Approach
If the patient presents with symptoms suggestive of tension pneumothorax, immediate intervention is required and can be lifesaving.
Patients generally have a more indolent presentation, typically describing dyspnea and chest pain. The degree of shortness of breath depends on patients preexisting lung disease and degree of hypoxia and pain the pneumothorax causes. The size of the pneumothorax does not necessarily correlate to the symptom presentation.
Risk factors for the development of spontaneous pneumothorax, such as the presence of chronic respiratory diseases, should be assessed.[1] Because Pneumocystis jirovecii pulmonary infection can result in a pneumothorax, the patient should also be questioned about risk factors for HIV infection.[27]
Clinical presentation
Tension pneumothorax
Patients complain of severe and worsening dyspnea and are distressed, with rapid labored respirations, cyanosis, profuse diaphoresis, and tachycardia. It can progress to shock and ultimately death if no intervention is taken.
It requires immediate intervention to decompress (needle or open) the involved hemithorax.[1][35]
Needle decompression of tension pneumothorax: animated demonstrationHow to decompress a tension pneumothorax. Demonstrates insertion of a large-bore intravenous cannula into the fourth intercostal space in an adult.
Primary spontaneous pneumothorax
Patients usually complain of a sudden onset of dyspnea and ipsilateral chest pain. The severity of the dyspnea is related to the volume of air in the pleural space.
Most primary spontaneous pneumothoraces occur at rest. The patient can, therefore, often recall the exact time when the pneumothorax developed.[39]
In some cases the typical symptoms of chest pain and dyspnea may be minor or even absent, meaning that a high index of suspicion is needed.
Secondary spontaneous pneumothorax
Patients complain of dyspnea and ipsilateral chest pain. Due to the underlying lung disease, their symptoms are typically more severe than those associated with primary spontaneous pneumothorax.[35]
Catamenial pneumothoraces are usually right-sided, believed to be related to peritoneal flow of fluid in a clockwise fashion making endometrial tissue more likely to implant on the right. A high index of suspicion for this should be maintained in women of childbearing age and if there is concomitant hemoptysis or pleural effusion.[25]
Pneumothorax ex vacuo
Due to the airway obstruction, the patient may complain of cough. Dyspnea may be related to the amount of collapsed lung and/or the volume of air in the pleural space.
Can also be a signal of nonexpandable lung, whether from entrapment from an ongoing process (i.e., malignant pleural effusion leading to a visceral pleural rind), or trapped lung from a resolved process (i.e., empyema that was treated with antibiotics but never drained).
Physical exam
Tension pneumothorax
Findings are similar to those seen with a large spontaneous pneumothorax; however, the involved hemithorax is larger with intercostal interspace widening, hyper-resonance is noted with percussion, and the trachea shifts toward the contralateral hemithorax.
The development of a tension pneumothorax is usually heralded by a sudden deterioration in the cardiopulmonary status of the patient. Loss of consciousness may follow quickly as blood flow to the brain is compromised.[1]
Primary spontaneous pneumothorax
Findings include decreased chest excursion, ipsilateral hyperinflation of the hemithorax with diminished breath sounds, and hyper-resonance on percussion.[1]
Secondary spontaneous pneumothorax
Findings are the same as in primary spontaneous pneumothorax; however, due to the patient's underlying respiratory disorder, the physical findings are less reliable.[1] Examination may also elicit findings related to the underlying respiratory condition.
Catamenial pneumothoraces are usually right-sided. The diagnosis is not difficult if the possibility is considered.[24]
Pneumothorax ex vacuo
Findings include diminished breath sounds and hyper-resonance on percussion. The chest, however, is not hyperexpanded.[4]
Imaging
Tension pneumothorax is considered a medical emergency. If a tension pneumothorax is clinically suspected, the involved hemithorax should be decompressed (needle or open) immediately. Valuable time should not be wasted waiting for radiographic confirmation, though point of care ultrasound (POCUS) showing a lack of lung sliding is consistent with pneumothorax and can aid in quick decision-making for intervention.[40] A delay in intervention may result in the death of the patient.[1]
A chest x-ray (CXR) is generally recommended as first-line test in most other pneumothoraces, and shows a visceral pleural line.[41] Expiratory radiographs are not recommended for routine diagnosis.[41] In secondary spontaneous pneumothorax the pleural line may be difficult to visualize because the adjacent diseased lung may be hyperlucent (e.g., in patients with emphysematous changes). In addition, it may be difficult to distinguish a large, thin-walled bulla from a pneumothorax. In this situation it may be necessary to obtain a computed tomography (CT) scan of the chest to confirm the diagnosis.[41][Figure caption and citation for the preceding image starts]: Anterior-posterior chest x-ray demonstrating a right pneumothoraxFrom the collection of Dr Ryland P. Byrd [Citation ends].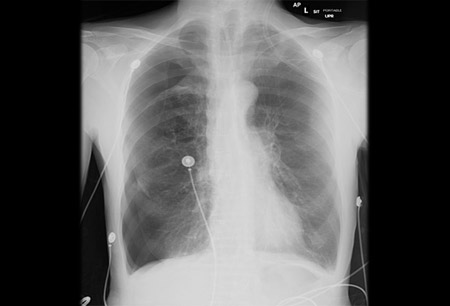
For pneumothorax ex vacuo, in addition to the presence of a visceral pleural line, ipsilateral loss of volume and lung atelectasis are present. CT may demonstrate an endobronchial obstruction.[Figure caption and citation for the preceding image starts]: Entrapped lung with pneumothorax ex-vacuo. This patient had a malignant pleural effusion that had developed a thick visceral pleural cortical rind preventing re-expansion. Chest tube was for pleural effusion removal, not evacuation of air.From the personal collection of Chris Kapp, MD; used with permission [Citation ends].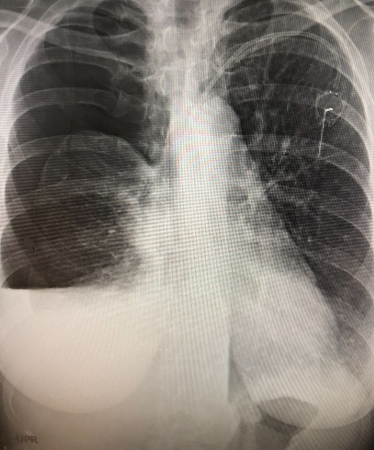
Chest ultrasound appears to be useful in the detection of pneumothoraces in adult blunt chest trauma victims who are immobilized, when upright posteroanterior chest radiographs cannot be obtained.[42] In one Cochrane review, chest ultrasound had a sensitivity of 91% and a specificity of 99% (compared with a sensitivity of 47% and a specificity of 100% for CXR) for detecting pneumothoraces in trauma patients in the emergency department. The authors concluded that chest ultrasound is superior to supine CXR, independent of the type of trauma, type of chest ultrasonography operator, or type of chest ultrasonography probe used, and they recommended that chest ultrasound is included in trauma protocols (e.g., advanced trauma life support [ATLS]).[43] The absence of lung sliding (see figure below) is a sensitive, though not specific finding for pneumothorax and discovery of a lung point is a specific marker for pneumothorax as it describes the point where the parietal and visceral pleura stop opposing one another.[40] In fact, POCUS is more sensitive than a single view CXR in detecting pneumothorax post-lung biopsy, occult pneumothoraces in the emergency department, and provides better confirmation of resolution of a pneumothorax than a CXR.
[Figure caption and citation for the preceding image starts]: POCUS of the lung in a large pneumothorax. Shown is the ultrasound view showing A-lines that are reverberations of the pleural line. There is a lack of B-lines, which is also consistent with a pneumothorax. M-mode is placed on the patient and shows a ‘barcode sign’ confirming presence of air in the pleural spaceFrom the personal collection of Chris Kapp, MD; used with permission [Citation ends].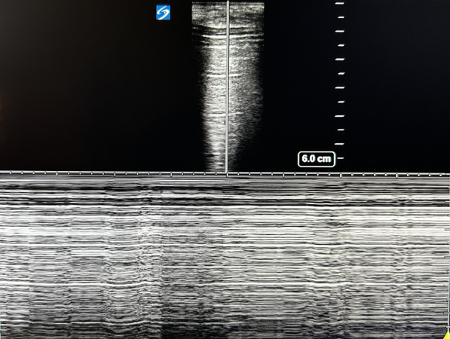
A CT scan of the chest is more sensitive than a chest radiograph or ultrasound in detecting pneumothoraces.[44] It is often used in patients with multiple traumatic injuries or where an occult pneumothorax is suspected.
Other tests
If a pneumothorax ex vacuo is suspected, a bronchoscopy may be necessary to establish the diagnosis and to remove the endobronchial obstruction.[45]
Use of this content is subject to our disclaimer
