Aetiology
Focal atrial tachycardia (focal AT) has a variety of causes. It may occur in healthy people, although often there is underlying cardiac pathology.[1][4][5] Associated conditions include cardiomyopathies, ischaemic heart disease, previous cardiac surgery, cardiac ablation, and hyperthyroidism.
People without cardiac pathology may develop this rhythm in the setting of exogenous stimulants such as amphetamines, cocaine, and acute alcohol intoxication. Focal AT is the classic presenting rhythm in patients with digoxin toxicity and is typically associated with AV nodal block.[Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in an 88-year-old woman with 2:1 AV nodal block in the setting of digoxin therapy and potassium 2.8 mmol/L (2.8 mEq/L)From the collection of Sarah Stahmer, MD [Citation ends].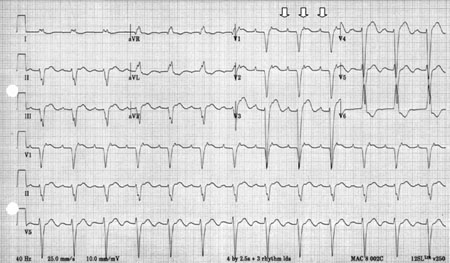 [Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in a 35-year-old with history of recent cocaine useFrom the collection of Sarah Stahmer, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in a 35-year-old with history of recent cocaine useFrom the collection of Sarah Stahmer, MD [Citation ends].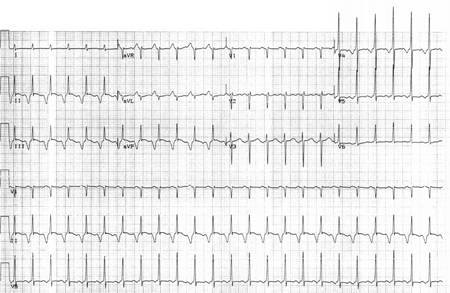 [Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in a 55-year-old with ischaemic cardiomyopathyFrom the collection of Sarah Stahmer, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in a 55-year-old with ischaemic cardiomyopathyFrom the collection of Sarah Stahmer, MD [Citation ends].
Pathophysiology
Atrial tachycardia is the least common and often the most challenging of the regular supraventricular tachycardias. It may arise from either atria or from structures contiguous with the atria, such as the pulmonary veins and superior vena cava. The anatomy of the atrium and surrounding structures serve as a substrate for arrhythmia initiation and propagation. Electrophysiological testing has shown that there are three possible mechanisms: abnormal automaticity of non-sinus atrial tissue, triggered automaticity due to delay after depolarisation, and micro-re-entry within the atria. Re-entrant circuits are dependent on areas of differential conduction and recovery and the presence of anatomic boundaries. Vulnerable atrial tissue due to scarring, disease, or medications can give rise to paroxysmal atrial tachycardias sustained by the bordering mitral and tricuspid annuli, orifices of the vena cava, pulmonary veins, and coronary sinus. Atrial tissues, such as the crista terminalis and pulmonary veins, are common sites for automaticity or triggered activity. The 12-lead ECG rarely provides clues to the cause. These are usually distinguished in the laboratory setting and rarely clinically.
In healthy people, the most likely cause is enhanced automaticity from a single focus in the atrium. It is usually seen in the setting of catecholamine excess, exacerbations of chronic lung disease, acute alcohol ingestion, and electrolyte imbalances. This rhythm tends to accelerate to its maximal rate and does not start with a premature atrial contraction. It typically shows beat-to-beat variability during warm-up and decelerates gradually. The contour of the P wave differs from the sinus P wave, with heart rates usually <200 bpm. Automatic atrial tachycardia tends to be incessant, particularly in children.
Re-entry is probably the underlying mechanism in people with diseased atrial tissue or those who have undergone cardiac surgery or ablation involving the atria. The arrhythmia circumnavigates the surgical scar, forming separate functional or anatomical limbs of the tachycardia. Slow conduction and unidirectional block induced by a premature beat completes the re-entrant circuit. A premature atrial beat starts the tachycardia loop, and alternations in the re-entrant circuit conduction can abruptly terminate the tachycardia, imparting it a paroxysmal nature.
Atrial tachycardias due to triggered activity are usually seen in patients with a known cardiomyopathy taking digoxin. These rhythms tend to be prolonged and are difficult to treat. They are also characterised by a warm-up period at onset and a cool-down period at termination rather than the abrupt nature of re-entrant loops. Atrial tachycardias due to digoxin toxicity typically involve AV block.
Classification
Atrial tachycardias[1]
Sinus tachycardia: regular tachycardia with uniform P wave before every QRS. Rate shows gradual variation in response to sympathetic/parasympathetic stimulation.
Focal atrial tachycardia: recurrent, regular tachycardia with a fixed heart rate at 100 to 250 bpm. P waves are visible before every QRS, and are uniform in their appearance when looking at a single lead. Onset and termination of arrhythmia are abrupt.
AV node re-entrant tachycardia: regular tachycardia with a fixed rate in the range of 140 to 280 bpm. P waves may be visible, but usually follow the QRS complex with a short R-P interval.
Multi-focal atrial tachycardia: irregular tachycardia at a rate of 120 to 200 bpm. P waves occur before every QRS, and there are at least three different P-wave morphologies when looking at a single lead.
Atrial flutter: new-onset atrial flutter usually has a fixed heart rate of 145 to 150 bpm due to 2:1 AV block and an atrial flutter rate of 300 bpm. When medicated with AV node-blocking agents, the heart rate may be irregular, indicating variable AV block.
Atrial fibrillation: irregular tachycardia with beat-to-beat variation in heart rate, P waves replaced by fibrillatory waves.
Use of this content is subject to our disclaimer