Approach
It is unusual to have Wolff-Parkinson-White (WPW) pattern as an incidental finding in healthy people who have ECG recording done for a routine health check-up. When managing patients with a WPW pattern on an ECG, the clinician should consider two main points: first, assessment of symptoms that may be due to the accessory pathway (AP) (e.g., palpitations, periods of fast heart rates, syncope or near-syncope); second, assessing the risk of sudden cardiac death.
Acute presentations
Patients with an acute arrhythmia due to WPW may present with palpitations, dizziness, shortness of breath, chest pain, and/or sudden cardiac death. The most common arrhythmias diagnosed are atrioventricular re-entrant tachycardia, atrial fibrillation, and atrial flutter. Sudden cardiac death and syncope are associated outcomes but rare. ECG should be recorded in any patients with suspected supraventricular arrhythmia.
Congenital cardiac abnormalities
From 7% to 20% of patients with WPW syndrome have other accompanying congenital abnormalities, the most common being Ebstein's anomaly, which is associated with single or multiple right-sided APs. Other rare associations include hypertrophic cardiomyopathy, mitral valve prolapse, atrial septal defect, ventricular septal defect, transposition of the great vessels, coarctation of the aorta, dextrocardia, coronary sinus diverticula, right and left atrial aneurysms, cardiac rhabdomyomas (as seen in patients with tuberous sclerosis), Marfan's syndrome, and Friedreich's ataxia. Echocardiogram can be used to diagnose these.[Figure caption and citation for the preceding image starts]: Right lateral accessory pathway in a patient with Ebstein's anomalyFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: WPW syndrome in a patient with hypertrophic obstructive cardiomyopathyFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: WPW syndrome in a patient with hypertrophic obstructive cardiomyopathyFrom the collection of Dr Mithilesh K. Das [Citation ends].
Locating APs
The precise localisation of APs helps in assessing the success rate and risks for catheter ablation, and in planning the ablation strategy. For example, left-sided APs are often ablated via a transseptal approach, and paraseptal APs, which are close to the His bundle, are associated with a risk for complete atrioventricular block during catheter ablation (some electrophysiologists now prefer cryoablation for APs close to the His bundle; see the treatment section).
Several algorithms have been developed, but, as a general rule, a positive delta wave (first 40 ms of QRS complex) in lead V1 suggests a left-sided AP and a negative delta wave in V1 suggests a right-sided AP. A positive delta wave in the inferior leads suggests an anterior AP. A left axis (with a negative delta wave in lead V1) suggests a right lateral AP. If the delta waves in the inferior leads are negative, then it denotes an inferior AP. A negative delta wave in lead I, aVL, and V6 (rightward QRS axis) with a positive delta wave in lead V1 suggests a left lateral pathway. It is prudent to recognise that the delta wave vector can only be determined with precision when the ECG shows maximum pre-excitation.[Figure caption and citation for the preceding image starts]: Antidromic reciprocating tachycardia in a patient with right posteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: A simplified algorithm for localising an accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: A simplified algorithm for localising an accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].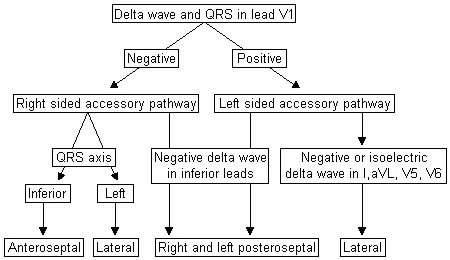 [Figure caption and citation for the preceding image starts]: Right anteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Right anteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: Left posteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Left posteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
Risk stratification
Patients with WPW pattern should be risk stratified with non-invasive and invasive tests, and those who are low risk should be monitored for any future arrhythmia. It is recommended that invasive risk stratification should be considered for all patients with asymptomatic pre-excitation and is strongly advised in all patients with asymptomatic pre-excitation who are competitive athletes or who have a high risk occupation. If a high risk AP is observed at the time of electrophysiology study (EPS), then catheter ablation is advised.[3] Therefore, asymptomatic patients should be referred to an electrophysiologist or a cardiologist with expertise in arrhythmia evaluation for risk stratification. While controversy exists, most experts recommend that all patients with ventricular pre-excitation undergo risk stratification to determine their risk of sudden cardiac death, regardless of the presence of symptoms.[15][16]
The risk of sudden cardiac death is determined by the anterograde refractory period of the AP. The presence of multiple APs and inducible tachycardia have also been identified as risk markers.
If the refractory period is very short, there are multiple APs, or tachycardia is induced, patients are at risk for developing symptomatic arrhythmias and also ventricular fibrillation in the setting of atrial fibrillation conducting rapidly over the AP. Shorter anterograde refractory periods are associated with an increased risk for sudden cardiac death because the AP can conduct impulses more rapidly to the ventricles. This is particularly important if the patient develops atrial fibrillation. Normally, the ventricles are 'protected' from rapid depolarisation due to the decremental properties of the AV node. However, in patients with an AP with a short anterograde refractory period, rapid conduction over the AP can lead to rapid ventricular rates that can deteriorate to ventricular fibrillation.
If ventricular pre-excitation is intermittent at rest, this suggests the anterograde refractory period is relatively long, and the AP is low risk for causing sudden cardiac death.
If ventricular pre-excitation is always present at rest, patients should be referred to an electrophysiologist to determine whether invasive risk stratification is warranted. If patients do not want to undergo an electrophysiology study, exercise stress testing can be used as a risk stratification tool.
Abrupt loss of pre-excitation during exercise is indicative of an AP incapable of dangerously rapid conduction from the atrium to the ventricle, and is considered to be a marker of a lower-risk AP. If pre-excitation does not abruptly disappear with exercise, then invasive risk stratification with an electrophysiology study should be considered.
APs capable of rapid anterograde conduction should be ablated to reduce the risk of sudden cardiac death, regardless of whether or not they cause supraventricular tachycardia.
A treadmill exercise test can be used as an indicator of risk of sudden death.
[Figure caption and citation for the preceding image starts]: Resting ECG shows delta waves (red arrows) in the inferior and lateral leadsFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: Loss of pre-excitation (delta waves) in inferior and lateral leads during exerciseFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Loss of pre-excitation (delta waves) in inferior and lateral leads during exerciseFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: Persistent loss of pre-excitation during the recovery period of exercise testing, suggestive of low-risk ECG for sudden cardiac deathFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Persistent loss of pre-excitation during the recovery period of exercise testing, suggestive of low-risk ECG for sudden cardiac deathFrom the collection of Dr Mithilesh K. Das [Citation ends].
Use of this content is subject to our disclaimer