History and exam
Key diagnostic factors
common
presence of risk factors
history of mechanical trauma
Significant historical findings that are warning features for serious injury include: fall from a height of >3 m (>10 feet), and motor vehicle accidents (MVA) at speeds of >96 km/h (>60 mph) with ejection from vehicle or evidence of the seat belt sign on the front trunk of patient, which is associated with lumbar Chance fracture.[51]
past medical history of osteoporosis or neoplasm
Most isolated fractures of thoracic and lumbar vertebrae are related to osteoporosis.[11][13][27] Trauma is often associated with lower energy injuries. Various neoplastic processes (e.g., metastasis, multiple myeloma) can infiltrate and weaken the bone to the extent that it may not withhold normal physiological loads. Consequently, the vertebrae will fracture when subjected to small trivial forces, such as simple falls or movements. [Figure caption and citation for the preceding image starts]: MRI thoracic spine: sagittal view (T2-weighted sequence) showing a pathological fracture of the T10 vertebral body caused by multiple myelomaFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].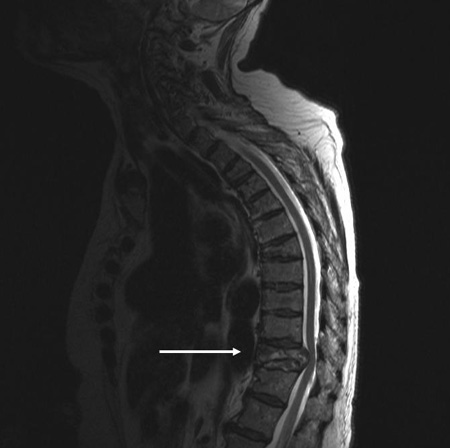 [Figure caption and citation for the preceding image starts]: MRI lumbar spine: sagittal view (T2-weighted sequence) showing an osteoporotic fracture of the T12 vertebral bodyFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI lumbar spine: sagittal view (T2-weighted sequence) showing an osteoporotic fracture of the T12 vertebral bodyFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].
back pain
bruising
Bruising may correlate with the level of spinal column injury.[56]
acute numbness/paraesthesia
May occur due to compression of the spinal cord or nerve root(s).
Careful clinical assessment of the level of neurological injury, including dermatomal distribution of sensation, is necessary for optimal analysis of radiological images.
The neurological injury level is defined as the most caudal segment of the spinal cord with normal sensory function on both sides.
Simultaneous right/left evaluation of individual dermatome sensation is likely to improve sensitivity in sensation function assessment.[65]
weakness
May be due to compression of the spinal cord or nerve root(s).
Careful clinical assessment of the level of neurological injury, including muscle weakness pattern, is necessary for optimal analysis of radiological images.
The neurological injury level is defined as the most caudal segment of the spinal cord with normal motor function on both sides.[65]
muscle spasticity/clonus (hypertonicity) or hypotonia
Muscle spasticity is suggestive of an upper motor neuron lesion, while hypotonia or flaccidity is suggestive of spinal shock (as a temporary feature) or a lower motor neuron lesion.
Clonus is said to be abnormal if the foot flexes involuntarily for >3 beats when that foot is forcefully extended. Abnormal clonus suggests upper motor neuron lesion.[65]
hyperreflexia or hyporeflexia
Increased reflexes are suggestive of an upper motor neuron lesion.
Reduced reflexes (or areflexia) are suggestive of a lower motor neuron lesion or hyper-acute spinal cord injury.
Hoffman's sign
Flicking of the nail bed of the middle finger results in a sudden twitch of the other fingers ipsilaterally. Presence of the Hoffman's sign is suggestive of an upper motor neuron lesion related to cervical spinal cord compression.[65]
positive Babinski's sign
Forceful stroking of the lateral or plantar aspect of the foot causes extension of the big toe and fanning out of the other toes ipsilaterally. A positive Babinski's sign is suggestive of an upper motor neuron lesion.[65]
uncommon
spinal deformity
A step deformity or swelling over the spine indicates the likely level of injury.
loss of anal sphincter reflex
Indicates higher-severity spinal cord injury.[65]
Other diagnostic factors
uncommon
absence of bulbocavernosus reflex (S3-S4)
The bulbocavernosus reflex is subserved by S4-S5 nerve root and elicited by squeezing the glans penis or pulling gently on the bladder indwelling catheter. The absence of this reflex indicates that spinal shock is likely present and precludes definitive evaluation about completeness of spinal cord injury.[11] The return of the bulbocavernosus reflex heralds the end of spinal shock. Absence of this reflex may also indicate sacral spinal cord injury or injury to sacral roots.[65]
signs of spinal shock (hypotonia or flaccidity that resolves within 24 hours)
Exhibited as a temporary feature of a lower motor neuron injury due to spinal cord impairment. Disrupts all cord functions below the level of injury, including reflexes (presence of reflexes indicates absence of spinal shock).[11] Usually resolves within 24 hours of injury (prognosis of neurological recovery is not reliable for this time period). Predictions regarding functional recovery are more reliable when based on neurological examinations 72 hours to 1 week after trauma than if based on examinations within the first 24 hours.[55]
Spinal shock is not usually considered as a limiting factor to making the decision about operative or peri-operative treatment. If a patient needs urgent spinal decompression, waiting for 72 hours for spinal shock to subside completely may be detrimental.
urinary incontinence
Usually due to high spinal level injury causing damage to the spinal cord. The impairment of the inhibitory modulation of the descending fibres will cause the bladder to contract at small bladder volumes, resulting in incontinence (hypertonic bladder). In addition, high spinal level injuries may lead to urinary retention with overflow incontinence in the acute period, and this will be painless if the injury is complete.[65]
painless urinary retention
If patients have no sense of a full bladder, this is suggestive of injury within the cauda equina. Nerves from the cauda equina supply the bladder, and injury to them causes urinary retention. Overflow incontinence may result.[65]
Risk factors
strong
falling from a height
Typically causes compression fractures.
high-energy mechanism of injury
Any high-energy mechanism may result in spinal trauma. Examples include high-speed motor vehicle collisions (especially when associated with ejection or rollover); motorcycle, bicycle, and recreational vehicle collisions; crush injuries; falls from height; injuries leading to an axial load to the head (e.g., diving and auto versus pedestrian).[11][14][38]
age >65 years
Older patients may present with thoracolumbar fractures as a result of low-energy trauma, for example, simple falls from standing, due to diminished bone mineralisation commonly present in older patient populations and the presence of underlying conditions, for example, osteoporosis and osteopenia, rheumatoid arthritis, diffuse idiopathic skeletal hyperostosis, and neoplasia).[9][10][11] Falls are about 2.8 times more likely to cause injury in older people (aged >65 years) than in the younger population (aged <65 years).[16]
concomitant osteoporosis
Most isolated fractures of thoracic and lumbar vertebrae are related to osteoporosis.[11][27] Trauma is often associated with lower-energy injuries.[Figure caption and citation for the preceding image starts]: MRI lumbar spine: sagittal view (T2-weighted sequence) showing an osteoporotic fracture of the T12 vertebral bodyFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].
previous vertebral fracture
underlying neoplastic lesion
Various neoplastic processes (e.g., metastasis, multiple myeloma) can infiltrate and weaken the bone to the extent that it may not withhold normal physiological loads. Consequently, the vertebrae will fracture when subjected to small trivial forces, such as simple falls or movements.[Figure caption and citation for the preceding image starts]: MRI thoracic spine: sagittal view (T2-weighted sequence) showing a pathological fracture of the T10 vertebral body caused by multiple myelomaFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].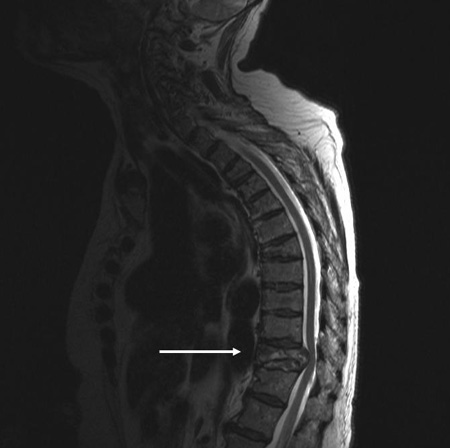
underlying metabolic or inflammatory disorders
Osteogenesis imperfecta, osteoporosis, rheumatoid arthritis, and ankylosing spondylitis are examples of metabolic or inflammatory disorders that increase the risk of thoracolumbar spine trauma.[11][Figure caption and citation for the preceding image starts]: MRI lumbar spine: sagittal view (T2-weighted sequence) showing an osteoporotic fracture of the T12 vertebral bodyFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].
Use of this content is subject to our disclaimer