Íleo paralítico pós-operatório
As tentativas para prevenir o íleo pós-operatório devem começar no período perioperatório, incluindo o manejo hídrico intraoperatório adequado e a evitação de analgesia com opioides. O programa Enhanced Recovery After Surgery (ERAS) é cada vez mais utilizado na tentativa de acelerar a recuperação da função intestinal e encurtar a duração da internação hospitalar.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus-an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[26]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS(®)) society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
[30]Hedrick TL, McEvoy MD, Mythen MMG, et al. American society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg. 2018 Jun;126(6):1896-907.
https://journals.lww.com/anesthesia-analgesia/fulltext/2018/06000/american_society_for_enhanced_recovery_and.20.aspx
http://www.ncbi.nlm.nih.gov/pubmed/29293183?tool=bestpractice.com
Os pilares das vias ERAS incluem a cirurgia minimamente invasiva, evitar opioides, controle multimodal da dor, deambulação precoce e ingestão precoce de fluidos e sólidos por via oral.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus-an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[26]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS(®)) society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
[29]Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017 Mar 1;152(3):292-8.
http://www.ncbi.nlm.nih.gov/pubmed/28097305?tool=bestpractice.com
[30]Hedrick TL, McEvoy MD, Mythen MMG, et al. American society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg. 2018 Jun;126(6):1896-907.
https://journals.lww.com/anesthesia-analgesia/fulltext/2018/06000/american_society_for_enhanced_recovery_and.20.aspx
http://www.ncbi.nlm.nih.gov/pubmed/29293183?tool=bestpractice.com
Em pacientes submetidos a cirurgia e que requeiram analgesia com opioides, a diminuição do uso de analgésicos opioides administrados sistemicamente ajuda a prevenir o íleo paralítico pós-operatório.[26]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS(®)) society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
As bombas de analgesia controladas pelo paciente também são benéficas, pois reduzem a quantidade total de opioides administrados em comparação com a administração de analgésicos de forma intermitente ao longo do dia por um enfermeiro.[31]Chan KC, Cheng YJ, Huang GT, et al. The effect of IVPCA morphine on post-hysterectomy bowel function. Acta Anaesthesiol Sin. 2002 Jun;40(2):61-4.
http://www.ncbi.nlm.nih.gov/pubmed/12194392?tool=bestpractice.com
Os adjuvantes úteis para o controle da dor incluem os anti-inflamatórios não esteroidais (AINEs) como o cetorolaco, analgésicos e anestésicos locais administrados por via epidural.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus-an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[32]Senagore AJ, Delaney CP, Mekhail N, et al. Randomized clinical trial comparing epidural anaesthesia and patient-controlled analgesia after laparoscopic segmental colectomy. Br J Surg. 2003 Oct;90(10):1195-9.
http://www.ncbi.nlm.nih.gov/pubmed/14515286?tool=bestpractice.com
[33]Marret E, Remy C, Bonnet F. Meta-analysis of epidural analgesia versus parenteral opioid analgesia after colorectal surgery. Br J Surg. 2007 Jun;94(6):665-73.
https://onlinelibrary.wiley.com/doi/full/10.1002/bjs.5825
http://www.ncbi.nlm.nih.gov/pubmed/17514701?tool=bestpractice.com
[34]Gendall KA, Kennedy RR, Watson AJ, et al. The effect of epidural analgesia on postoperative outcome after colorectal surgery. Colorectal Dis. 2007 Sep;9(7):584-98;discussion 598-600.
http://www.ncbi.nlm.nih.gov/pubmed/17506795?tool=bestpractice.com
[35]Carli F, Trudel JL, Belliveau P. The effect of intraoperative thoracic epidural anesthesia and postoperative analgesia on bowel function after colorectal surgery: a prospective, randomized trial. Dis Colon Rectum. 2001 Aug;44(8):1083-9.
http://www.ncbi.nlm.nih.gov/pubmed/11535845?tool=bestpractice.com
[36]Schlachta CM, Burpee SE, Fernandez C, et al. Optimizing recovery after laparoscopic colon surgery (ORAL-CS): effect of intravenous ketorolac on length of hospital stay. Surg Endosc. 2007 Dec;21(12):2212-9.
http://www.ncbi.nlm.nih.gov/pubmed/17440782?tool=bestpractice.com
[37]Chen JY, Wu GJ, Mok MS, et al. Effect of adding ketorolac to intravenous morphine patient-controlled analgesia on bowel function in colorectal surgery patients: a prospective, randomized, double-blind study. Acta Anaesthesiol Scand. 2005 Apr;49(4):546-51.
http://www.ncbi.nlm.nih.gov/pubmed/15777304?tool=bestpractice.com
[38]McNicol ED, Ferguson MC, Schumann R. Single-dose intravenous ketorolac for acute postoperative pain in adults. Cochrane Database Syst Rev. 2021 May 17;5(5):CD013263.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013263.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/33998669?tool=bestpractice.com
[39]Bell S, Rennie T, Marwick CA, et al. Effects of peri-operative nonsteroidal anti-inflammatory drugs on post-operative kidney function for adults with normal kidney function. Cochrane Database Syst Rev. 2018 Nov 29;11(11):CD011274.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011274.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/30488949?tool=bestpractice.com
[40]Chen JY, Ko TL, Wen YR, et al. Opioid-sparing effects of ketorolac and its correlation with the recovery of postoperative bowel function in colorectal surgery patients: a prospective randomized double-blinded study. Clin J Pain. 2009 Jul-Aug;25(6):485-9.
http://www.ncbi.nlm.nih.gov/pubmed/19542795?tool=bestpractice.com
[51]Guay J, Nishimori M, Kopp SL. Epidural local anesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting, and pain after abdominal surgery: a Cochrane review. Anesth Analg. 2016 Dec;123(6):1591-602.
https://journals.lww.com/anesthesia-analgesia/fulltext/2016/12000/epidural_local_anesthetics_versus_opioid_based.33.aspx
http://www.ncbi.nlm.nih.gov/pubmed/27870743?tool=bestpractice.com
Várias metanálises e ensaios randomizados e controlados mostraram uma diminuição da duração do íleo paralítico pós-operatório em pacientes que receberam goma de mascar após a cirurgia.[58]Yeh YC, Klinger EV, Reddy P. Pharmacologic options to prevent postoperative ileus. Ann Pharmacother. 2009 Sep;43(9):1474-85.
http://www.ncbi.nlm.nih.gov/pubmed/19602600?tool=bestpractice.com
[66]Vasquez W, Hernandez AV, Garcia-Sabrido JL, et al. Is gum chewing useful for ileus after elective colorectal surgery? A systematic review and meta-analysis of randomized clinical trials. J Gastrointest Surg. 2009 Apr;13(4):649-56.
http://www.ncbi.nlm.nih.gov/pubmed/19050983?tool=bestpractice.com
[67]Purkayastha S, Tilney HS, Darzi AW, et al. Meta-analysis of randomized studies evaluating chewing gum to enhance postoperative recovery following colectomy. Arch Surg. 2008 Aug;143(8):788-93.
http://archsurg.ama-assn.org/cgi/reprint/143/8/788
http://www.ncbi.nlm.nih.gov/pubmed/18711040?tool=bestpractice.com
[68]Noble EJH, Harris R, Hosie KB, et al. Gum chewing reduces postoperative ileus? A systematic review and meta-analysis. Int J Surg. 2009 Apr;7(2):100-5.
https://www.sciencedirect.com/science/article/pii/S1743919109000089?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/19261555?tool=bestpractice.com
[69]Fitzgerald JE, Ahmed I. Systematic review and meta-analysis of chewing-gum therapy in the reduction of postoperative paralytic ileus following gastrointestinal surgery. World J Surg. 2009 Dec;33(12):2557-66.
http://www.ncbi.nlm.nih.gov/pubmed/19763686?tool=bestpractice.com
[70]Short V, Herbert G, Perry R, et al. Chewing gum for postoperative recovery of gastrointestinal function. Cochrane Database Syst Rev. 2015;(2):CD006506.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006506.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25914904?tool=bestpractice.com
[71]van den Heijkant TC, Costes LM, van der Lee DG, et al. Randomized clinical trial of the effect of gum chewing on postoperative ileus and inflammation in colorectal surgery. Br J Surg. 2015 Feb;102(3):202-11.
http://www.ncbi.nlm.nih.gov/pubmed/25524125?tool=bestpractice.com
[72]Zhu YP, Wang WJ, Zhang SL, et al. Effects of gum chewing on postoperative bowel motility after caesarean section: a meta-analysis of randomised controlled trials. BJOG. 2014 Jun;121(7):787-92.
http://onlinelibrary.wiley.com/doi/10.1111/1471-0528.12662/full
http://www.ncbi.nlm.nih.gov/pubmed/24629205?tool=bestpractice.com
[73]Andersson T, Bjerså K, Falk K, et al. Effects of chewing gum against postoperative ileus after pancreaticoduodenectomy - a randomized controlled trial. BMC Res Notes. 2015 Feb 10;8:37.
http://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-015-0996-0
http://www.ncbi.nlm.nih.gov/pubmed/25886536?tool=bestpractice.com
Essa é uma modalidade segura e fácil que pode ser utilizada na maioria dos pacientes, porém não é recomendada rotineiramente porque a qualidade da evidência é muito baixa.[26]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS(®)) society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
[74]Pereira Gomes Morais E, Riera R, Porfírio GJ, et al. Chewing gum for enhancing early recovery of bowel function after caesarean section. Cochrane Database Syst Rev. 2016 Oct 17;10(10):CD011562.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011562.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/27747876?tool=bestpractice.com
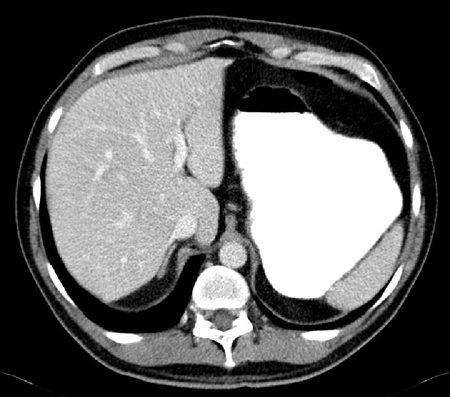
Nos pacientes com distensão abdominal significativa e vômitos repetidos, deve-se colocar uma sonda nasogástrica.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus-an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[30]Hedrick TL, McEvoy MD, Mythen MMG, et al. American society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg. 2018 Jun;126(6):1896-907.
https://journals.lww.com/anesthesia-analgesia/fulltext/2018/06000/american_society_for_enhanced_recovery_and.20.aspx
http://www.ncbi.nlm.nih.gov/pubmed/29293183?tool=bestpractice.com
Deve-se medir o débito gástrico, e o volume perdido deve ser reposto com soro fisiológico intravenoso. A decisão de remover a sonda nasogástrica é baseada no débito medido ao longo do tempo e na resolução clinica do íleo paralítico. O paciente é avaliado quanto a ausência de cólicas e a distensão abdominal, diminuição do débito através da sonda nasogástrica e eliminação de fezes e flatos com o objetivo de se remover a sonda nasogástrica. Pode ser necessário reinserir a sonda nasogástrica, caso o paciente apresente novamente evidências de íleo paralítico continuado, com distensão abdominal e vômitos. No entanto, estudos recentes mostraram que a descompressão nasogástrica rotineira é desnecessária e pode ser prejudicial.[82]Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. 2007 Jul 18;2007(3):CD004929.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6669251
http://www.ncbi.nlm.nih.gov/pubmed/17636780?tool=bestpractice.com
Portanto, o uso rotineiro deixou de ser recomendado, e a descompressão nasogástrica é reservada para uso seletivo.[82]Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. 2007 Jul 18;2007(3):CD004929.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6669251
http://www.ncbi.nlm.nih.gov/pubmed/17636780?tool=bestpractice.com
Frequentemente é realizada descompressão orogástrica no período intraoperatório, mas a sonda é removida ao se concluir a cirurgia.[26]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS(®)) society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
Os pacientes com íleo paralítico pós-operatório prolongado (íleo paralítico no ou após o 4º dia pós-cirurgia, sem resolução prévia do íleo paralítico pós-operatório) podem não conseguir realizar qualquer ingestão oral por várias semanas. A nutrição parenteral é recomendada para os pacientes que não tiverem ingestão oral por mais de 7 dias.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus-an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[76]Gero D, Gié O, Hübner M, et al. Postoperative ileus: in search of an international consensus on definition, diagnosis, and treatment. Langenbecks Arch Surg. 2017 Feb;402(1):149-58.
http://www.ncbi.nlm.nih.gov/pubmed/27488952?tool=bestpractice.com
No entanto, a nutrição parenteral é benéfica nos pacientes que permanecem em repouso intestinal durante mais de 14 dias ou que apresentam desnutrição subjacente.[83]Sandstrom R, Drott C, Hyltander A, et al. The effect of postoperative intravenous feeding (TPN) on outcome following major surgery evaluated in a randomized study. Ann Surg. 1993 Feb;217(2):185-95.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1242758
http://www.ncbi.nlm.nih.gov/pubmed/8439216?tool=bestpractice.com
Deve-se verificar os eletrólitos diariamente para se identificar eventuais anormalidades eletrolíticas associadas à alimentação intravenosa pós-operatória e ao estado de jejum. Os benefícios de se iniciar a nutrição parenteral antes de transcorridos 7 dias são menores que os riscos associados à nutrição parenteral e ao acesso venoso central. Na maioria dos pacientes, o estado de "inanição" pós-operatório não está associado a um aumento da morbidade ou da mortalidade. A inserção de um acesso venoso central está associada a um risco elevado de lesão iatrogênica nos vasos próximos, pneumotórax, trombose venosa profunda (TVP) e bacteremia associada ao acesso central.[Figure caption and citation for the preceding image starts]: Tomografia computadorizada (TC) mostrando estômago significativamente dilatadoDo acervo pessoal da Dra. Paula I. Denoya [Citation ends].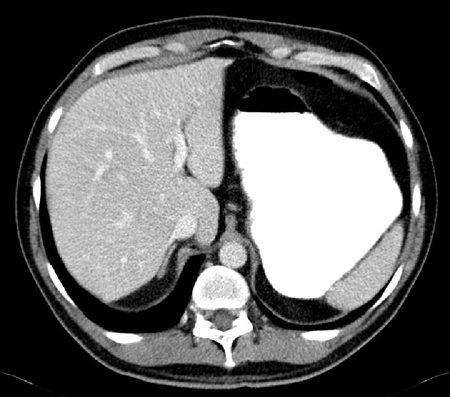 [Figure caption and citation for the preceding image starts]: Sonda nasogástricaDo acervo pessoal da Dra. Paula I. Denoya [Citation ends].
[Figure caption and citation for the preceding image starts]: Sonda nasogástricaDo acervo pessoal da Dra. Paula I. Denoya [Citation ends].
Outras terapias avaliadas
Em pacientes com OID aguda como resultado de adesões, há alguma evidência de que os agentes de contraste hidrossolúveis (por exemplo, gastrografina) são um tratamento eficaz, evitando a cirurgia e estando associados a uma redução no tempo de hospitalização.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus-an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[84]Ceresoli M, Coccolini F, Catena F, et al. Water-soluble contrast agent in adhesive small bowel obstruction: a systematic review and meta-analysis of diagnostic and therapeutic value. Am J Surg. 2016 Jun;211(6):1114-25.
http://www.ncbi.nlm.nih.gov/pubmed/26329902?tool=bestpractice.com
No entanto, dois pequenos ensaios duplo-cegos controlados por placebo em pacientes com íleo paralítico pós-operatório prolongado após cirurgias colorretais eletivas sugerem que a Gastrografin® tem utilidade clínica limitada nesses pacientes, e o valor terapêutico desses tratamentos permanece controverso e incerto.[75]American College of Radiology. ACR Appropriateness Criteria: suspected small-bowel obstruction. 2019 [internet publication].
https://acsearch.acr.org/docs/69476/Narrative
[85]Biondo S, Miquel J, Espin-Basany E, et al. A double-blinded randomized clinical study on the therapeutic effect of gastrografin in prolonged postoperative ileus after elective colorectal surgery. World J Surg. 2016 Jan;40(1):206-14.
http://www.ncbi.nlm.nih.gov/pubmed/26446450?tool=bestpractice.com
[86]Vather R, Josephson R, Jaung R, et al. Gastrografin in prolonged postoperative ileus: a double-blinded randomized controlled trial. Ann Surg. 2015 Jul;262(1):23-30.
http://www.ncbi.nlm.nih.gov/pubmed/25575258?tool=bestpractice.com
Agentes pró-motilidade têm sido utilizados para tratar o íleo paralítico, com sucesso limitado.[62]Traut U, Brügger L, Kunz R, et al. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008;(1):CD004930.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004930.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/18254064?tool=bestpractice.com
Embora a metoclopramida seja útil para o tratamento protelado do esvaziamento gástrico, ela não se mostrou útil com o íleo paralítico pós-operatório quando avaliada em ensaios randomizados e controlados.[87]Cheape JD, Wexner SD, James K, et al. Does metoclopramide reduce the length of ileus after colorectal surgery? A prospective randomized trial. Dis Colon Rectum. 1991 Jun;34(6):437-41.
http://www.ncbi.nlm.nih.gov/pubmed/2036922?tool=bestpractice.com
[88]Seta ML, Kale-Pradhan PB. Efficacy of metoclopramide in postoperative ileus after exploratory laparotomy. Pharmacotherapy. 2001 Oct;21(10):1181-6.
http://www.ncbi.nlm.nih.gov/pubmed/11601663?tool=bestpractice.com
Descobriu-se que a eritromicina intravenosa não é benéfica para o tratamento do íleo paralítico pós-operatório e as evidências são insuficientes para recomendar o uso de medicamentos semelhantes à colecistoquinina, cisaprida, agonistas dopaminérgicos, propranolol ou vasopressina.[62]Traut U, Brügger L, Kunz R, et al. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008;(1):CD004930.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004930.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/18254064?tool=bestpractice.com
[88]Seta ML, Kale-Pradhan PB. Efficacy of metoclopramide in postoperative ileus after exploratory laparotomy. Pharmacotherapy. 2001 Oct;21(10):1181-6.
http://www.ncbi.nlm.nih.gov/pubmed/11601663?tool=bestpractice.com
[89]Lightfoot AJ, Eno M, Kreder KJ, et al. Treatment of postoperative ileus after bowel surgery with low-dose intravenous erythromycin. Urology. 2007 Apr;69(4):611-5.
http://www.ncbi.nlm.nih.gov/pubmed/17445634?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Sonda nasogástricaDo acervo pessoal da Dra. Paula I. Denoya [Citation ends].
[Figure caption and citation for the preceding image starts]: Sonda nasogástricaDo acervo pessoal da Dra. Paula I. Denoya [Citation ends].