Investigations
1st investigations to order
CXR
Test
Infants with respiratory distress must have CXR in both anteroposterior and lateral positions. Pneumothorax or pneumomediastinum is differentiated in lateral views of chest.
In pneumomediastinum, a 'spinnaker sail' sign (lifting of thymic lobes) in the posteroanterior view is a typical finding.[50]
Asymmetric chest wall and asymmetric movements with decreased air entry suggest pneumothorax.
Cardiomegaly with increased cardiothoracic ratio may be seen in the presence of severe intrauterine hypoxia.[Figure caption and citation for the preceding image starts]: CXR showing patchy infiltrations on both lungs, suggestive of atelectasis in a patient with MASFrom the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].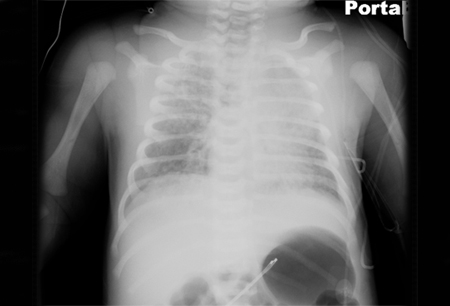 [Figure caption and citation for the preceding image starts]: Pneumomediastinum with spinnaker sail sign (arrow)From the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].
[Figure caption and citation for the preceding image starts]: Pneumomediastinum with spinnaker sail sign (arrow)From the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].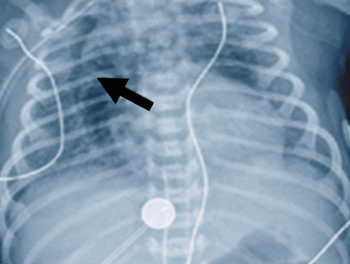 [Figure caption and citation for the preceding image starts]: CXR showing air at the base of right lung above the diaphragm, suggestive of pneumothorax in a patient with MASFrom the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].
[Figure caption and citation for the preceding image starts]: CXR showing air at the base of right lung above the diaphragm, suggestive of pneumothorax in a patient with MASFrom the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].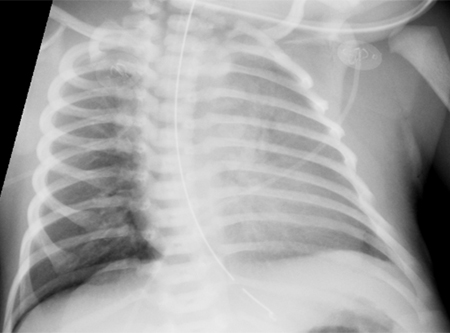
Result
pulmonary hyperinflation with patchy infiltrates alternating with areas of atelectasis; radiological findings may be variable
FBC
Test
Performed to rule out infection.
Result
low WBC count if infection is present
CRP
Test
Performed to rule out infection.
Result
may be elevated if infection is present
blood culture
Test
Performed to rule out infection.
Result
may be positive for infectious organism if infection is present
Investigations to consider
dual pulse oximetry
Test
Patients with severe respiratory distress should be assessed with dual pulse oximetry. Oxygen saturations with a difference of ≥10% between the right upper limb and lower limb suggests right-to-left shunt from pulmonary artery to descending aorta through the ductus arteriosus. This indicates presence of pulmonary hypertension.[49][52]
Result
abnormal pre- and postductal values (≥10%)
ABG (pH, PaO₂, PaCO₂)
Test
Preferably arterial samples from umbilical artery if an umbilical arterial catheter is in place. Otherwise, a radial arterial sample can be obtained. A warmed heel arterialised capillary sample is acceptable for measuring arterial oxygen.
This test in full-term infants may help distinguish pulmonary disease from congenital heart disease. Administration of 100% oxygen leads to an increase in PaO₂ in the presence of pulmonary disease, but not in the presence of cyanotic congenital heart disease. This test is not performed in preterm neonates: oxygen administration should be carefully titrated to minimise the risk of retinopathy of prematurity.
Result
may show hypoxaemia, hypercarbia, acidosis
echocardiography
Test
May be performed to rule out congenital cyanotic heart disease and to assess pulmonary vascular resistance.
Result
may be normal; may show signs of pulmonary hypertension, including tricuspid regurgitation, elevated pulmonary artery pressure, and right-to-left shunt through patent ductus arteriosus and patent foramen ovale
cranial ultrasound
Test
Performed if neurological damage is suspected (hypotonia, seizures).
Result
may show hypoxaemic brain injury, hypodensity, cerebral oedema, intracranial haemorrhage
electroencephalogram
Test
Performed if neurological damage is suspected (hypotonia, seizures).
Result
may show seizure activity, decreased amplitude (diffuse oedema or diffuse injury)
urinalysis
Test
Patients with severe hypoxia may present with oliguria or anuria.
Result
may show haematuria, proteinuria
Use of this content is subject to our disclaimer