Approach
The diagnosis of acute aspiration is primarily by history, bearing in mind the presence of risk factors, with confirmation when necessary by imaging studies. At times it can be witnessed: for example, during intubation or in a patient who is vomiting and then aspirates. The signs, symptoms, and imaging studies can be indistinguishable from pneumonia and other causes of acute respiratory distress syndrome (ARDS), so the possibility of gastric aspiration must be considered in high-risk patients.
History, physical exam, and lab tests
Aspiration usually takes place in the presence of risk factors, typically in patients ages >70 years who have comorbid conditions that may alter mental status, or in patients with a depressed level of consciousness due to intoxication, illness, or drugs. A sudden onset of fever, cough paroxysms, wheeze, laryngospasm, or cyanosis in at-risk patients should prompt consideration for acute aspiration. Aspiration in the setting of general anesthesia or intoxication, or in the intensive care unit, is also common, but may not present with overt symptoms. It may be silent and may only be apparent from the consequences of aspiration such as bronchospasm, hypoxia, bronchiolitis/bronchitis, pneumonia, atelectasis, fever, and even respiratory failure from noncardiogenic pulmonary edema.[37][41]
A complete blood count (CBC) and blood gas analysis can determine leukocytosis and hypoxia.
If pneumonia develops after the aspiration of gastric contents, hypoxia, leukocytosis, and other features of systemic inflammatory response may ensue, though these findings may not distinguish infection from more chemical pneumonitis. See Aspiration pneumonia.
Aspiration pneumonitis caused by barium sulfate should be suspected in patients who develop respiratory distress after upper gastrointestinal studies with barium. This is often directly visualized radiographically given the high-density material.[Figure caption and citation for the preceding image starts]: Bronchoscopy showing barium aspiration in a lung transplant patient in the right mainstem bronchus after a barium swallow studyFrom the collection of Dr Kamran Mahmood [Citation ends]. [Figure caption and citation for the preceding image starts]: Barium aspiration. A barium swallow was conducted in a 53-year-old woman. Imaging revealed hyperdense airway-centered material in the left lower lobe consistent with barium aspiration bronchiolitis. A tracheoesophageal fistula was confirmedFrom the collection of Dr Augustine Lee; used with permission of Mayo Foundation for Medical Education and Research, all rights reserved [Citation ends].
[Figure caption and citation for the preceding image starts]: Barium aspiration. A barium swallow was conducted in a 53-year-old woman. Imaging revealed hyperdense airway-centered material in the left lower lobe consistent with barium aspiration bronchiolitis. A tracheoesophageal fistula was confirmedFrom the collection of Dr Augustine Lee; used with permission of Mayo Foundation for Medical Education and Research, all rights reserved [Citation ends].
Chest x-ray
When aspiration of gastric contents results in aspiration pneumonitis or pneumonia, the chest x-ray reveals patchy, bilateral airspace consolidations with a perihilar and basilar distribution.[48] However, an estimated 25% of cases may not be apparent on chest x-rays relative to computed tomography (CT) imaging.[68] The right lung may be involved more frequently because of the obtuse angle between the trachea and the right main bronchus. The most commonly involved segments are the superior and posterobasal segments of the right lower lobe and the posterior segment of the right upper lobe because of their dependent location in the supine position. If the patient is in a different position, other segments can be involved.
Chest x-ray findings of aspiration pneumonitis usually develop within 2 hours of aspiration and sometimes resolve quickly. However, if pneumonia develops, opacities can become apparent days later and can take weeks to resolve.
Barium aspiration should be confirmed by chest x-ray, which may reveal hyperdense opacities in the mid and lower lungs, sometimes outlining the tracheobronchial tree, and more distally, with a bronchiolocentric or centrilobular pattern.[70][71][72][Figure caption and citation for the preceding image starts]: A. Portable upright chest x-ray before aspiration; B. Chest x-ray 1 hour after aspiration, showing bilateral diffuse alveolar infiltrates, worse at the bases on the right sideFrom the collection of Dr Henri Colt [Citation ends].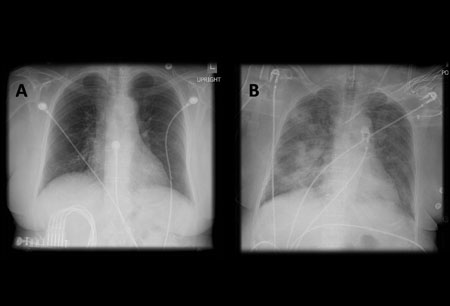 [Figure caption and citation for the preceding image starts]: Barium aspiration. A barium swallow was conducted in a 53-year-old woman. Imaging revealed hyperdense airway-centered material in the left lower lobe consistent with barium aspiration bronchiolitis. A tracheoesophageal fistula was confirmedFrom the collection of Dr Augustine Lee; used with permission of Mayo Foundation for Medical Education and Research, all rights reserved [Citation ends].
[Figure caption and citation for the preceding image starts]: Barium aspiration. A barium swallow was conducted in a 53-year-old woman. Imaging revealed hyperdense airway-centered material in the left lower lobe consistent with barium aspiration bronchiolitis. A tracheoesophageal fistula was confirmedFrom the collection of Dr Augustine Lee; used with permission of Mayo Foundation for Medical Education and Research, all rights reserved [Citation ends].
Chest CT
In cases of aspirated gastric content, chest CT may show opacities in the posterior segments of the upper lobes and the superior segments of the lower lobes. In advanced cases, the findings may be indistinguishable from those of ARDS. CT scanning precisely delineates the location of the lobar and segmental opacities. Aspiration of fat (exogenous lipoid pneumonia) or contrast material can sometimes be determined by measuring the tissue attenuation on CT scans. Lung abscess and empyema are potential complications of aspiration that are visualized better with CT than with plain chest x-ray.[73] See Lung abscess and Empyema.
Although chest x-ray is sufficient in most cases of aspiration, a CT chest should be ordered if foreign body aspiration is suspected (to plan extraction) or if the patient fails to improve with initial therapy (to rule out empyema or lung abscess). Chest CT is superior compared with chest x-ray in the detection of aspiration pneumonia, and if initial chest x-ray is inconclusive, CT should be ordered.[68]
[Figure caption and citation for the preceding image starts]: Lipoid pneumonia. A 77-year-old woman with dysphagia and achalasia following a stroke presented with recurrent lung infiltrates, including a persisting right middle lobe lesion. Hounsfield units (HU) measurement was -157, consistent with lipoid pneumonia. Comparative subcutaneous fat and aorta (blood/tissue) HU are shownFrom the collection of Dr Augustine Lee, used with permission of Mayo Foundation for Medical Education and Research, all rights reserved [Citation ends].
Bronchoscopy and bronchoalveolar lavage
Bronchoscopy can play both a diagnostic and therapeutic role. If the aspirated material is particulate or potentially obstructive, or if there is radiographic evidence of lobar or segmental collapse, the airway can be cleared and further evolution to ARDS may be avoided. In cases of aspiration of barium sulfate, especially if a patient has hypoxia or respiratory distress, early bronchoscopy may be helpful, but incurs some risk of disseminating the contrast to unaffected airways.[24][74][Figure caption and citation for the preceding image starts]: Bronchoscopy showing barium aspiration in a lung transplant patient in the right mainstem bronchus after a barium swallow studyFrom the collection of Dr Kamran Mahmood [Citation ends]. Another occasional therapeutic role besides airway and lung lavage is the potential placement of tracheal or bronchial stents in cases of tracheoesophageal fistula, as well as the placement of percutaneous tracheostomy for those with severe dysphagia.
Another occasional therapeutic role besides airway and lung lavage is the potential placement of tracheal or bronchial stents in cases of tracheoesophageal fistula, as well as the placement of percutaneous tracheostomy for those with severe dysphagia.
Aside from potential therapeutic roles, bronchoscopy is also important diagnostically. Bronchoalveolar lavage techniques or protected brush specimens can be used to identify, confirm, or refute the presence of an infection, which will have direct impact on the patient’s antibiotic management.[2] In addition to infection, bronchoalveolar lavage can diagnose acute eosinophilic pneumonia and diffuse alveolar hemorrhage, both of which can present similarly to acute aspiration with acute respiratory distress and lung infiltrates.[75] Occasionally, cytologic analysis can pick up unusual tumors that can appear pneumonic on imaging. When the differential is broader, a bronchoscopic biopsy may occasionally be employed for interstitial pneumonias and other considerations, though not often in the acute setting.[75] Finally, a careful bronchoscopic exam may be important to identify a tracheoesophageal fistula that may be complicating cancer, surgery, radiation, or trauma.
Biomarkers of aspiration syndromes
Multiple biomarkers are used in the research setting and at some centers. These have included the evaluation of lipid laden macrophages, pepsin, amylase, bile, and cytokines directly from lower airway samples.[40][76] The sensitivity and specificity of these markers remain unclear, and they lack clinical validation.[40]
Tests to identify need for antibiotics
Tests to identify a bacterial component to the pneumonic presentation depend on the clinical scenario and may include culture and sensitivities of samples obtained from bronchoalveolar lavage and brushing, venepuncture, or thoracentesis. See Aspiration pneumonia, Hospital-acquired pneumonia, Community-acquired pneumonia, Pleural effusion, Empyema, Lung abscess, and Sepsis in adults.
Use of this content is subject to our disclaimer