Last reviewed: 16 Mar 2025
Last updated: 21 Jan 2025
Summary
Definition
History and exam
Key diagnostic factors
- presence of risk factors
- history of mechanical trauma
- past medical history of osteoporosis or neoplasm
- back pain
- bruising
- acute numbness/paraesthesia
- weakness
- muscle spasticity/clonus (hypertonicity) or hypotonia
- hyperreflexia or hyporeflexia
- Hoffman's sign
- positive Babinski's sign
- spinal deformity
- loss of anal sphincter reflex
Other diagnostic factors
- absence of bulbocavernosus reflex (S3-S4)
- signs of spinal shock (hypotonia or flaccidity that resolves within 24 hours)
- urinary incontinence
- painless urinary retention
Risk factors
- falling from a height
- high-energy mechanism of injury
- age >65 years
- concomitant osteoporosis
- previous vertebral fracture
- underlying neoplastic lesion
- underlying metabolic or inflammatory disorders
Diagnostic investigations
Investigations to consider
- thoracolumbar spine x-ray (anterior-posterior and lateral views)
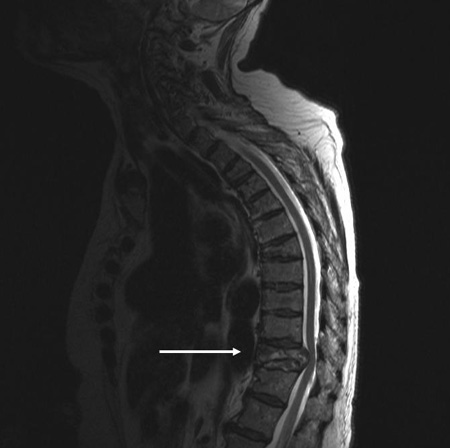
- MRI spine
- CT myelography
- MRI with STIR sequence
- Whole body CT
Treatment algorithm
Contributors
Authors
Besnik Nurboja, BSc, MBBS, MD (Res), MRCS, FRCEM
Consultant in Emergency Medicine
Emergency Medicine
Epsom and St Helier University Hospital NHS Trust
London
UK
Disclosures
BN declares that he has no competing interests.
David Choi, FRCS(SN)

Consultant Neurosurgeon and Spinal Surgeon
The National Hospital for Neurology and Neurosurgery
London
UK
Disclosures
DC declares that he has no competing interests.
Peer reviewers
Byron F. Stephens, MD, MSCI
Associate Professor
Vanderbilt University School of Medicine
Nashville
TN
Disclosures
BFS has received Institutional Research Support from Nuvasive and Stryker.
Use of this content is subject to our disclaimer