Patients with established atrial fibrillation (AF) may present with typical symptoms (e.g., palpitations, shortness of breath, fatigue, chest pain, dizziness), complications of AF (e.g., stroke), or associated conditions (e.g., features of thyroid disease), or they may be asymptomatic. An ECG usually confirms the diagnosis. Further investigations include baseline laboratory blood tests and echocardiogram.
Clinical presentation
The most common presenting symptoms of AF are palpitations, shortness of breath, and fatigue; chest pain, dizziness, and anxiety occur less frequently.[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
[80]National Institute for Health and Care Excellence. Atrial fibrillation: diagnosis and management. Jun 2021 [internet publication].
https://www.nice.org.uk/guidance/ng196
[81]Jurgens CY, Lee CS, Aycock DM, et al. State of the science: the relevance of symptoms in cardiovascular disease and research: a scientific statement from the American Heart Association. Circulation. 2022 Sep 20;146(12):e173-84.
https://www.doi.org/10.1161/CIR.0000000000001089
http://www.ncbi.nlm.nih.gov/pubmed/35979825?tool=bestpractice.com
AF may also present with symptoms associated with stroke.[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
[80]National Institute for Health and Care Excellence. Atrial fibrillation: diagnosis and management. Jun 2021 [internet publication].
https://www.nice.org.uk/guidance/ng196
Women and younger patients usually present with palpitations, whereas men are more likely to be asymptomatic.[81]Jurgens CY, Lee CS, Aycock DM, et al. State of the science: the relevance of symptoms in cardiovascular disease and research: a scientific statement from the American Heart Association. Circulation. 2022 Sep 20;146(12):e173-84.
https://www.doi.org/10.1161/CIR.0000000000001089
http://www.ncbi.nlm.nih.gov/pubmed/35979825?tool=bestpractice.com
Black patients report more AF symptoms compared with white or Hispanic patients.[81]Jurgens CY, Lee CS, Aycock DM, et al. State of the science: the relevance of symptoms in cardiovascular disease and research: a scientific statement from the American Heart Association. Circulation. 2022 Sep 20;146(12):e173-84.
https://www.doi.org/10.1161/CIR.0000000000001089
http://www.ncbi.nlm.nih.gov/pubmed/35979825?tool=bestpractice.com
AF can cause a tachycardia-induced cardiomyopathy resulting in symptoms of congestive heart failure.[3]Lévy S, Steinbeck G, Santini L, et al. Management of atrial fibrillation: two decades of progress - a scientific statement from the European Cardiac Arrhythmia Society. J Interv Card Electrophysiol. 2022 Oct;65(1):287-326.
http://www.ncbi.nlm.nih.gov/pubmed/35419669?tool=bestpractice.com
In some cases, due to the rapidity of the ventricular response, cerebral hypoperfusion can result in presyncope or syncope.
In asymptomatic patients, AF may be incidentally detected during a health check or following an acute complication, such as stroke. The prevalence of AF in patients with a first-ever ischaemic stroke has been found to be around 15% to 25%.[4]Marini C, De Santis F, Sacco S, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005 Jun;36(6):1115-9.
https://www.ahajournals.org/doi/full/10.1161/01.STR.0000166053.83476.4a
http://www.ncbi.nlm.nih.gov/pubmed/15879330?tool=bestpractice.com
[5]Paciaroni M, Agnelli G, Caso V, et al. Atrial fibrillation in patients with first-ever stroke: frequency, antithrombotic treatment before the event and effect on clinical outcome. J Thromb Haemost. 2005 Jun;3(6):1218-23.
http://onlinelibrary.wiley.com/doi/10.1111/j.1538-7836.2005.01344.x/full
http://www.ncbi.nlm.nih.gov/pubmed/15892862?tool=bestpractice.com
The past medical and surgical history may be significant for all types of cardiac disease (such as valvular heart disease, coronary artery disease, hypertension, pericarditis, cardiomyopathy, and other arrhythmias), including recent cardiothoracic surgery, as well as for many non-cardiac conditions such as diabetes, thyroid disease, and cancer. Risk factors for sleep-disordered breathing (SDB) should be considered, with screening and diagnosis where indicated. Although polysomnography is the gold standard for diagnosing SDB, home sleep apnoea testing shows promise in diagnosing obstructive sleep apnoea in most patients with AF.[45]Mehra R, Chung MK, Olshansky B, et al. Sleep-disordered breathing and cardiac arrhythmias in adults: mechanistic insights and clinical implications: a scientific statement from the American Heart Association. Circulation. 2022 Aug 30;146(9):e119-36.
https://www.doi.org/10.1161/CIR.0000000000001082
http://www.ncbi.nlm.nih.gov/pubmed/35912643?tool=bestpractice.com
The modified European Heart Rhythm Association symptom scale can be used to assess and quantify symptoms before and after initiation of treatment. It evaluates the effect of six symptoms of AF (palpitations, fatigue, dizziness, dyspnoea, chest pain, and anxiety) on the patient’s daily activity.[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
Class 1: AF does not cause any symptoms
Class 2a (mild): normal daily activity not affected by symptoms related to AF
Class 2b (moderate): normal daily activity not affected by symptoms related to AF, but patient troubled by symptoms
Class 3 (severe): normal daily activity affected by symptoms related to AF
Class 4 (disabling): normal daily activity discontinued.
AF symptoms do not always correlate with objectively measured AF episodes and AF can switch between symptomatic and asymptomatic even in the same individual.[81]Jurgens CY, Lee CS, Aycock DM, et al. State of the science: the relevance of symptoms in cardiovascular disease and research: a scientific statement from the American Heart Association. Circulation. 2022 Sep 20;146(12):e173-84.
https://www.doi.org/10.1161/CIR.0000000000001089
http://www.ncbi.nlm.nih.gov/pubmed/35979825?tool=bestpractice.com
Multiple studies have shown a clear association between AF and increased risk of cognitive impairment and dementia.[81]Jurgens CY, Lee CS, Aycock DM, et al. State of the science: the relevance of symptoms in cardiovascular disease and research: a scientific statement from the American Heart Association. Circulation. 2022 Sep 20;146(12):e173-84.
https://www.doi.org/10.1161/CIR.0000000000001089
http://www.ncbi.nlm.nih.gov/pubmed/35979825?tool=bestpractice.com
[82]Chen LY, Norby FL, Gottesman RF, et al. Association of atrial fibrillation with cognitive decline and dementia over 20 Years: the ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study). J Am Heart Assoc. 2018 Mar 7;7(6):e007301.
https://www.doi.org/10.1161/JAHA.117.007301
http://www.ncbi.nlm.nih.gov/pubmed/29514809?tool=bestpractice.com
[83]Papanastasiou CA, Theochari CA, Zareifopoulos N, et al. Atrial fibrillation is associated with cognitive impairment, all-cause dementia, vascular dementia, and alzheimer's disease: a systematic review and meta-analysis. J Gen Intern Med. 2021 Oct;36(10):3122-35.
https://link.springer.com/article/10.1007/s11606-021-06954-8
http://www.ncbi.nlm.nih.gov/pubmed/34244959?tool=bestpractice.com
[84]Koh YH, Lew LZW, Franke KB, et al. Predictive role of atrial fibrillation in cognitive decline: a systematic review and meta-analysis of 2.8 million individuals. Europace. 2022 Sep 1;24(8):1229-39.
https://academic.oup.com/europace/article/24/8/1229/6513640?login=false
http://www.ncbi.nlm.nih.gov/pubmed/35061884?tool=bestpractice.com
[85]Zhang W, Liang J, Li C, et al. Age at diagnosis of atrial fibrillation and incident dementia.. JAMA Netw Open. 2023 Nov 1;6(11):e2342744.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2811523
http://www.ncbi.nlm.nih.gov/pubmed/37938842?tool=bestpractice.com
This association is independent of whether patients had prior stroke or not, and whether the dementia is due to Alzheimer's disease or vasculopathies.[81]Jurgens CY, Lee CS, Aycock DM, et al. State of the science: the relevance of symptoms in cardiovascular disease and research: a scientific statement from the American Heart Association. Circulation. 2022 Sep 20;146(12):e173-84.
https://www.doi.org/10.1161/CIR.0000000000001089
http://www.ncbi.nlm.nih.gov/pubmed/35979825?tool=bestpractice.com
[83]Papanastasiou CA, Theochari CA, Zareifopoulos N, et al. Atrial fibrillation is associated with cognitive impairment, all-cause dementia, vascular dementia, and alzheimer's disease: a systematic review and meta-analysis. J Gen Intern Med. 2021 Oct;36(10):3122-35.
https://link.springer.com/article/10.1007/s11606-021-06954-8
http://www.ncbi.nlm.nih.gov/pubmed/34244959?tool=bestpractice.com
[86]Diener HC, Hart RG, Koudstaal PJ, et al. Atrial fibrillation and cognitive function: JACC review topic of the week. J Am Coll Cardiol. 2019 Feb 12;73(5):612-19.
https://www.doi.org/10.1016/j.jacc.2018.10.077
http://www.ncbi.nlm.nih.gov/pubmed/30732716?tool=bestpractice.com
The pathophysiology and exact mechanisms (e.g., silent microinfarcts, cerebral hypoperfusion and bleed, ischaemic stroke) of AF-related dementia require further evaluation.
Physical examination
The pulse may be irregularly irregular and rapid but, depending on where the pulse is taken, decreased perfusion may cause an underestimation of these findings.[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
[80]National Institute for Health and Care Excellence. Atrial fibrillation: diagnosis and management. Jun 2021 [internet publication].
https://www.nice.org.uk/guidance/ng196
Palpation of the carotids or auscultation may be necessary. An apparently palpable regular pulse does not exclude AF. It can be extremely difficult to appreciate irregularity if the pulse rate is very rapid or very slow. The latter may occur in patients with very poor atrioventricular (AV) nodal conduction due to intrinsic AV nodal disease or AV nodal blocking drugs. In patients with digitalis toxicity, a junctional rhythm may be present in the face of AF. An apparently irregular pulse does not always indicate AF: for example, other causes of irregular pulse are frequent premature atrial and/or ventricular complexes in the presence of sinus rhythm, atrial tachycardia, or atrial flutter. It is therefore necessary to confirm the rhythm with an ECG. Other findings may include irregular jugular venous pulsations, variation in the intensity of the first heart sound, or absence of a fourth sound heard previously during sinus rhythm.
There may be physical findings consistent with an underlying cause of AF, such as features of heart failure, stroke, or an endocrinological problem, such as hyperthyroidism. In an older patient the symptoms may be as subtle as a decrease in mentation or listlessness.
ECG
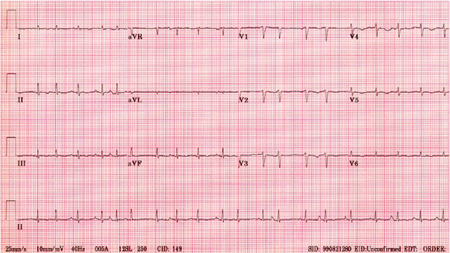
An ECG is performed in all patients with possible AF, and is usually confirmatory. P waves are absent and are replaced by rapid fibrillatory waves, which vary in size, shape, and timing, leading to an irregular ventricular response when AV conduction is intact. [Figure caption and citation for the preceding image starts]: Atrial fibrillation: P waves are not discernible; the ventricular (QRS complexes) rate is irregularly irregularFrom the collection of Dr Arti N. Shah [Citation ends].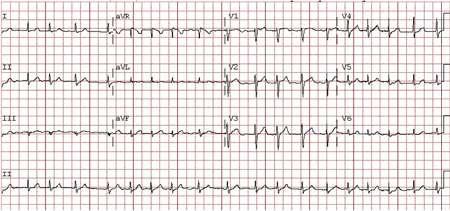 [Figure caption and citation for the preceding image starts]: Atrial fibrillation: P waves are not discernible; 'fibrillatory or f waves' of varying amplitudes and very rapid and irregular rates are particularly seen in lead V1; the ventricular (QRS complexes) rate is irregularly irregularFrom the collection of Dr Bharat K. Kantharia [Citation ends].
[Figure caption and citation for the preceding image starts]: Atrial fibrillation: P waves are not discernible; 'fibrillatory or f waves' of varying amplitudes and very rapid and irregular rates are particularly seen in lead V1; the ventricular (QRS complexes) rate is irregularly irregularFrom the collection of Dr Bharat K. Kantharia [Citation ends].
Low-amplitude P waves, such as in an atrial tachycardia, especially multifocal atrial tachycardia that may be observed in patients with COPD, may mimic AF. In patients with cardiac implantable electronic devices (CIEDs) such as the permanent pacemakers, AF may be detected as atrial high rate episodes (AHRE). Like clinical AF, CIED-recorded AHRE need to be confirmed by inspection of stored electrogram events because some AHRE may be electrical artefacts/false positives.[1]Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024 Jan 2;149(1):e1-156.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001193?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/38033089?tool=bestpractice.com
In patients with CIEDs, if surface ECG shows rapid-paced ventricular rate, underlying AF may not be visible between the paced ventricular complexes and the diagnosis of AF may be missed. Inconsistent premature atrial contractions can impart an irregular ventricular rhythm that at times may be called AF by the ECG diagnostic algorithms.
ECG can also be used to screen for a pre-excitation syndrome, such as Wolff-Parkinson-White syndrome. See Wolff-Parkinson-White syndrome.
Other rhythms that need to be excluded are counterclockwise atrial flutter, clockwise atrial flutter, and multifocal atrial tachycardia. Where diagnostic uncertainty remains, the use of Holter monitoring or an event recorder (e.g., Cardiomemo) may also be required.[1]Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024 Jan 2;149(1):e1-156.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001193?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/38033089?tool=bestpractice.com
[80]National Institute for Health and Care Excellence. Atrial fibrillation: diagnosis and management. Jun 2021 [internet publication].
https://www.nice.org.uk/guidance/ng196
[Figure caption and citation for the preceding image starts]: Atrial flutter: typical saw-tooth appearance of the flutter waves in the inferior leads (leads II, III, and aVF) indicates typical counterclockwise atrial flutter; the ventricular (QRS complexes) rate is variableFrom the collection of Dr Arti N. Shah [Citation ends]. [Figure caption and citation for the preceding image starts]: Multifocal atrial tachycardia: there are P waves of multiple (at least 3) different morphologiesFrom the collection of Dr Arti N. Shah [Citation ends].
[Figure caption and citation for the preceding image starts]: Multifocal atrial tachycardia: there are P waves of multiple (at least 3) different morphologiesFrom the collection of Dr Arti N. Shah [Citation ends].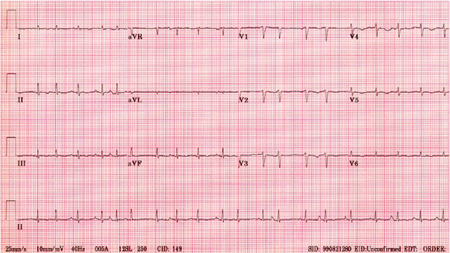
Mobile health technologies, including smart devices, have become a popular research area for AF detection.[87]Lopez Perales CR, Van Spall HGC, Maeda S, et al. Mobile health applications for the detection of atrial fibrillation: a systematic review. Europace. 2021 Jan 27;23(1):11-28.
https://www.doi.org/10.1093/europace/euaa139
http://www.ncbi.nlm.nih.gov/pubmed/33043358?tool=bestpractice.com
[88]Guo Y, Wang H, Zhang H, et al. Mobile Photoplethysmographic Technology to Detect Atrial Fibrillation. J Am Coll Cardiol. 2019 Nov 12;74(19):2365-2375.
https://www.doi.org/10.1016/j.jacc.2019.08.019
http://www.ncbi.nlm.nih.gov/pubmed/31487545?tool=bestpractice.com
[89]Nazarian S, Lam K, Darzi A, et al. Diagnostic accuracy of smartwatches for the detection of cardiac arrhythmia: systematic review and meta-analysis. J Med Internet Res. 2021 Aug 27;23(8):e28974.
https://www.jmir.org/2021/8/e28974
http://www.ncbi.nlm.nih.gov/pubmed/34448706?tool=bestpractice.com
[90]Gill S, Bunting KV, Sartini C, et al. Smartphone detection of atrial fibrillation using photoplethysmography: a systematic review and meta-analysis. Heart. 2022 Sep 26;108(20):1600-7.
https://heart.bmj.com/content/108/20/1600.long
http://www.ncbi.nlm.nih.gov/pubmed/35277454?tool=bestpractice.com
[91]Sattar Y, Song D, Sarvepalli D, et al. Accuracy of pulsatile photoplethysmography applications or handheld devices vs. 12-lead ECG for atrial fibrillation screening: a systematic review and meta-analysis. J Interv Card Electrophysiol. 2022 Oct;65(1):33-44.
https://link.springer.com/article/10.1007/s10840-021-01068-x
http://www.ncbi.nlm.nih.gov/pubmed/34775555?tool=bestpractice.com
[92]Biersteker TE, Schalij MJ, Treskes RW. Impact of mobile health devices for the detection of atrial fibrillation: systematic review. JMIR Mhealth Uhealth. 2021 Apr 28;9(4):e26161.
https://mhealth.jmir.org/2021/4/e26161
http://www.ncbi.nlm.nih.gov/pubmed/33908885?tool=bestpractice.com
A large number of mobile health apps and wearable activity monitors are available, but many are not clinically validated and caution is advised for clinical use.[1]Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024 Jan 2;149(1):e1-156.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001193?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/38033089?tool=bestpractice.com
[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
If AF is detected by mobile or wearable devices, diagnosis should be confirmed with single-lead or 12-lead ECG analysed by a physician with expertise in ECG rhythm interpretation.[1]Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024 Jan 2;149(1):e1-156.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001193?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/38033089?tool=bestpractice.com
[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
Echocardiography
Transthoracic echocardiogram may be performed after the 12-lead ECG and is important to exclude important cardiac pathologies and risk factors for persistent AF, such as valvular and pericardial disease and cardiomyopathies.[1]Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024 Jan 2;149(1):e1-156.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001193?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/38033089?tool=bestpractice.com
[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
Furthermore, it can suggest left atrial thrombus. However, absence of thrombi in the left atrium by a transthoracic echocardiogram does not rule them out. In order to exclude left atrial thrombi, it is mandatory to perform a trans-oesophageal echocardiogram as opposed to a transthoracic echocardiogram, because this test is more accurate at detecting left atrial thrombi. All patients who need cardioversion, and have unknown or suboptimal anticoagulation profile, should have a trans-oesophageal echocardiogram first to exclude left atrial thrombus.
Laboratory evaluation
Thyroid function tests should be done in all patients presenting with AF. Hyperthyroidism can be diagnosed with laboratory work and treated appropriately with medicine, radioablative therapy, or surgery. Diagnosing thyrotoxicosis is also important when the ventricular rate is difficult to control.[1]Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024 Jan 2;149(1):e1-156.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001193?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/38033089?tool=bestpractice.com
[2]Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498.
https://academic.oup.com/eurheartj/article/42/5/373/5899003
http://www.ncbi.nlm.nih.gov/pubmed/32860505?tool=bestpractice.com
Furthermore, cardiomyopathy related to thyrotoxicosis may reverse completely upon treatment of thyrotoxicosis. Routine biochemistry including serum urea and electrolytes plus serum magnesium, and liver transaminases, should be done to assess for the presence of other comorbid conditions, and to assess electrolyte and metabolic status. These tests are also helpful in choosing anti-arrhythmic agents and their dosages. Screening for diabetes mellitus should also be considered.
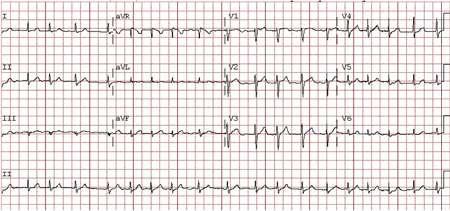 [Figure caption and citation for the preceding image starts]: Atrial fibrillation: P waves are not discernible; 'fibrillatory or f waves' of varying amplitudes and very rapid and irregular rates are particularly seen in lead V1; the ventricular (QRS complexes) rate is irregularly irregularFrom the collection of Dr Bharat K. Kantharia [Citation ends].
[Figure caption and citation for the preceding image starts]: Atrial fibrillation: P waves are not discernible; 'fibrillatory or f waves' of varying amplitudes and very rapid and irregular rates are particularly seen in lead V1; the ventricular (QRS complexes) rate is irregularly irregularFrom the collection of Dr Bharat K. Kantharia [Citation ends].
 [Figure caption and citation for the preceding image starts]: Multifocal atrial tachycardia: there are P waves of multiple (at least 3) different morphologiesFrom the collection of Dr Arti N. Shah [Citation ends].
[Figure caption and citation for the preceding image starts]: Multifocal atrial tachycardia: there are P waves of multiple (at least 3) different morphologiesFrom the collection of Dr Arti N. Shah [Citation ends].