis for cirrhotic patients with refractory ascites. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD004889.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004889.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/17054221?tool=bestpractice.com
[106]Albillos A, Bañares R, González M, et al. A meta-analysis of transjugular intrahepatic portosystemic shunt versus paracentesis for refractory ascites. J Hepatol. 2005 Dec;43(6):990-6.
http://www.ncbi.nlm.nih.gov/pubmed/16139922?tool=bestpractice.com
[107]Salerno F, Cammà C, Enea M, et al. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007 Sep;133(3):825-34.
https://www.doi.org/10.1053/j.gastro.2007.06.020
http://www.ncbi.nlm.nih.gov/pubmed/17678653?tool=bestpractice.com
[108]Chen RP, Zhu Ge XJ, Huang ZM, et al. Prophylactic use of transjugular intrahepatic portosystemic shunt aids in the treatment of refractory ascites: metaregression and trial sequential meta-analysis. J Clin Gastroenterol. 2014 Mar;48(3):290-9.
http://www.ncbi.nlm.nih.gov/pubmed/24030734?tool=bestpractice.com
[109]Bai M, Qi XS, Yang ZP, et al. TIPS improves liver transplantation-free survival in cirrhotic patients with refractory ascites: an updated meta-analysis. World J Gastroenterol. 2014 Mar 14;20(10):2704-14.
https://www.doi.org/10.3748/wjg.v20.i10.2704
http://www.ncbi.nlm.nih.gov/pubmed/24627607?tool=bestpractice.com
One Cochrane systematic review and network meta-analysis reported that the overall certainty (quality) of evidence was very low, primarily because of unclear or high risk of bias in trials assessing interventions for the treatment of refractory ascites in patients with cirrhosis.[103]Benmassaoud A, Freeman SC, Roccarina D, et al. Treatment for ascites in adults with decompensated liver cirrhosis: a network meta-analysis. Cochrane Database Syst Rev. 2020 Jan 16;1:CD013123.
https://www.doi.org/10.1002/14651858.CD013123.pub2
http://www.ncbi.nlm.nih.gov/pubmed/31978257?tool=bestpractice.com
[  ]
For adults with decompensated liver cirrhosis, how do treatments for ascites compare?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.3068/fullShow me the answer
]
For adults with decompensated liver cirrhosis, how do treatments for ascites compare?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.3068/fullShow me the answer
Disease severity at the time of TIPS placement is an important predictive factor for outcomes.[112]Lebrec D, Giuily N, Hadengue A, et al. Transjugular intrahepatic portosystemic shunts: comparison with paracentesis in patients with cirrhosis and refractory ascites: a randomized trial. French Group of Clinicians and a Group of Biologists. J Hepatol. 1996 Aug;25(2):135-44. http://www.ncbi.nlm.nih.gov/pubmed/8878773?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer