Etiology
Causes include fibrosis and calcification of the conduction system, coronary artery disease (including patients with a chronic disease and/or an acute coronary syndrome), and medication such as AV-nodal blocking agents (i.e., beta-blockers, calcium-channel blockers, digitalis, adenosine), antiarrhythmic medications such as sodium-channel blockers, and some class III agents (i.e., sotalol and amiodarone).[1][9][10] Additional etiologies include high vagal tone; cardiomyopathy (e.g., hypertrophic, sarcoid, amyloid, hemochromatosis); calcification from adjacent valves; catheter ablation for arrhythmias; cardiac surgery, such as valve repair or replacement, myectomy, or following interventions such as septal ethanol ablation or transcatheter aortic valve insertion; blunt cardiac injury; and some indigenous medicines.[11][12][13] Severe electrolyte disturbances, acidosis, or hypoxemia may result in AV block as well as neuromuscular disorders (myotonic dystrophy, Kearns-Sayre syndrome, Erb dystrophy, peroneal muscular atrophy), myocarditis, infective endocarditis, cardiac tuberculosis, and Lyme disease. AV block may be congenital or associated with complex congenital heart diseases, e.g., atrial septal defects, atrioventricular cushion defects and selected cyanotic congenital heart diseases.[14][15] Inherited progressive cardiac conduction disease in structurally normal hearts in individuals less than 50 years of age is also now well recognized. In one study of patients in Denmark ages <50 years with AV block, the etiology was unknown in 50.3% of patients.[16]
Pathophysiology
Block at the level of the AV node manifesting as first-degree or type I second-degree AV block is usually a function of either high vagal tone or medication. High vagal tone is due to either a tonic elevation (e.g., in younger, athletic patients) or transient vagotonia, as in neurocardiogenic syncope, sleep, nausea, vomiting, or gagging.[17] Transient vagotonia may also result from endotracheal suctioning, micturition or bowel movements, prolonged paroxysms of coughing or other instances of Valsalva, or inferior ischemia or infarction. AV-nodal blocking agents are most commonly beta-blockers, calcium-channel blockers, digitalis, and adenosine. AV block is particularly common when these drugs are used in combination (e.g., digitalis or beta-blockers and calcium-channel blockers).
Block in the His-Purkinje system is usually manifested as type II second-degree AV block or third-degree AV block. His-Purkinje system disease (usually seen as a widened QRS or bundle-branch block on a 12-lead ECG) is usually due to an irreversible structural abnormality that is extensive enough to compromise AV conduction. Because the His-Purkinje system conducts in an all or nothing fashion, AV block at this level will manifest as a consistent PR interval followed by a nonconducted P wave (type II second-degree AV block) or as complete heart block.
Classification
Degrees of block[1]
There are 2 commonly accepted clinical classification systems in use that are not formal classification systems: degrees of block versus anatomic sites of block.
First-degree AV block [Figure caption and citation for the preceding image starts]: First-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].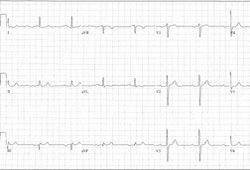
Fixed prolongation of the PR interval >0.2 seconds (or >200 milliseconds) with no failure of AV conduction.
Second-degree AV block, type I [Figure caption and citation for the preceding image starts]: Type I second-degree AV block. This figure demonstrates typical features of the AV Wenckebach, including progressively shortening R-R intervals as the P-R intervals lengthen; the figure also shows grouped beating, which is also typical for AV WenckebachCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].
Progressive prolongation of the PR interval with eventual loss of AV conduction for 1 beat.
Followed by resumption of AV conduction with a progressively prolonging PR interval. The first sinus beat following resumption of AV conduction is conducted with a normal PR interval. Thereafter, there is progressive prolongation of the PR interval.
Eventual loss of AV conduction for 1 beat (pattern repeats, giving rise to group beating).
Second-degree AV block, type II [Figure caption and citation for the preceding image starts]: Type II second-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].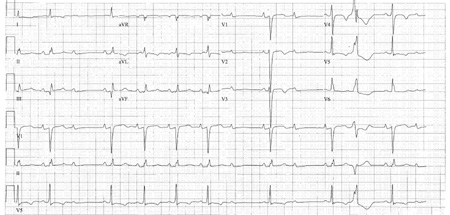
Fixed, unchanging PR intervals.
Then, occasional loss of AV conduction for 1 beat (during sinus rhythm, excluding premature atrial beats).
Finally, fixed, unchanging PR intervals.
Third-degree AV block [Figure caption and citation for the preceding image starts]: Third-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Third-degree heart block: right bundle-branch block escapeCourtesy of Dr Sanjiv Petkar; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Third-degree heart block: right bundle-branch block escapeCourtesy of Dr Sanjiv Petkar; used with permission [Citation ends].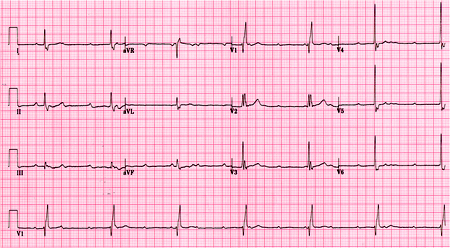
Complete, persistent loss of conduction from the atria to the ventricles.
High-grade AV block
The term high-grade AV block is applied to a pattern where ≥2 sinus P waves block consecutively in the context of periodic AV conduction.
Anatomic sites of block
There are 2 commonly accepted clinical classification systems in use: degrees of block versus anatomic sites of block.
Nodal: at the level of the AV node.
Infranodal: either at the level of the His bundle (intra-His) or below (infra-His).
Use of this content is subject to our disclaimer