Vigilância gastrointestinal
A vigilância gastrointestinal é recomendada para todos os pacientes.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://gut.bmj.com/content/69/3/411.long
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95.
https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
[22]Wagner A, Aretz S, Auranen A, et al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med. 2021 Jan 27;10(3):473.
https://www.mdpi.com/2077-0383/10/3/473/htm
http://www.ncbi.nlm.nih.gov/pubmed/33513864?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Obstrução do intestino delgado é uma das maiores causas de cirurgias e pode ser minimizada pela remoção de pólipos no intestino delgado.[35]Oncel M, Remzi FH, Church JM, et al. Benefits of "clean sweep" in Peutz-Jegher's patients. Colorectal Dis. 2004 Sep;6(5):332-5.
http://www.ncbi.nlm.nih.gov/pubmed/15335366?tool=bestpractice.com
[36]Edwards DP, Khosraviani K, Stafferton R, et al. Long-term results of polyp clearance by intraoperative enteroscopy in the Peutz-Jeghers syndrome. Dis Colon Rectum. 2003 Jan;46(1):48-50.
http://www.ncbi.nlm.nih.gov/pubmed/12544521?tool=bestpractice.com
[37]Zanoni EC, Averbach M, Borges JL, et al. Laparoscopic treatment of intestinal intussusception in the Peutz-Jeghers syndrome: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2003 Aug;13(4):280-2.
http://www.ncbi.nlm.nih.gov/pubmed/12960794?tool=bestpractice.com
Uma série retrospectiva sugere que o rastreamento de rotina e a polipectomia do trato gastrointestinal podem evitar a necessidade de uma cirurgia de emergência.[38]Latchford AR, Neale K, Phillips RK, et al. Peutz-Jeghers syndrome: intriguing suggestion of gastrointestinal cancer prevention from surveillance. Dis Colon Rectum. 2011 Dec;54(12):1547-51.
http://www.ncbi.nlm.nih.gov/pubmed/22067184?tool=bestpractice.com
As diretrizes europeias e dos EUA, junto com declarações de consenso de especialistas, fazem as seguintes recomendações relativas à vigilância gastrointestinal.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://gut.bmj.com/content/69/3/411.long
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95.
https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
[22]Wagner A, Aretz S, Auranen A, et al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med. 2021 Jan 27;10(3):473.
https://www.mdpi.com/2077-0383/10/3/473/htm
http://www.ncbi.nlm.nih.gov/pubmed/33513864?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
A videoendoscopia por cápsula (VEC) ou a enterografia por ressonância magnética (ERM) do intestino delgado deve começar aos 8 anos de idade (ou antes, se o paciente estiver sintomático). A endoscopia por cápsula é segura para uso em indivíduos com SPJ e polipose do intestino delgado que não apresentam sintomas obstrutivos. Se houver preocupação relativa à retenção de cápsula, uma cápsula biodegradável deve ser utilizada. Caso não sejam encontrados pólipos no exame inicial, as diretrizes dos EUA recomendam que a vigilância do intestino delgado seja restabelecida aos 18 anos de idade e continue a cada 2-3 anos ao longo da vida, enquanto as diretrizes europeias recomendam repetir a vigilância a cada 3 anos desde o início.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com
[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://gut.bmj.com/content/69/3/411.long
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95.
https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
[22]Wagner A, Aretz S, Auranen A, et al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med. 2021 Jan 27;10(3):473.
https://www.mdpi.com/2077-0383/10/3/473/htm
http://www.ncbi.nlm.nih.gov/pubmed/33513864?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
A endoscopia digestiva alta (EDA) e a colonoscopia para procurar pólipos do trato gastrointestinal superior ou colorretais devem ser realizadas aos 8 anos de idade. Se forem encontrados pólipos, ambos os exames são repetidos a cada 3 anos; se nenhum pólipo for detectado, um exame basal subsequente é realizado aos 18 anos de idade e a cada 3 anos a partir de então.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com
[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://gut.bmj.com/content/69/3/411.long
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
Excisão de pólipo
As diretrizes diferem em relação ao limiar e tamanho no qual os pólipos assintomáticos do intestino delgado devem ser removidos, embora todas concordem que qualquer pólipo sintomático deva ser removido, independente do tamanho. As diretrizes dos EUA recomendam a remoção de pólipos assintomáticos ≥10 milímetros de diâmetro, enquanto as diretrizes europeias recomendam um limiar maior de >15-20 milímetros.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com
[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://gut.bmj.com/content/69/3/411.long
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95.
https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
[22]Wagner A, Aretz S, Auranen A, et al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med. 2021 Jan 27;10(3):473.
https://www.mdpi.com/2077-0383/10/3/473/htm
http://www.ncbi.nlm.nih.gov/pubmed/33513864?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
A polipectomia é realizada via endoscopia alta ou enteroscopia por balão simples ou duplo, dependendo da localização dos pólipos. Uma série de 34 pacientes com polipose hamartomatosa no intestino delgado revelou que a enteroscopia por balão duplo foi bem-sucedida em mais de 80% dos pacientes e teve uma margem de segurança aceitável.[39]Gorospe EC, Alexander JA, Bruining DH, et al. Performance of double-balloon enteroscopy for the management of small bowel polyps in hamartomatous polyposis syndromes. J Gastroenterol Hepatol. 2013 Feb;28(2):268-73.
http://www.ncbi.nlm.nih.gov/pubmed/23190124?tool=bestpractice.com
A cirurgia pode ser necessária na presença de neoplasia, ou se o tamanho do pólipo ou o número impedir a remoção endoscópica. Ela também pode ser necessária em pacientes com intussuscepção ou obstrução do intestino delgado. Algumas autoridades recomendam uma tentativa de depurar o intestino delgado de pólipos durante a laparotomia, por meio de uma endoscopia intraoperatória com polipectomia ou, para pólipos maiores, por meio de enterotomia. Essa abordagem agressiva no diagnóstico e ressecção de pólipos do intestino delgado ("limpeza completa") foi associada a um maior intervalo entre cirurgias subsequentes e a uma diminuição no total de operações.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[35]Oncel M, Remzi FH, Church JM, et al. Benefits of "clean sweep" in Peutz-Jegher's patients. Colorectal Dis. 2004 Sep;6(5):332-5.
http://www.ncbi.nlm.nih.gov/pubmed/15335366?tool=bestpractice.com
[36]Edwards DP, Khosraviani K, Stafferton R, et al. Long-term results of polyp clearance by intraoperative enteroscopy in the Peutz-Jeghers syndrome. Dis Colon Rectum. 2003 Jan;46(1):48-50.
http://www.ncbi.nlm.nih.gov/pubmed/12544521?tool=bestpractice.com
[37]Zanoni EC, Averbach M, Borges JL, et al. Laparoscopic treatment of intestinal intussusception in the Peutz-Jeghers syndrome: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2003 Aug;13(4):280-2.
http://www.ncbi.nlm.nih.gov/pubmed/12960794?tool=bestpractice.com
Há dados limitados para orientar sobre o tamanho dos pólipos que devem ser submetidos à polipectomia no estômago ou no cólon.[13]Latchford A, Cohen S, Auth M, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):442-52.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Peutz_Jeghers_Syndrome_in_Children.31.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585892?tool=bestpractice.com
A US Multi-Society Task Force on Colorectal Cancer é a única organização que fornece uma recomendação específica; ela orienta a remoção de pólipos >5 milímetros de diâmetro e a tentativa de remoção de todos os pólipos, caso seja endoscopicamente viável.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
Às vezes, a colectomia é necessária e deve ser considerada se o manejo colonoscópico for difícil e, especialmente, se for encontrada alteração neoplásica em pólipos cólicos.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
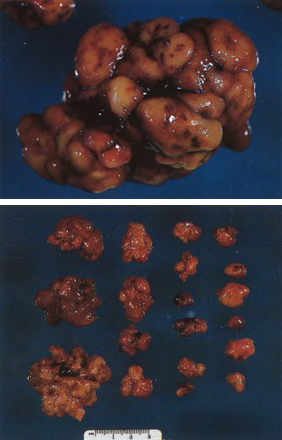
[Figure caption and citation for the preceding image starts]: Pólipo hamartomatoso identificado no intestino delgado por endoscopia por cápsulaDo acervo de Dra. Carol A. Burke, usado com permissão [Citation ends].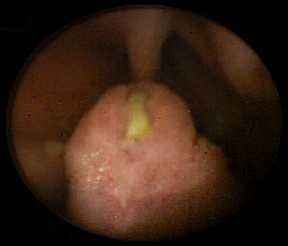 [Figure caption and citation for the preceding image starts]: Massa polipoide no intestino delgadoDo acervo do Dr. James Church, usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Massa polipoide no intestino delgadoDo acervo do Dr. James Church, usado com permissão [Citation ends]. [Figure caption and citation for the preceding image starts]: Ondulação serosa característica resultante de hamartoma pedunculado no intestino delgado de paciente com síndrome de Peutz-Jeghers (SPJ)Do acervo do Dr. James Church, usado com permissão [Citation ends].
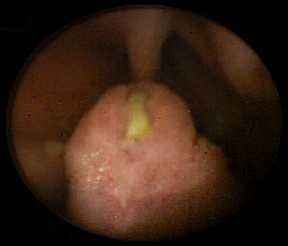
[Figure caption and citation for the preceding image starts]: Ondulação serosa característica resultante de hamartoma pedunculado no intestino delgado de paciente com síndrome de Peutz-Jeghers (SPJ)Do acervo do Dr. James Church, usado com permissão [Citation ends]. [Figure caption and citation for the preceding image starts]: Endoscopia intraoperatóriaDo acervo do Dr. James Church, usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Endoscopia intraoperatóriaDo acervo do Dr. James Church, usado com permissão [Citation ends]. [Figure caption and citation for the preceding image starts]: Coleta de pólipo hamartomatoso após 'limpeza completa'Do acervo do Dr. James Church, usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Coleta de pólipo hamartomatoso após 'limpeza completa'Do acervo do Dr. James Church, usado com permissão [Citation ends].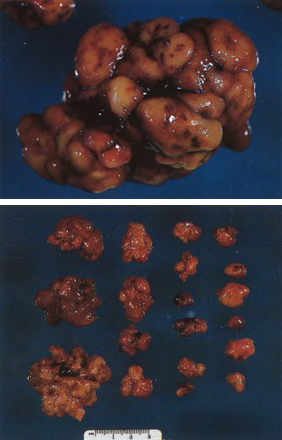
Vigilância para cânceres extraintestinais
Em pacientes com SPJ, o risco de desenvolvimento de qualquer forma de câncer ao longo da vida é estimado em até 93%.[1]van Lier MG, Wagner A, Mathus-Vliegen EM, et al. High cancer risk in Peutz-Jeghers syndrome: a systematic review and surveillance recommendations. Am J Gastroenterol. 2010 Jun;105(6):1258-64.
http://www.ncbi.nlm.nih.gov/pubmed/20051941?tool=bestpractice.com
Os riscos de ocorrência de cânceres específicos ao longo da vida incluem câncer de mama (40% a 85%), de pâncreas (11% a 36%), de ovário (21%), pulmonar (7% a 17%), cervical (10% a 23%) e de útero (9%).[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
Meninos e adolescentes do sexo masculino e, menos comumente, jovens, também correm risco de desenvolver câncer de testículo.[16]Giardiello FM, Bresinger JD, Tersmette AC, et al. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology. 2000 Dec;119(6):1447-53.
http://www.ncbi.nlm.nih.gov/pubmed/11113065?tool=bestpractice.com
As diretrizes de vigilância para cânceres extraintestinais em pacientes com síndrome de Peutz-Jeghers foram publicadas.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[19]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://gut.bmj.com/content/69/3/411.long
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[20]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019 Sep;51(9):877-95.
https://www.thieme-connect.com/products/ejournals/html/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Câncer de mama
O risco de câncer de mama em mulheres com SPJ é similar aos portadores de mutações do gene BRCA1 ou BRCA2 (risco vitalício de 40% a 85%).[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
A US Multi-Society Task Force on Colorectal Cancer recomenda o autoexame da mama mensal a partir dos 18 anos de idade, exame da mama clínico a cada dois anos a partir dos 25 anos de idade, ressonância nuclear magnética (RNM) da mama anual a partir dos 25-29 anos, e mamografia com consideração de tomossíntese (mamografia tridimensional) alternando a cada 6 meses com RNM da mama com contraste a partir dos 30-75 anos.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
A National Comprehensive Cancer Network (NCCN) recomenda mamografia e RNM anualmente, juntamente com um exame clínico das mamas a cada 6 meses, começando aproximadamente aos 30 anos de idade.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
A mastectomia profilática pode ser considerada de acordo com o caso.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
Câncer de pâncreas
O câncer de pâncreas é a terceira neoplasia maligna mais comum (depois do câncer de mama e colorretal) em indivíduos com SPJ, com risco vitalício de 11% a 36% de adenocarcinoma ductal pancreático.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Recomenda-se vigilância por ultrassonografia endoscópica (USE) e/ou RNM ou colangiopancreatografia por ressonância magnética (CPRM).O International Cancer of the Pancreas Screening Consortium recomenda exames de imagem do pâncreas a cada 1-2 anos a partir dos 40 anos.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[34]Canto MI, Harinck F, Hruban RH, et al. International Cancer of the Pancreas Screening (CAPS) Consortium summit on the management of patients with increased risk for familial pancreatic cancer. Gut. 2013 Mar;62(3):339-47.
https://gut.bmj.com/content/62/3/339.long
http://www.ncbi.nlm.nih.gov/pubmed/23135763?tool=bestpractice.com
A NCCN recomenda exames de imagem anuais do pâncreas com USE ou RNM/CPRM iniciando aos 30-35 anos de idade.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Cânceres ginecológicos
Os riscos vitalícios para câncer de ovário, útero e cervical são estimados em 21%, 9% e 10% a 23%, respectivamente.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
As diretrizes diferem em relação à idade recomendada para iniciar o rastreamento com exame pélvico, esfregaço cervical e ultrassonografia transvaginal; a NCCN recomenda o início aproximadamente aos 18-20 anos, e outras sociedades recomendam o início mais tardiamente, aos 25 anos.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Quase todos os cânceres de ovário em pacientes com SPJ são tumores do cordão sexual com túbulos anulares (TCSTA). Tais tumores podem causar menstruação irregular e puberdade precoce. Recomenda-se realizar um exame físico anual para verificar a presença de puberdade precoce a partir dos 8 anos de idade, bem como um exame pélvico e uma ultrassonografia pélvica anuais a partir dos 18-25 anos.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Para vigilância de câncer uterino, recomenda-se realizar um exame pélvico anual a partir dos 18-25 anos. O American College of Gastroenterology (ACG) recomenda a ultrassonografia transvaginal anual a partir dos 25 anos de idade.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
A NCCN não recomenda o rastreamento por ultrassonografia de rotina, mas recomenda a realização de uma biópsia do endométrio caso haja sangramento anormal.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Uma grande proporção de câncer cervical em pacientes com SPJ é adenocarcinoma com desvio mínimo (antes conhecido como adenoma maligno), um adenocarcinoma raro e bem diferenciado de difícil detecção com citologia em meio líquido, que tem prognóstico desfavorável. As diretrizes recomendam o exame pélvico anual e a citologia em meio líquido a partir dos 18-25 anos de idade (novamente, as diretrizes diferem em relação à idade em que os exames devem ser iniciados).[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
A NCCN também defende a consideração de uma histerectomia total após a mulher ter uma família completa.[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Câncer de testículo
Pacientes do sexo masculino com SPJ têm risco vitalício de 9% de desenvolver tumor de células de Sertoli, com idade média de 9 anos no diagnóstico.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Recomenda-se o exame testicular anual e a observação quanto a alterações feminizantes, com ultrassonografia testicular de acompanhamento se forem detectadas anormalidades. A idade em que isso deve começar é controversa; a Multi-Society Task Force on Colorectal Cancer dos EUA aconselha o rastreamento desde o nascimento, enquanto a NCCN recomenda uma idade inicial mais alta de aproximadamente 10 anos.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
Câncer pulmonar
O risco vitalício estimado de câncer pulmonar em pacientes com SPJ é de 7% a 17%.[4]Syngal S, Brand RE, Church JM, et al; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
https://journals.lww.com/ajg/Fulltext/2015/02000/ACG_Clinical_Guideline__Genetic_Testing_and.8.aspx
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
As diretrizes diferem em relação às recomendações de vigilância. A US Multi-Society Task Force on Colorectal Cancer e a NCCN recomendam simplesmente educar os pacientes sobre os sintomas e o abandono do hábito de fumar.[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
[33]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1436
No entanto, o American College of Chest Physicians, a American Society of Clinical Oncology e a American Cancer Society aconselham a tomografia computadorizada (TC) de baixa dose anualmente dos 55 aos 74 anos (com base no nível de risco cumulativo em pacientes com SPJ, que é semelhante a pessoas com história de tabagismo de mais de 30 anos-maços que abandonaram o hábito de fumar por 10-15 anos).[14]Boland CR, Idos GE, Durno C, et al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022 Jun;162(7):2063-85.
https://www.gastrojournal.org/article/S0016-5085(22)00151-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35487791?tool=bestpractice.com
As evidências que dão suporte a essas recomendações não são robustas. Na opinião dos autores, essa vigilância deve ser individualizada com base no fenótipo, na idade e incidência esperadas da doença, e na história familiar.
 [Figure caption and citation for the preceding image starts]: Massa polipoide no intestino delgadoDo acervo do Dr. James Church, usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Massa polipoide no intestino delgadoDo acervo do Dr. James Church, usado com permissão [Citation ends]. [Figure caption and citation for the preceding image starts]: Ondulação serosa característica resultante de hamartoma pedunculado no intestino delgado de paciente com síndrome de Peutz-Jeghers (SPJ)Do acervo do Dr. James Church, usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Ondulação serosa característica resultante de hamartoma pedunculado no intestino delgado de paciente com síndrome de Peutz-Jeghers (SPJ)Do acervo do Dr. James Church, usado com permissão [Citation ends]. [Figure caption and citation for the preceding image starts]: Endoscopia intraoperatóriaDo acervo do Dr. James Church, usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Endoscopia intraoperatóriaDo acervo do Dr. James Church, usado com permissão [Citation ends]. [Figure caption and citation for the preceding image starts]: Coleta de pólipo hamartomatoso após 'limpeza completa'Do acervo do Dr. James Church, usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Coleta de pólipo hamartomatoso após 'limpeza completa'Do acervo do Dr. James Church, usado com permissão [Citation ends].