History and exam
Key diagnostic factors
common
presence of risk factors
Key risk factors include substance misuse, digoxin toxicity, and previous cardiac surgery to correct congenital heart defects.
cardiac disease
Previous myocardial infarction, cardiac or great vessel surgery, congenital heart disease, or cardiomyopathy predisposes to focal atrial tachycardia.
Other diagnostic factors
common
medications
Include aminophylline, beta-agonists, potassium-wasting diuretics, or over-the-counter cold/sinus medications that contain phenylephrine.
palpitations
The beating of the heart becomes clinically manifest when the rate is discordant with clinical context - for example, a heart rate of 160 bpm while lying in bed.
fatigue, weakness
Result from poor cardiac output and decreased exercise tolerance.
uncommon
chest pain
Chest pressure, pain, or dyspnoea suggests an acute coronary syndrome, which may be a precipitating event or a result of the tachyarrhythmia.
shortness of breath, cough
Indicate worsening of baseline COPD or congestive heart failure, which may precipitate the arrhythmia.
Other symptoms include fever, sputum, wheezing, nocturnal cough, orthopnoea, and paroxysmal nocturnal dyspnoea.
nausea, vomiting
Symptoms of digoxin toxicity.
light-headedness, syncope
Indicate haemodynamic compromise from the tachyarrhythmia.
rales
Indicate congestive heart failure.
oedema
Indicates congestive heart failure.
Risk factors
strong
substance misuse (alcohol ingestion/withdrawal, cocaine, amphetamines)
These are associated with catecholamine excess.[6] The proposed mechanism is enhanced automaticity of non-pacemaker cells.[Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in a 35-year-old with history of recent cocaine useFrom the collection of Sarah Stahmer, MD [Citation ends].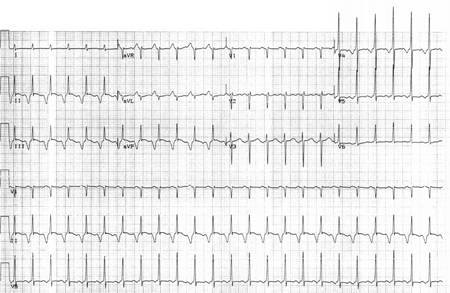
digoxin toxicity
The risk is increased in the setting of kidney disease, hypokalaemia, hypomagnesemia and drug interactions that may increase digoxin concentrations (e.g., amiodarone, verapamil, quinidine).[6]
Focal AT with AV nodal block is a classic presenting dysrhythmia in digoxin intoxication.[Figure caption and citation for the preceding image starts]: Focal atrial tachycardia in an 88-year-old woman with 2:1 AV nodal block in the setting of digoxin therapy and potassium 2.8 mmol/L (2.8 mEq/L)From the collection of Sarah Stahmer, MD [Citation ends].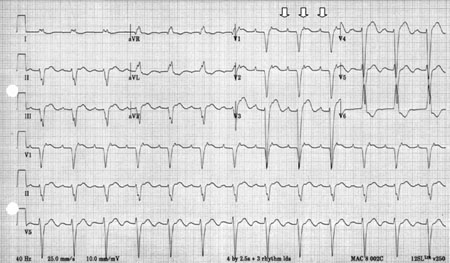
previous cardiac surgery to correct congenital heart defects
Congenital defects include transposition of the great vessels and atrial septal defects.[7]
Cardiac surgery leaves scar tissue in the atrial tissue, which provides a substrate for micro re-entry pathways.
weak
coronary artery disease
Given the rarity of focal atrial tachycardia (focal AT), its multiple mechanisms, and disease associations, much of the data linking this arrhythmia to a cause are observational.
exacerbation of chronic lung disease
A variety of supraventricular tachyarrhythmias have been associated with acute respiratory illnesses, the most common being multi-focal atrial tachycardia.
Focal AT is less common, but the underlying mechanisms of enhanced automaticity are the same: hypoxia, administration of medications such as methylxanthines and beta agonists, and electrolyte disturbances.
theophylline
Theophylline increases atrial automaticity, which can predispose to supraventricular tachycardia, including atrial tachycardia.[6]
Use of this content is subject to our disclaimer