Recommendations
Key Recommendations
If the patient is having an acute aspiration event, see Acute aspiration.
A careful history is key to correctly diagnosing aspiration pneumonia. Consider aspiration pneumonia if the patient has clinical signs or symptoms of pneumonia (e.g., cough, breathlessness, fever, etc.) and a history of, or risk factors for, aspiration.[3]
Practical tip
Older patients often fail to mount the same systemic inflammatory response that younger patients do, so may not have a fever or raised white cell count.
Many patients may present with non-specific signs such as delirium, reduced appetite or mobility, and general debilitation.
Although acute illness is uncommon in aspiration pneumonia, think ‘Could this be sepsis?’ based on acute deterioration in an adult patient in whom there is clinical evidence or strong suspicion of infection.[48][49][50] See Sepsis in adults.
Use a systematic approach, alongside your clinical judgement, for assessment; urgently consult a senior clinical decision-maker (e.g., ST4 level doctor in the UK) if you suspect sepsis.[48][50][51][52]
Refer to local guidelines for the recommended approach at your institution for assessment and management of a patient with suspected sepsis.
During the COVID-19 pandemic, for patients with suspected or confirmed COVID-19 pneumonia, see Coronavirus disease 2019 (COVID-19).
Consider all patients with cough and fever or suggestive symptoms to have COVID-19 until proven otherwise. Pneumonia due to COVID-19 is not covered in this topic.
Order a chest x-ray and full blood count as first-line investigations for any patient with suspected aspiration pneumonia.
In addition, obtain a sputum sample for culture and Gram stain if possible, and blood culture. Note, it is often difficult to find a causative organism as many patients do not produce sputum, and antibiotics may already have been administered.[3]
Consider an arterial blood gas if the patient has worsening oxygenation, increased work of breathing, or other systemic signs of organ dysfunction.[3]
Aspiration pneumonia predominantly occurs in older adults. As such, the recommendations in this topic are principally referring to practice in adults.
If the patient is having an acute aspiration event, see Acute aspiration.
During the COVID-19 pandemic, for patients with suspected or confirmed COVID-19 pneumonia with symptoms and signs that start at any point after hospital admission, see Coronavirus disease 2019 (COVID-19).
Consider all patients with cough and fever or suggestive symptoms to have COVID-19 until proven otherwise. COVID-19 viral pneumonia may be more likely if the patient presents with:[54]
A history of typical COVID-19 symptoms for about a week
Severe myalgia
Anosmia
Breathlessness
Absence of pleuritic pain.
Pneumonia due to COVID-19 is not covered in this topic.
Distinguishing aspiration pneumonia from other pneumonias (community- or hospital-acquired) is difficult; seek advice from a senior colleague if you are unsure.[6] Consider the following:
Aspiration pneumonia is unlikely if the patient has an uncompromised immune system[55]
Many patients who have an episode of aspiration develop a chemical pneumonitis rather than aspiration pneumonia.[56]
Practical tip
Be aware that patients with risk factors for aspiration such as swallowing dysfunction may have community-acquired pneumonia rather than aspiration pneumonia.
Take a focused history; this is especially important because witnessed aspiration is not seen in the majority of patients.
Risk factors for aspiration pneumonia can be classified according to the underlying mechanism, which can cause aspiration pneumonia due to:
Aspiration of oral secretions:
Swallowing dysfunction (e.g., stroke, dementia, epilepsy, multiple sclerosis, Parkinson’s disease, motor neuron disease)
Impaired conscious level
General anaesthetic or oropharyngeal procedures
Gastrointestinal (GI) disease (e.g., upper GI surgery, hiatal hernia) and conditions that affect gastric emptying (e.g., obesity, pregnancy)
Poor cough (e.g., upper airway problems such as pharyngeal pouches and vocal cord palsies, neuromuscular disease)
Aspiration pneumonia is a poor prognostic sign in patients with neuromuscular disease[8]
Poor oral hygiene
Learning disability
Reflux/vomiting:
General anaesthetic or oropharyngeal procedures
Recumbent position during enteral feeding
Polytrauma
Head and neck cancers.
Symptoms include cough, breathlessness, and pleuritic chest pain, but may be non-specific and be present for 1 week or more after aspiration. Rigors or a more acute presentation is uncommon. The patient may have a history of vomiting.
Look for signs such as fever, crepitations, tachypnoea, and frothy or purulent sputum, which may indicate aspiration pneumonia.
Sputum is foul smelling if there is infection by anaerobes, although anaerobic infection is less commonly observed than in prior decades.[8][14][15][16]
Many patients may present with non-specific signs such as delirium, reduced appetite or mobility, and general debilitation.
Practical tip
Think 'Could this be sepsis?' based on acute deterioration in an adult patient in whom there is clinical evidence or strong suspicion of infection.[48][49][50] See Sepsis in adults.
The patient may present with non-specific or non-localised symptoms (e.g., acutely unwell with a normal temperature) or there may be severe signs with evidence of multi-organ dysfunction and shock.[48][49][50]
Remember that sepsis represents the severe, life-threatening end of infection.[59]
Use a systematic approach (e.g., National Early Warning Score 2 [NEWS2]), alongside your clinical judgement, to assess the risk of deterioration due to sepsis.[48][49][51][60] Consult local guidelines for the recommended approach at your institution.
Arrange urgent review by a senior clinical decision-maker (e.g., ST4 level doctor in the UK) if you suspect sepsis:[52]
Within 30 minutes for a patient who is critically ill (e.g., NEWS2 score of 7 or more, evidence of septic shock, or other significant clinical concerns).
Within 1 hour for a patient who is severely ill (e.g., NEWS2 score of 5 or 6).
Follow your local protocol for investigation and treatment of all patients with suspected sepsis, or those at risk. Start treatment promptly. Determine urgency of treatment according to likelihood of infection and severity of illness, or according to your local protocol.[52]
In the community: refer for emergency medical care in hospital (usually by blue-light ambulance in the UK) any patient who is acutely ill with a suspected infection and is:[50]
Deemed to be at high risk of deterioration due to organ dysfunction (as measured by risk stratification)
At risk of neutropenic sepsis.
Check the patient’s ability to cough and clear the pharynx/larynx. Always consider aspiration pneumonia if a patient has a poor cough and has symptoms or signs of pneumonia.
The initial tests for aspiration pneumonia are essentially the same as those for typical pneumonia.
Chest x-ray (CXR)
Order CXR as a first-line investigation, even in the absence of significant pulmonary symptoms, to look for a new infiltrate or atelectasis in dependent regions of the lungs.
[Figure caption and citation for the preceding image starts]: Early ill-defined opacities of the right upper lobe above the minor fissure consistent with early changes of aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].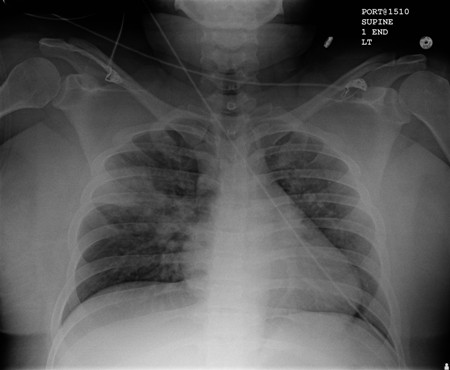 [Figure caption and citation for the preceding image starts]: Increased opacification of the right perihilar region and superior segment of the right lower and upper lobes consistent with worsening aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Increased opacification of the right perihilar region and superior segment of the right lower and upper lobes consistent with worsening aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].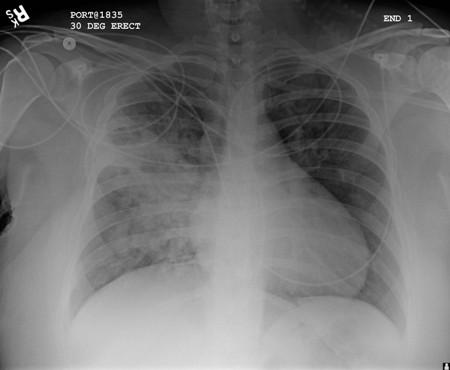 Note that a chest x-ray fails to detect aspiration pneumonia in up to 25% of cases when compared with thoracic computed tomography.[3][53]
Note that a chest x-ray fails to detect aspiration pneumonia in up to 25% of cases when compared with thoracic computed tomography.[3][53]
Full blood count (FBC)
Order FBC as a first-line investigation.
Leukocytosis is often present, but may be absent in older adults.[61]
Always check for neutrophilia in the presence of a normal white cell count.[62]
Arterial blood gas (ABG)
Consider ABG based on the patient’s clinical status (e.g., worsening oxygenation, increased work of breathing, and other systemic signs of organ dysfunction).
Urea and electrolytes
Recommended by the British Thoracic Society as part of the diagnostic work-up.[3]
Electrolytes may be deranged.
Liver function tests (LFTs)
Recommended by the British Thoracic Society as part of the diagnostic work-up.[3]
Abnormal LFTs are common in community-acquired pneumonia. Low albumin or raised alanine aminotransferase (ALT) are indicators of a higher mortality, or prolonged hospital admission.[63]
C-reactive protein (CRP)
Recommended by the British Thoracic Society as part of the diagnostic work-up.[3]
Elevated CRP may point to a diagnosis of pneumonia, over other causes of respiratory tract infection.[64]
Sputum Gram stain and culture
Always send a sputum sample for Gram stain and culture where possible.
Gram stain is recommended because of the low cost and ease of obtaining the sample. Gram stain may reveal white blood cells and mixed bacterial flora. The Gram stain result is often inconclusive, although occasionally it may verify the infecting organism.
Although sputum cultures are not specifically indicated and their results are not very informative, they are routinely performed due to the lack of other available diagnostic tests. They are inexpensive and a non-invasive way to obtain a bacterial specimen. However, testing requires an adequate specimen (i.e., uncontaminated by saliva), which may be difficult to obtain. Most culture results are inconclusive. Culture results usually fail to grow common pulmonary pathogens. Results may guide therapy if organism identification and sensitivities are available.
More info: Blood cultures
Blood cultures are recommended by the British Thoracic Society in instances of suspected aspiration pneumonia.[3] However, antibiotic administration should not be delayed in favour of blood cultures. As such, and as aspiration pneumonia is an acute event, blood cultures are usually taken after the administration of antibiotics, and thus unreliable.
Bronchoscopy
Bronchoscopy may be used in large-volume particulate aspirates or if a foreign body or lobar collapse is suspected as a cause of airway obstruction, but there are no studies showing benefits of such an intervention.[65] Protected brush specimens have been used only in research studies trying to identify an aetiology for aspiration pneumonia; the impact of such an intervention in managing aspiration pneumonia has not been determined. For aspiration pneumonia, particularly in a nursing home or a hospital setting, obtaining a good sputum or lower respiratory tract sample is currently recommended as per the guidelines for hospital-acquired pneumonia.[21][66]
Use of this content is subject to our disclaimer