History and exam
Key diagnostic factors
common
presence of risk factors
Key risk factors include: gestational age >42 weeks; maternal history of hypertension, pre-eclampsia, eclampsia, smoking, substance abuse; fetal distress; oligohydramnios; thick meconium; an Apgar score <7; chorioamnionitis and caesarean delivery.
signs of post-maturity
Typical signs include green/yellow-coloured skin and umbilical cord; long, stained nails; dry and peeling skin; post-mature appearance; and loss of subcutaneous tissue.
tachypnoea
Usually seen immediately after birth. However, a significant number of infants may be asymptomatic and apparently vigorous at birth and develop severe respiratory distress hours later.
cyanosis
Usually seen immediately after birth. However, a significant number of infants may be asymptomatic and apparently vigorous at birth and develop severe respiratory distress hours later. The presence of cyanosis should prompt immediate intervention.
chest wall asymmetry with decreased air entry
An asymmetric chest wall and asymmetric movements with decreased air entry suggest pneumothorax.[Figure caption and citation for the preceding image starts]: CXR showing air at the base of right lung above the diaphragm, suggestive of pneumothorax in a patient with MASFrom the personal collection of Dr Vidyasagar and Dr Bhat [Citation ends].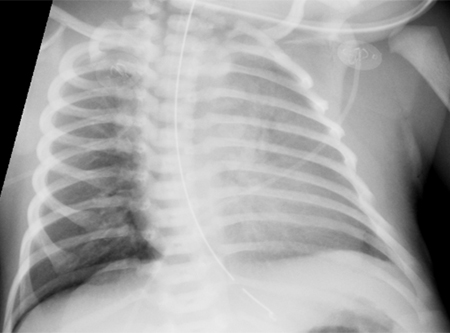
barrel-shaped chest
Seen as increased anteroposterior chest diameter.
Other diagnostic factors
common
grunting
Due to reduced pulmonary compliance.
chest retractions
Due to reduced pulmonary compliance.
rales
Breath sounds may be diminished. Diffuse rales may be present.
rhonchi
Breath sounds may be diminished. Rhonchi may be present.
tachycardia
May be present due to respiratory distress.
hypotension
May be present due to respiratory distress.
Risk factors
strong
gestational age >42 weeks
Meconium-stained amniotic fluid is seen in 22% to 44% of post-mature babies (>42 weeks' gestation).[3] Post-maturity is associated with increasing placental insufficiency, which causes fetal hypoxia and passage of meconium. The reported decreased incidence of MAS during the 1990s may be due to a 33% reduction in post-term births.[8]
pregnancy-induced hypertension
Pregnancy-induced hypertension is associated with a 1.7-fold increased risk of MAS.[26]
maternal diabetes mellitus
Maternal diabetes mellitus is associated with a 3-fold increased risk of MAS.[26]
maternal smoking or substance misuse
Maternal tobacco smoking and substance misuse (especially cocaine) are associated with fetal distress and an increased risk of meconium-stained amniotic fluid and MAS.[6] They can cause placental vasoconstriction, which leads to fetal hypoxia and induces fetal passage of meconium.
fetal distress
Meconium passage is a marker of intrapartum and antepartum fetal compromise. Non-reassuring or abnormal cardiotocography is associated with MAS.[27]
oligohydramnios
Causes cord compression and fetal hypoxaemia. Oligohydramnios is associated with a 2.8-fold increase in risk of MAS.[28]
thick meconium
Clinical presentation of infants born in meconium-stained amniotic fluid can depend on the consistency of the meconium. When infants are born through thin meconium and are vigorous at birth, respiratory complications are minimal.[29]
Apgar score <7
chorioamnionitis
Causes fetal stress and passage of meconium in utero. Intrapartum maternal fever is associated with diagnosis of MAS.[27]
caesarean delivery
Babies born by caesarean section have a greater risk of MAS.[27]
Use of this content is subject to our disclaimer