Approach
The diagnosis of AV block can be made from any interpretable cardiac rhythm tracing such as a 12-lead ECG, a cardiac telemetry rhythm strip, a Holter-monitor rhythm strip, or an event monitor strip.
History
Patients tend to be male and >50 to 60 years old. Underlying cardiovascular disease (e.g., coronary artery disease or an acute coronary syndrome; hypertension, congestive heart failure; left ventricular hypertrophy or cardiomyopathy; or recent cardiac surgery) may be evident. Other strong risk factors are acid-base disturbance or neuromuscular disease. Infrequently, patients may have a family history of AV block as well. Rarely, Lyme disease is linked to AV block; as a potentially reversible cause, it is important to identify. Clinical evidence of cardiac involvement occurs in 5% of patients with sarcoidosis, although subclinical disease is more often encountered at autopsy. AV block can occur as a result of granulomatous involvement of the interventricular septum or the conduction system. Such patients usually present with syncope at an earlier age than AV block due to other etiologies.[27] Symptoms associated with AV block are fatigue, dyspnea, chest pain, palpitations, and nausea and vomiting. Syncope and presyncope are less commonly associated symptoms most often encountered in emergency care settings.
Physical examination
On examination, patients often have a slow heart rate. If <40 bpm, hospital admission is warranted for pacemaker implantation or temporary transvenous pacing. Blood pressure measurement is crucial. Most often, blood pressure is high with a wide pulse pressure. If blood pressure is low, often ventricular rates are very low (<40 bpm). Low blood pressure is usually seen in an emergency care setting. On examination of jugular venous pressure, if cannon A waves are identified, an irreversible and complete heart block may be present.
Laboratory tests
A 12-lead ECG is essential to identify the type and severity of AV block. It is performed first, and the length and position of the PR interval is key in determining the degree of heart block. Evidence of ischemia, a potential cause of AV block, is also determined on ECG. Serum troponin is drawn initially to verify and track ischemia. CK-MB may be indicated in selected patients. Also drawn immediately are serum potassium, calcium, and digitalis levels, and serum pH, which may identify possible reversible causes of AV block. If a patient may have been exposed to Lyme disease, a serologic test is warranted to rule out this reversible cause of AV block.
Cardiac tracing interpretation
The diagnostic criteria are based on measurement of the PR interval and the presence or absence of nonconducted atrial impulses (no QRS following a P wave). The definitions of the various degrees of block are as follows.
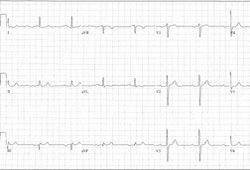
First-degree AV block is fixed prolongation of the PR interval >0.2 seconds (or >200 milliseconds). [Figure caption and citation for the preceding image starts]: First-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].
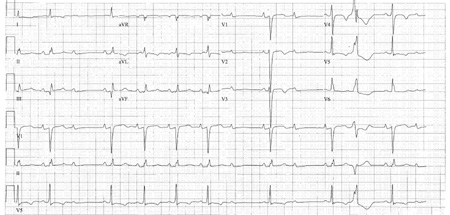
Second-degree AV block, type I, is progressive prolongation of the PR interval with eventual loss of AV conduction for 1 beat, then resumption of AV conduction with a PR interval that progressively prolongs with eventual loss of AV conduction for 1 beat. The pattern repeats, giving rise to group beating. The first sinus beat, following resumption of AV conduction, is conducted with a normal PR interval.[Figure caption and citation for the preceding image starts]: Type I second-degree AV block. This figure demonstrates typical features of the AV Wenckebach, including progressively shortening R-R intervals as the P-R intervals lengthen; the figure also shows grouped beating, which is also typical for AV WenckebachCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].

Second-degree AV block, type II, is the occasional loss of AV conduction for 1 beat (during sinus rhythm, excluding premature atrial beats) preceded and followed by fixed, unchanging PR intervals. [Figure caption and citation for the preceding image starts]: Type II second-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].
Third-degree AV block is complete, persistent loss of conduction from the atria to the ventricles. Also called complete heart block, third-degree heart block shows no consistent PR relationship.[Figure caption and citation for the preceding image starts]: Third-degree AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Third-degree heart block: right bundle-branch block escapeCourtesy of Dr Sanjiv Petkar; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Third-degree heart block: right bundle-branch block escapeCourtesy of Dr Sanjiv Petkar; used with permission [Citation ends].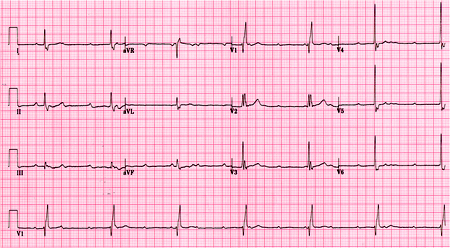
The term high-grade AV block is applied to a pattern where ≥2 sinus P waves block consecutively in the context of periodic AV conduction.
Categorizing 2:1 AV block
One scenario in which the degree of block may be difficult to determine is that of 2:1 AV block. In this case, it is impossible to determine the behavior of the PR interval, whether it progressively prolongs or stays fixed before the nonconducted P wave (absent QRS). Thus, it is difficult to determine the anatomic location of the second-degree AV block: nodal or infranodal. This distinction is important, as the 2 locations imply distinct pathophysiologic processes and prognoses: benign versus potentially malignant, respectively.
Nodal second-degree AV block is suggested during 2:1 AV block when the following feature is present.
Narrow QRS interval: this suggests the His-Purkinje system is intact and thus the level of block is occurring at the level of the AV node.
Up to 30% of infranodal block, however, may be associated with a narrow QRS interval.[34]
Presence of high vagal tone causing AV block is suspected from the following clinical and ECG features.
A slow sinus rate.
Long PR interval with conducted P waves.
Episodes of 2:1 AV block occurring in the following settings: sleep; episodes of nausea, vomiting, or gagging (i.e., endotracheal suctioning); pain; micturition or bowel movements; paroxysmal coughing; or other instances of Valsalva (such as extreme straining to sit up).
Improved frequency of conducted P waves with atropine (with measurable increase in the sinus rate). Caution: giving atropine to patients with infranodal block (usually those with widened QRS complexes at baseline) may worsen the degree of AV block and markedly decrease the ventricular rate. Hence, before giving atropine, consultation with a cardiologist or cardiac electrophysiologist should be considered.
Improved frequency of conducted P waves with exercise (walking around or leg lifts in bed with demonstrable increase in the sinus rate).
Infranodal second-degree AV block is suggested during 2:1 AV block when the following features are present.
Widened QRS interval: this suggests intrinsic disease in the His-Purkinje system. However, up to 30% of infranodal block may be associated with a narrow QRS interval.[34]
Worsened frequency of conducted P waves with exercise (walking around or leg lifts in bed with demonstrable increase in the sinus rate) or with atropine: the His-Purkinje system can demonstrate a fatigue phenomenon with more frequent stimulation (i.e., the higher the sinus rate, the more frequently the His-Purkinje system is stimulated and the worse the frequency of conduction becomes).[Figure caption and citation for the preceding image starts]: 2:1 AV blockCourtesy of Dr Susan F. Kim, Dr John F. Beshai, and Dr Stephen L. Archer; used with permission [Citation ends].

Ambulatory ECG monitoring, imaging, and other tests
A chest x-ray may be helpful in identifying or supporting possible causes of AV block, such as structural heart disease or CHF. A transthoracic echocardiogram aids in identifying or quantifying structural heart disease. This test is necessary if a permanent pacemaker is considered possible. 24-hour ambulatory monitoring may be helpful in identifying AV block when such a heart block is suspected. An external loop recorder may be used for 2-4 weeks for more frequent symptoms. An implantable loop recording is useful if the 24-hour ambulatory monitoring does not detect AV block, but AV block is still suspected due to symptoms and signs; implantable loop recorders may be used for up to 3 years for less frequent symptoms or unexplained syncope. If AV block is thought to occur as a result of neurocardiogenic syncope, tilt-table testing is suggested. If the severity of AV block is unknown and the need for a pacemaker is still unclear, an electrophysiology study may help identify the AV block. Cardiac stress testing is warranted when cardiac ischemia or exercise-induced AV block is likely. Especially in the setting of an acute coronary syndrome and cardiac ischemia, coronary angiography will help identify obstructive lesions, which, when treated, may help in reversing heart block.
Use of this content is subject to our disclaimer