Aetiology
The aetiology of traumatic thoracolumbar fractures includes:
Motor vehicle accidents (accounts for >30% of fractures)[12]
Falls; approximately three times more likely to cause fracture in older adults (age >65 years) than in the younger population (accounts for 30% of fractures)[16]
Sports; for example, diving (accounts for 10% of fractures)[12][32]
Gunshot injuries (accounts for 15% of fractures).[33]
If fractures occur in younger people with mild trauma, an underlying sinister cause, such as neoplasia (e.g., bony metastasis, multiple myeloma) or metabolic disorders, must be excluded.[Figure caption and citation for the preceding image starts]: MRI thoracic spine: sagittal view (T2-weighted sequence) showing a pathological fracture of the T10 vertebral body caused by multiple myelomaFrom the personal collection of Dr B. Nurboja and Mr D. Choi [Citation ends].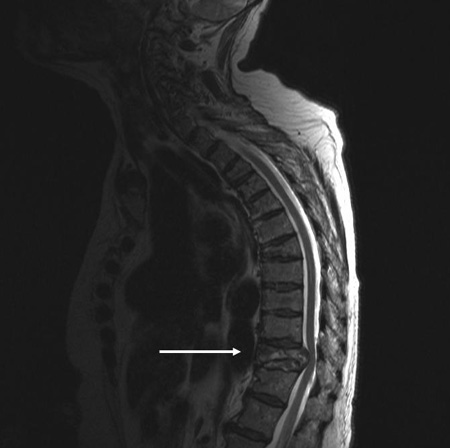
Pathophysiology
Thoracolumbar fractures are breakages in the vertebrae of the spinal column in the thoracic and lumbar regions. They may be associated with disruption of the ligamentous complexes, and can result in instability or compression of neural structures.
Kinematics
Understanding the kinematics (or physiological motion allowed within the constraints of anatomy) of the thoracolumbar spine and the forces acting on it aids understanding of the ways in which thoracolumbar fractures occur.
The thoracic spine is much stiffer than the lumbar spine in sagittal and lateral flexion-extension, due to the rib cage exerting a restraining effect, and also because of thinner discs. However, rotation about the craniocaudal axis is greater in the thoracic spine (75°) than in the lumbar spine (10°) because of the positioning of the facets. The range of movements of the spine decreases with age.[34]
The three excessive movements that may cause fracture, either alone or in combination, include translation (forwards, lateral, or backwards), rotation, and shear.
Nature of damage
It has been shown that anterior column disruption decreases the load-carrying capacity of the thoracolumbar spine by 30%, while disruption of the posterior column alone reduces the load-carrying capacity of the thoracolumbar junction by 25%.
Disruption of the middle column with the anterior column reduces the load-carrying capacity of the spine by 70%, and with posterior column disruption the reduction of load-carrying capacity is 65%.[35]
The disruption of the annulus diminishes rotatory stability by 80%, while disruption of the facet joints diminishes rotatory stability by 20%.[36]
The underlying processes of the different types of fractures are due to supraphysiological forces acting on various spinal columns.
Compression fractures: loading axial and flexion forces act on the anterior column; bony fragments are not dispersed.
Burst fractures: axial forces (with or without flexion or rotation forces) act on the anterior and middle columns with or without posterior column involvement; bony fragments are moved away from each other.
Wedge fractures: loading forces act on the anterior column while in flexion.
Dislocation fractures: usually occur due to translation forces severely disrupting the disc, facet joints, and ligamentous complex, resulting in complete displacement of the adjacent vertebrae; this always leads to complete disruption of the spinal cord.
Fracture stability is important, as unstable fractures are known to lead to paralysis, loss of sensation, and loss of sphincter control. Any suspected thoracolumbar fracture should be treated as unstable until confirmed otherwise.
Unstable fractures are those with disruption of the ligaments, or with movement of vertebral bodies in relation to each other.
Magnetic resonance imaging scan of the spine (with flexion-extension view) is used to assess fracture stability.
The pathophysiology of the consequences of thoracolumbar spine trauma varies.
Spinal shock: immediate depolarisation of the axonal membranes, from the kinetic energy of the injury to the spinal cord, causes temporary features of a lower motor neuron injury, due to injured spinal cord impairment.[37]
Urinary incontinence: impairment of the inhibitory modulation of descending fibres causes the bladder to contract at small bladder volumes, which leads to hypertonic bladder and incontinence.
Classification
Thoracolumbar Arbeitsgemeinschaft für Osteosynthesefragen Spine injury score (TL AOSIS)[1]
Compression injuries
AO: Minor, non-structural
A1: Wedge compression
A2: Split
A3: Incomplete burst
A4: Complete burst.
Distraction injuries
B1: Transosseus tension band disruption/Chane fracture
B2: Posterior tension band disruption
B3: Hyperextension.
Translational injuries/displacement or dislocation
Published in 2013, the updated AOSpine classification merges key elements of the AO-Magerl classification and the Thoracolumbar Injury Classification and Severity Score. It incorporates both fracture morphology and clinical factors relevant for clinical decision-making.
AO thoracolumbar classification system[2]
This Swiss system classifies thoracolumbar fractures into three major groups, based on the mechanism of injury:
A. Compression (NOTE: posterior soft tissue must be intact even if there is some posterior element fracture)
A1: Wedge
A2: Split or coronal
A3: Burst.
B. Distraction
B1: Distraction of the posterior soft tissues (subluxation)
B2: Distraction of the posterior arch (Chance fracture)
B3: Distraction of the anterior disc (extension spondylolysis).
C. Multi-directional with translation
C1: Anterior-posterior (dislocation)
C2: Lateral (lateral shear)
C3: Rotational (rotational burst).
The AO classification provides a comprehensive classification describing the nature of injury, the degree of instability, and prognostic aspects that are important for choosing the most appropriate treatment.
Denis classification[3]
This classification system involves the division of the spinal column into anterior, middle, and posterior columns and the definition of different fracture types.
The anterior column includes the anterior halves of the vertebral bodies and the anterior longitudinal ligament.
The middle column includes the posterior halves of the vertebral bodies and the posterior longitudinal ligament.
The posterior column includes the facet joints, pedicles, and supraspinous ligaments.
[Figure caption and citation for the preceding image starts]: Denis definitions of types of spinal fractureContent adapted by author from Denis F. The three-column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983 Nov-Dec;8(8):817-31 [Citation ends].
Compression fractures are classified according to whether they are caused by anterior or lateral flexion. These injuries cause anterior column compression and sometimes associated posterior column distraction.
Burst fractures are classified according to whether the fracture was caused by an axial load alone, or whether flexion, rotation, or lateral flexion was also involved. These injuries cause anterior and middle column compression, and may sometimes also produce associated posterior column distraction.
Seat belt fractures are defined by their distinctive flexion-disruption mechanism of injury. The anterior column may be intact or distracted, but the middle and posterior columns are distracted.
Fracture-dislocations are classified according to whether the dislocation involves rotation, shear, or flexion-distraction. These injuries can produce any pattern of column involvement.
[Figure caption and citation for the preceding image starts]: Denis classification of spinal fractureCreated by BMJ using content by Dr B. Nurboja and Mr D. Choi [Citation ends].
Thoracolumbar Injury Classification and Severity Score (TLICS)[4]
This classification system for thoracolumbar fractures, also known as the Thoracolumbar Injury Severity Score (TLISS), was devised by the Spine Trauma Study Group (STSG) and has been validated and shown to have good reliability.[4][5][6]
It is a composite scoring system based on three injury components: 1) morphology of injury determined by radiographic appearance; 2) integrity of the posterior ligamentous complex; and 3) neurological status of the patient.
Injury morphology
Compression fracture: 1 point
Compression fracture plus burst: 2 points
Translational/rotational fracture: 3 points
Distraction fracture: 4 points
Disruption of posterior ligamentous complex
Intact: 0 points
Suspected/indeterminate: 2 points
Injured: 3 points
Neurological status
Intact: 0 points
Nerve root: 2 points
Cord, conus medullaris
Complete: 2 points
Incomplete: 3 points
Cauda equina: 3 points
A score of ≤3 suggests a non-operative management, while a score of ≥5 suggests that surgical intervention may be considered. A score of 4 might be handled conservatively or surgically.
This classification system also provides a guide for determining the optimal approach (anterior, posterior, combined anterior-posterior) for surgically treated patients based on: 1) disruption of the posterior ligamentous complex; and 2) neurological status.
Posterior approach
Neurological status: intact or root injury
Posterior ligamentous complex: intact or disrupted
Anterior approach
Neurological status: incomplete spinal cord injury or cauda equina
Posterior ligamentous complex: intact
Combined approach
Neurological status: incomplete or complete spinal cord injury or cauda equina
Posterior ligamentous complex: intact or disrupted
Holdsworth classification[7]
This classification pre-dates the modern imaging modalities and is no longer used.
Two-column model with anterior column, consisting of the structures ventral to the posterior longitudinal ligament, and posterior column, made up of structures dorsal to the posterior longitudinal ligament.
Fractures are further classified as wedge, rotational fracture-dislocation, extension dislocation, and vertebral compression burst fractures.
Ferguson and Allen classification[8]
This classification is of historical interest only and is no longer used.
Thoracolumbar spinal injuries are classified on the basis of the mechanical mode of failure of the vertebral bodies.
The choice of instrumentation for surgery is based on the surgeon's understanding of these injury patterns.
Use of this content is subject to our disclaimer