Complications
Infants with MAS are prone to develop air leak syndromes.[3] Partial obstructions and airway trapping may lead to alveolar overdistention (ball-valve mechanism). Also, mechanical ventilation using high peak inspiratory pressure causes air leaking. Once the alveoli rupture, the air enters the mediastinum, causing pneumothorax. The accumulation of air in these spaces can compromise ventilation and cardiac function. Unrecognised and untreated, pneumothorax leads to persistence of hypoxia and continuation of persistent pulmonary hypertension.
Air leak syndromes should be recognised early and treated appropriately to avoid compromise of ventilation and oxygenation. Treatment consists of removal of the accumulated air using needle aspiration and/or continuous drainage of air using an underwater drainage system.[Figure caption and citation for the preceding image starts]: CXR showing air at the base of right lung above the diaphragm, suggestive of pneumothorax in a patient with MASFrom the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].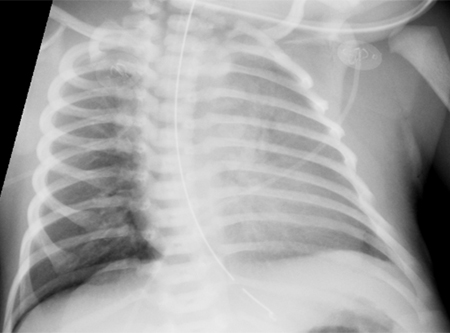
Infants with MAS are at risk of developing persistent pulmonary hypertension. Inhaled nitric oxide and extracorporeal membrane oxygenation therapy may be required in these patients.
Infants with MAS are prone to develop air leak syndromes.[3] Partial obstructions and airway trapping may lead to alveolar overdistention (ball-valve mechanism). Also, mechanical ventilation using high peak inspiratory pressure causes air leaking. Once the alveoli rupture, the air enters the mediastinum, causing pneumomediastinum.
The accumulation of air in these spaces can compromise ventilation and cardiac function. Unrecognised and untreated, it leads to persistence of hypoxia and continuation of persistent pulmonary hypertension.
Air leak syndromes should be recognised early and treated appropriately to avoid compromise of ventilation and oxygenation. Treatment consists of removal of the accumulated air using needle aspiration and/or continuous drainage of air using an underwater drainage system.[Figure caption and citation for the preceding image starts]: Pneumomediastinum with spinnaker sail sign (arrow)From the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].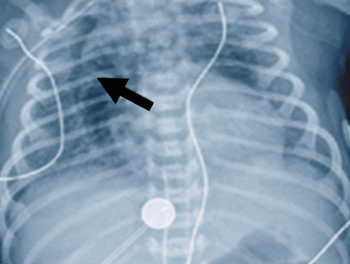
Infants who require high ventilatory pressure and prolonged oxygen exposure may develop chronic lung disease secondary to barotrauma and oxygen toxicity. Between 5% and 10% of ventilated infants require oxygen beyond 28 days after birth. The risk of this complication can be reduced by using appropriate ventilation, lowering oxygen requirements. Use of surfactant therapy, high-frequency ventilation, extracorporeal membrane oxygenation, and inhaled nitric oxide may help decrease the need for high pressures and high oxygen concentrations.[3]
Neurological complications in MAS are secondary to cerebral hypoxaemic ischaemia of the brain and include cerebral palsy.[3][70][72]
This depends on the severity of fetal distress before delivery and on the degree of hypoxaemia experienced after birth.
Some may present with concomitant physical disabilities requiring physiotherapy.
Neurological complications in MAS are secondary to cerebral hypoxaemic ischaemia of the brain and include seizures.[3][70]
This depends on the severity of fetal distress before delivery and on the degree of hypoxaemia experienced after birth. About 5% of infants with MAS admitted to the neonatal intensive care unit have neurological symptoms of hypotonia and seizure.[9]
Supportive therapy with anticonvulsants and emergent treatment with brain cooling may have beneficial effects in these infants.
MAS is associated with invasive procedures such as multiple intubations and intravascular lines such as umbilical, arterial, and venous, which increase the risk of infection. Infections may also be acquired during delivery.
Risk can be reduced by using sterile techniques.[3]
Use of this content is subject to our disclaimer