Focal atrial tachycardia
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
adult: undifferentiated supraventricular tachycardia
adenosine
Causes AV node blockade with slowing of the ventricular response rate or cessation of the atrial tachycardia.[13]Innes JA. Review article: adenosine use in the emergency department. Emerg Med Australas. 2008 Jun;20(3):209-15.
http://www.ncbi.nlm.nih.gov/pubmed/18549383?tool=bestpractice.com
Effects are transient, and can be misleading when trying to differentiate from other forms of supraventricular tachycardia, if the focal AT terminates with adenosine.[Figure caption and citation for the preceding image starts]: Response to adenosine 6 mg intravenouslyFrom the collection of Sarah Stahmer, MD [Citation ends].
Transient slowing of the ventricular response rate with sustained atrial activity indicates flutter or focal AT. Flutter will have the characteristic saw-tooth pattern of an atrial macro-re-entrant circuit. Focal AT will show discrete P waves with an isoelectric baseline.
Lack of response to adenosine suggests either sinus tachycardia or focal AT, and strongly suggests that the rhythm is not re-entrant supraventricular tachycardia or atrial flutter.
Some forms of atrial tachycardia will break in response to adenosine.[17]Engelstein ED, Lippman N, Stein KM, et al. Mechanism-specific effects of adenosine on atrial tachycardia. Circulation. 1994 Jun;89(6):2645-54. http://www.ncbi.nlm.nih.gov/pubmed/8205677?tool=bestpractice.com
Primary options
adenosine: adults: 6 mg/dose intravenously initially, followed by 12 mg/dose in 1-2 minutes if no effect, may repeat 12 mg/dose once more in 1-2 minutes if no effect, maximum 30 mg/total dose
adult: focal AT; digoxin excess not suspected
beta-blocker or calcium-channel blocker
Calcium-channel blockers or beta-blockers may be helpful in controlling the ventricular response rate or breaking the tachycardia.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115. http://content.onlinejacc.org/article.aspx?articleid=2443667 http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com
Catecholamine excess should be suspected if there is a history or suspicion of recent use of exogenous catecholamines, cocaine, or alcohol with clinical features of catecholamine excess (agitation, diaphoresis, hypertension).
Supportive care and withdrawal of any offending agent are first-line therapy. Supportive care includes intravenous fluids for any haemodynamic instability without overt congestive heart failure, as well as correction of any associated electrolyte imbalance.
Beta-blockers should be used with caution if there is a suspicion that the dysrhythmia was triggered by cocaine.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115.
http://content.onlinejacc.org/article.aspx?articleid=2443667
http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in a 35-year-old with history of recent cocaine useFrom the collection of Sarah Stahmer, MD [Citation ends].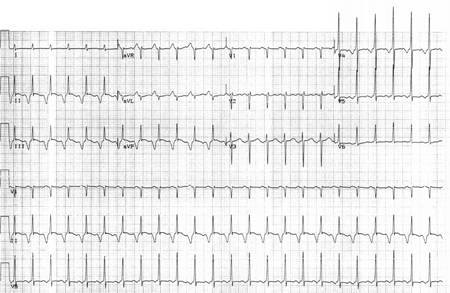
Blocking the beta receptors leaves the circulating noradrenaline (norepinephrine) free to activate the alpha receptors with no opposing beta effects. This may induce hypertensive crisis and vasospasm.
Beta-blockers are generally reserved for patients who are not suspected to have taken cocaine, and who are refractory to supportive care, show evidence of cardiac ischaemia, or are haemodynamically unstable.
The effects of any pharmacological intervention for focal AT are often unpredictable given the multitude of causes and underlying mechanisms. For this reason, if there are any concerns about the potential risks of giving an agent to a stable patient, choose agents that are short acting and can be stopped if there are adverse effects.
Beta-blockers and calcium-channel blockers should be avoided in patients with decompensated heart failure or haemodynamic instability. Beta-blockers should also be avoided in patients with active pulmonary disease.
Primary options
diltiazem: adults: 0.25 mg/kg intravenously initially, followed by 10 mg/hour infusion, consult specialist for further guidance on dose
OR
esmolol: adults: 500 micrograms/kg/dose intravenously initially, followed by 50 micrograms/kg/minute infusion for 4 minutes, if no response after 5 minutes repeat loading dose and increase infusion, consult specialist for further guidance on dose
Secondary options
verapamil: adults: 5-10 mg intravenously initially, followed by 10 mg 30 minutes later if no effect, consult specialist for further guidance on dose
OR
metoprolol: adults: 5 mg/dose intravenously initially, may repeat every 5 minutes, maximum 3 doses
catheter ablation
Electrophysiological study involving ablation may aid in diagnosing the mechanism of the tachycardia; it can be curative and may be offered as first-line therapy to select patients.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115. http://content.onlinejacc.org/article.aspx?articleid=2443667 http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com
The need to confirm the mechanism of SVT and preference for an alternative to long-term pharmacological therapy are factors that may support the use of catheter ablation.
Catheter ablation is a specialised intervention undertaken by electrophysiologists and may be dependent on availability of an electrophysiologist.
amiodarone or ibutilide
Patients who are refractory or have contraindications to adenosine, beta-blockers, or calcium-channel blockers may benefit from these second-line medications.
Amiodarone is a highly effective agent in the management of a wide range of supraventricular and ventricular tachycardias.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115. http://content.onlinejacc.org/article.aspx?articleid=2443667 http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com It prolongs the duration of the action potential and the refractory period in atrial and ventricular tissues, slows automaticity in pacemaker cells, and slows AV nodal conduction. Patients should, therefore, be closely monitored when this treatment is started.
Ibutilide has been reported to be effective in some cases of focal AT, but its mechanism of action is not clear.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115. http://content.onlinejacc.org/article.aspx?articleid=2443667 http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com [16]Brugada J, Katritsis DG, Arbelo E, et al. 2019 ESC guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020 Feb 1;41(5):655-720. https://academic.oup.com/eurheartj/article/41/5/655/5556821 http://www.ncbi.nlm.nih.gov/pubmed/31504425?tool=bestpractice.com Continuous ECG monitoring is recommended and caution should be used in patients with QT prolongation.
Primary options
amiodarone: adults: 150 mg intravenously over 10 minutes, followed by 1 mg/minute infusion over 6 hours (total dose 360 mg), then 0.5 mg/minute infusion over 18 hours (total dose 540 mg)
OR
ibutilide: adults body weight <60 kg: 0.01 mg/kg intravenously as a single dose; adults body weight ≥60 kg: 1 mg intravenously as a single dose; may repeat dose after 10 minutes if no response
third-line pharmacotherapy or direct current (DC) cardioversion + cardiology consult
Patients who are refractory to second-line pharmacotherapy should be referred for a cardiology consult. Cardioversion may be effective in some cases; usually if re-entry is the mechanism. Other forms of focal AT are often resistant to electrical disruption. Medications that may be effective are in the Ic class of anti-arrhythmics. Because of the risk of untoward side effects with these medications, cardiology consultation is advised when considering these therapies.
Primary options
flecainide: adults: 50 mg orally every 12 hours initially, increase gradually according to response, maximum 300 mg/day
OR
propafenone: adults: 150 mg orally (immediate-release) every 8 hours initially, increase gradually according to response, maximum 900 mg/day; 225 mg orally (extended-release) every 12 hours initially, increase gradually according to response, maximum 850 mg/day
direct current (DC) cardioversion
Electrical disruption may be effective in some cases of focal AT. When a patient has become unstable, it is reasonable to attempt DC cardioversion when it is clear that the tachyarrhythmia is non-sinus and is responsible for the haemodynamic compromise.
Electrical disruption is usually only effective if re-entry is the mechanism; other forms of focal AT are typically resistant to electrical disruption.
If an underlying cause is identified, this should be treated.
adult: focal AT; digoxin toxicity suspected
supportive care
Digoxin toxicity should be suspected if there is a history of congestive heart failure, the patient is taking digoxin, and the rhythm is atrial tachycardia with evidence of atrio-ventricular blockade.
When atrial tachycardia is a manifestation of digoxin toxicity, treatment is aimed at supportive care, withholding digoxin, optimising volume status, and replacing potassium if there is a deficit.[Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in an 88-year-old woman with 2:1 AV nodal block in the setting of digoxin therapy and potassium 2.8 mmol/L (2.8 mEq/L)From the collection of Sarah Stahmer, MD [Citation ends].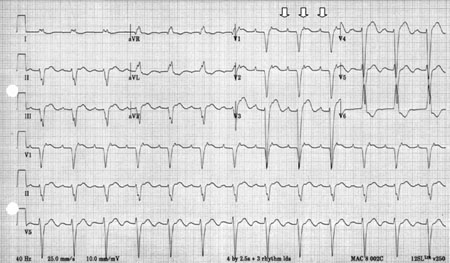
This approach is usually sufficient for restoring sinus rhythm.
digoxin immune Fab
Additional treatment recommended for SOME patients in selected patient group
Patients with evidence of refractory arrhythmias, particularly ventricular, or haemodynamically compromising AV block may benefit from digoxin-specific antibody fragments (Fab) therapy to bind digoxin.[19]Antman EM, Wenger TL, Butler VP Jr, et al. Treatment of 150 cases of life-threatening digitalis intoxication with digoxin-specific Fab antibody fragments: final report of a multicenter study. Circulation. 1990 Jun;81(6):1744-52. http://www.ncbi.nlm.nih.gov/pubmed/2188752?tool=bestpractice.com
Primary options
digoxin immune Fab: adults: consult specialist for guidance on dose
child
anti-arrhythmic medication ± catheter ablation
Paediatric atrial tachycardias are uncommon. Atrial tachycardia in children is often incessant and refractory to typical treatments used for atrioventricular nodal re-entrant tachycardia; tachycardia-induced cardiomyopathy is commonly observed.
The treatment of paediatric patients with atrial tachycardia includes medications to suppress the arrhythmia and/or control the ventricular response and catheter ablation. Beta-blockers, digoxin, and antiarrhythmics such as amiodarone are often effective as first-line pharmacological interventions to achieve rate control. Many children will have spontaneous resolution of the arrhythmia.
Amiodarone should not be used in babies aged <1 month because of the additive benzyl alcohol, which may precipitate metabolic acidosis and gasping syndrome.[20]Perry J, Fenrich AL, Hulse JE, et al. Pediatric use of amiodarone: efficacy and safety in critically ill patients from a multicenter protocol. J Am Coll Cardiol. 1996 Apr;27(5):1246-50. http://www.ncbi.nlm.nih.gov/pubmed/8609351?tool=bestpractice.com
Patients with incessant tachycardias will usually require catheter ablation, which is associated with a high degree of success, a low complication rate, and a low recurrence rate.
Selection of drug therapy in children should be under specialist guidance.
adult: sustained or recurrent focal AT
catheter ablation
Many patients with sustained and/or recurrent atrial tachycardias are referred for catheter ablative therapy. The success of this treatment depends on the site of origin and underlying mechanism.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115. http://content.onlinejacc.org/article.aspx?articleid=2443667 http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com The presence of recurring symptoms, persistent tachycardia leading to heart failure, and unsuccessful medical treatment, are factors that may support the use of catheter ablation for focal atrial tachycardia.
Catheter ablation is a specialised intervention undertaken by electrophysiologists and may be dependent on availability of an electrophysiologist.
antiarrhythmic medication
There is limited evidence that these drugs are moderately effective for the long-term pharmacological therapy of focal AT. Most of the evidence for the long-term use of these drugs in the management of focal AT come from studies in children. Due to the risk of pro-arrhythmia and other potential complications it is important to consider individual benefit versus harm.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115. http://content.onlinejacc.org/article.aspx?articleid=2443667 http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com Class Ic or class III antiarrhythmics are typically used in this setting. Consult a specialist for guidance on selection and dose of antiarrhythmics.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer