Case history
Case history #1
A 23-year-old man is taken to the emergency department following a road traffic accident. History from witnesses reveals that he was hit by a car travelling at 48 km/h (30 mph) while he was crossing the road. On examination, the patient is alert and haemodynamically stable, and describes numbness in both legs. He is able to move his lower limbs sideways but not against gravity (suggesting a power of 2/5). Lower-limb reflexes are diminished. On examination of his abdomen, his bladder is palpable; therefore, a urinary catheter is inserted. He states that he did not feel an urge to urinate and claims he cannot feel the catheter in situ.
Case history #2
A 73-year-old man presents to the emergency department after falling off a roof 5 m (16 feet) high. He landed on his back, and he has excruciating pain in his mid-thoracic spinal level, which is limiting his movements. On examination, tone, power, coordination, and sensation are normal. Reflexes are present, equal, and symmetrical, with negative Babinski's sign.
Other presentations
Older patients, particularly postmenopausal women, make up a minority of thoracolumbar spine trauma patients. They often present following a trivial fall while walking, which results in an osteoporotic fracture of the thoracolumbar spine.[9][10][11] If thoracolumbar fractures occur in younger people with mild trauma, an underlying sinister cause, such as neoplasia (e.g., bony metastasis, multiple myeloma) or metabolic disorders, must be excluded.[11] Often, pathological fractures are preceded by other clinical features such as progressive back pain, deformity, or neurological deficit.[Figure caption and citation for the preceding image starts]: MRI thoracic spine: sagittal view (T2-weighted sequence) showing a pathological fracture of the T10 vertebral body caused by multiple myelomaFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].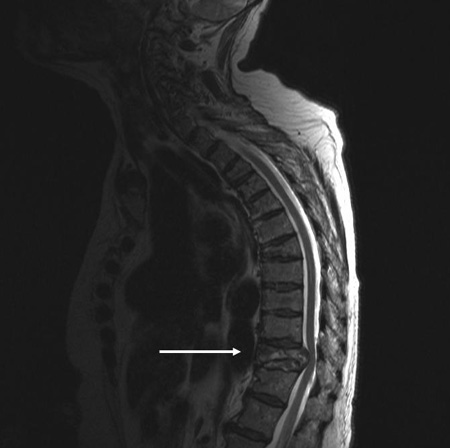
Use of this content is subject to our disclaimer