Tests
1st tests to order
12-lead ECG
Test
Diagnosis of the various degrees of AV block is frequently made incidental to the workup for any number of presenting conditions.
Symptoms specifically suggestive of AV block prompting a 12-lead ECG include syncope, presyncope, episodic lightheadedness, and progressive exertional fatigue and/or dyspnea. The 12-lead ECG should also be inspected for evidence of acute ischemia (such as ST-segment changes), which may point to a reversible cause of AV block. [Figure caption and citation for the preceding image starts]: First-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].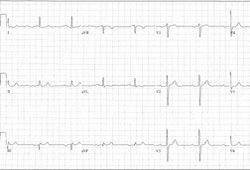 [Figure caption and citation for the preceding image starts]: Type I second-degree AV block. This figure demonstrates typical features of the AV Wenckebach, including progressively shortening R-R intervals as the P-R intervals lengthen; the figure also shows grouped beating, which is also typical for AV WenckebachCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Type I second-degree AV block. This figure demonstrates typical features of the AV Wenckebach, including progressively shortening R-R intervals as the P-R intervals lengthen; the figure also shows grouped beating, which is also typical for AV WenckebachCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Type II second-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Type II second-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].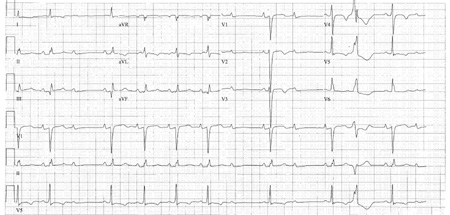 [Figure caption and citation for the preceding image starts]: Third-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Third-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Third-degree heart block: right bundle-branch block escapeCourtesy of Dr Sanjiv Petkar; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Third-degree heart block: right bundle-branch block escapeCourtesy of Dr Sanjiv Petkar; used with permission [Citation ends].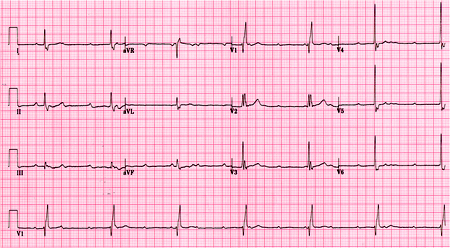
Result
first-degree AV block: fixed PR interval >0.210 seconds (or >210 milliseconds); second-degree AV block, type I: progressive PR interval prolongation, eventual loss of AV conduction for 1 beat, return to normal PR interval, then progressive PR prolongation with eventual loss of AV conduction; second-degree AV block, type II: occasional loss of AV conduction for 1 beat preceded and followed by fixed, unchanging PR intervals; third-degree AV block: no consistent PR relationship
serum troponin
Test
Because acute ischemia should be aggressively managed and presents a potentially reversible cause of AV block, an indicative history and physical exam should prompt the obtaining of serum cardiac enzymes.
Result
may be elevated
serum potassium
Test
Severely abnormal values may represent reversible causes of AV block.
Result
may be very low or very high
serum calcium
Test
Severely abnormal values may represent reversible causes of AV block.
Result
may be very low or very high
serum pH
Test
If severe acidosis or alkalosis is suspected, a serum pH should be obtained. Severely abnormal values may represent reversible causes of AV block.
Result
may be very low or very high
serum digitalis level
Test
If a patient is taking digitalis and presents with new AV block, especially advanced AV block, a serum digitalis level should be obtained. Digitalis toxicity is a reversible cause of AV block. Digitalis toxicity does not necessarily correlate with serum levels. However, an elevated level may increase the suspicion for toxicity.
Result
normal to elevated
Tests to consider
24-hour ambulatory monitoring or event monitoring
Test
24-hour ambulatory monitoring may be helpful in identifying AV block when such a heart block is suspected. An external loop recorder may be used for 2-4 weeks for more frequent symptoms. An implantable loop recording is useful if the 24-hour ambulatory monitoring does not detect AV block, but AV block is still suspected due to symptoms and signs; implantable loop recorders may be used for up to 3 years for less frequent symptoms or unexplained syncope.
Result
evidence of AV block
chest x-ray
Test
Evidence of structural heart disease (e.g., cardiomegaly, or coronary or valvular calcification) or CHF may be present. Hilar lymphadenopathy suggests sarcoidosis. Any number of pulmonary findings may explain hypoxemia, leading to reversible AV block.
There are numerous reasons for a chest radiograph to be ordered, such as the presence of cardiopulmonary symptoms or a high clinical suspicion for heart or lung disease.
Result
may show hilar lymphadenopathy, cardiomegaly, coronary or valvular calcification, or signs of pulmonary congestion
transthoracic echocardiogram
Test
In the setting of advanced heart block, especially if permanent pacemaker placement is considered, a transthoracic echocardiogram should be ordered. The test can demonstrate the presence or absence of structural heart disease and quantify left ventricular systolic function (if ≤35%, biventricular pacemaker with or without implantable cardioverter-defibrillator [ICD] placement should be considered).
Result
may show ventricular dysfunction or hypertrophy, valvular disease, wall-motion abnormalities
serologic testing for Lyme disease
Test
This test should be ordered when the clinical suspicion is high (history, signs, and symptoms support the diagnosis). Because it is a potentially reversible cause, Lyme disease should be considered, especially in younger patients presenting with exposure to endemic areas.
Result
may show positive antibody titer
tilt-table testing
Test
This test can be ordered when AV block is thought to occur in the setting of neurocardiogenic syncope. Neurocardiogenic syncope is a clinical diagnosis, based on patient history, and the sensitivity and specificity of tilt-table testing are widely ranging (30% to 80% and 50% to 90%, respectively).[35]
Result
evidence of AV block
electrophysiology study
Test
This test should be ordered when the severity of conduction disease and the possible need for treatment with a pacemaker are unclear, such as with 2:1 AV block. Significant infranodal conduction disease is defined by a His-bundle-to-ventricle (HV) interval >100 ms.
Result
may show significant infranodal conduction disease
cardiac stress testing
Test
This test should be ordered when a high clinical suspicion exists for cardiac ischemia, outside the acute stages of an acute coronary syndrome.
Active ischemia, especially in the inferior territory, may be a reversible cause of AV block. It can also identify patients with vagotonia who retain chronotropic competence (the ability to appropriately increase heart rate) with exercise. These patients usually do not require a pacemaker.
Infrequently, exercise may show worsening of AV conduction. In such patients, a permanent pacemaker would be indicated.
Result
may show evidence of cardiac ischemia, appropriate increase in heart rate, or worsening of AV conduction
coronary angiography
Test
This test should be ordered when a high clinical suspicion exists for cardiac ischemia, especially in an acute coronary syndrome, when appropriate. Significant obstructive lesions may be reversible, treatable causes of AV block.
Result
may show evidence of significant CAD
serum CK-MB
Test
Less commonly used than troponin. Acute ischemia should be aggressively managed and presents a potentially reversible cause of AV block.
Result
may be elevated
Use of this content is subject to our disclaimer