SJS and TEN are similar to second-degree burns in terms of physiologic effects.
Treatment requires a multidisciplinary team so that patients receive optimal daily wound care, nutrition, critical care, pain management, and supportive care.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Transfer to a burn center, a specialized wound care center, or a dermatology intensive care unit is recommended for patients with SJS/TEN.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Exact treatment will depend on the extent of skin involvement, but the same general principles are applicable to both SJS and TEN. Treatment should be initiated on a case-by-case basis depending on individual patient presentation.[76]Zimmermann S, Sekula P, Venhoff M, et al. Systemic immunomodulating therapies for Stevens-Johnson syndrome and toxic epidermal necrolysis: a systematic review and meta-analysis. JAMA Dermatol. 2017 Jun 1;153(6):514-22.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5817620
http://www.ncbi.nlm.nih.gov/pubmed/28329382?tool=bestpractice.com
[77]Schneider JA, Cohen PR. Stevens-Johnson syndrome and toxic epidermal necrolysis: a concise review with a comprehensive summary of therapeutic interventions emphasizing supportive measures. Adv Ther. 2017 Jun;34(6):1235-44.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5487863
http://www.ncbi.nlm.nih.gov/pubmed/28439852?tool=bestpractice.com
Both conditions have a tendency to progress over the course of several days, so patients should be monitored closely.
Immediate care
Upon diagnosis, the causative agent should be identified and withdrawn immediately. Usually it will be a new medication started in the 2-3 weeks prior to onset of the rash.
Drugs most frequently implicated in SJS/TEN are listed in the etiology section. See Etiology.
Patients with SJS/TEN should be assessed in the same way as a patient with cutaneous burns, using a structured approach to evaluate airway, breathing, and circulation. See Cutaneous burns (Diagnosis approach).
Arterial blood gases and oxygen saturation will help determine patient clinical respiratory status.
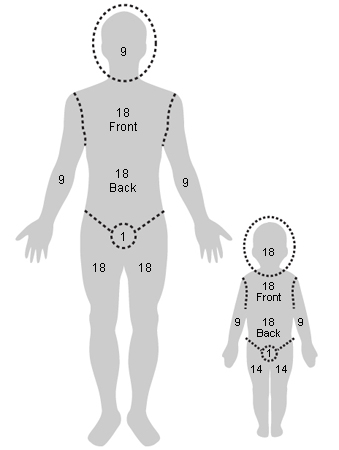
An immediate assessment of total body surface area (TBSA) involvement is required to assess severity of disease. Various methods can be used, such as the Wallace rule of 9s, Palmer, the Lund-Browder burn estimate chart, or SCORTEN.[55]Lund CC, Browder NC. The estimation of areas of burns. Surg Gynecol Obst. 1944;79:352-8.[57]Wachtel TL, Berry CC, Wachtel EE, et al. The inter-rater reliability of estimating the size of burns from various burn area chart drawings. Burns. 2000 Mar;26(2):156-70.
http://www.ncbi.nlm.nih.gov/pubmed/10716359?tool=bestpractice.com
Wallace rule of 9s
Opens in new window See Diagnosis approach.
[Figure caption and citation for the preceding image starts]: Rule of ninesFrom Dr Sheridan's personal collection [Citation ends].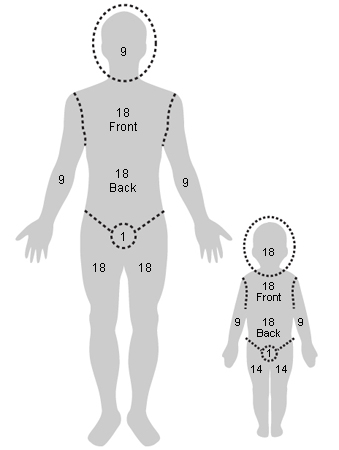
[Figure caption and citation for the preceding image starts]: Lund-Browder diagramFrom Dr Sheridan's personal collection [Citation ends].
The greater the percentage of TBSA involved, the greater the fluid requirement.[56]Hettiaratchy S, Papini R. Initial management of a major burn: II - assessment and resuscitation. BMJ. 2004 Jul 10;329(7457):101-3.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC449823
http://www.ncbi.nlm.nih.gov/pubmed/15242917?tool=bestpractice.com
Consider intubation and early tracheostomy in patients with oral involvement and one of the following:[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Initial body surface area (BSA) 70% or more
Progression of BSA involved from day of hospitalization (DOH) 1 to DOH 3 of ≥15%
Underlying neurologic diagnosis prevents airway protection
Documented airway involvement on direct laryngoscopy.
Evidence suggests that for patients who are intubated, mortality rates increase to over 50%.[54]de Prost N, Mekontso-Dessap A, Valeyrie-Allanore L, et al. Acute respiratory failure in patients with toxic epidermal necrolysis: clinical features and factors associated with mechanical ventilation. Crit Care Med. 2014 Jan;42(1):118-28.
http://www.ncbi.nlm.nih.gov/pubmed/23989174?tool=bestpractice.com
Provided the patient does not require therapeutic anticoagulation on admission, immobile patients should receive prophylactic low molecular weight heparin.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Mechanical thromboprophylaxis with graduated compression stockings or intermittent pneumatic compression is recommended for acutely ill patients at increased risk of thrombosis who are bleeding or at high risk for major bleeding.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Patients at high risk of bleeding, and those in whom enteral nutrition cannot be established, should be given a proton-pump inhibitor to prevent stress-related gastritis and intestinal ulceration.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Potential oral, ocular, and urogenital involvement should be evaluated as part of the initial assessment of all patients with SJS/TEN.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Wound care
Wound care can follow either a conservative or surgical approach to debridement depending on the needs of the individual patient.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Conservative management (antishear strategy) recommends:[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Preserving the detached epidermis as a biologic dressing
Limiting dressing changes
Using an air-fluidized bed
Using nonadherent dressings
Using lysis and drainage of wounds only for patient comfort
Cleansing wounds with sterile water, normal saline, or dilute chlorhexidine when dressings are changed
Applying an emollient to the whole epidermis to enhance skin barrier function, reduce fluid loss, and encourage re-epithelialization
Considering use of nonadherent, silver-impregnated primary dressings for antibacterial properties, reduced requirement for dressing changes, and improved patient comfort
Using secondary absorptive dressings to control exudate.
The surgical approach for wound care for SJS/TEN patients generally follows practice in burn management: once the surgical debridement of detached epidermis is achieved, wounds are covered with a biologic dressing, such as xenograft (pigskin), allograft (cadaver skin), or synthetic dressing.[78]Nizamoglu M, Ward JA, Frew Q, et al. Improving mortality outcomes of Stevens Johnson syndrome/toxic epidermal necrolysis: a regional burns centre experience. Burns. 2018 May;44(3):603-11.
http://www.ncbi.nlm.nih.gov/pubmed/29029855?tool=bestpractice.com
With healing, consider a nonadherent silver-impregnated dressing for dressing changes and improved patient comfort.
UK guidance recommends that patients should be transferred to burn unit for surgical debridement and wound care if they have TEN (>30% BSA epidermal loss) and evidence of the following:[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Once the skin has regenerated (after about 2-3 weeks) emollients can be useful to keep it supple and prevent drying out.
Fluid management
If a patient is vomiting frequently, dehydration may occur. In addition, depending on the extent of the skin sloughing, the patient may be losing significant amounts of fluids through the denuded skin surface. Electrolyte and fluid balance should be monitored daily.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
If the patient can take fluids orally, encourage them to do so. Otherwise, start intravenous fluids such as lactated Ringer solution or 0.9% sodium chloride to hydrate the patient. One case series study indicates that approximately 2 mL/kg/% TBSA may be adequate if there are no other complications.[79]Shiga S, Cartotto R. What are the fluid requirements in toxic epidermal necrolysis? J Burn Care Res. 2010 Jan-Feb;31(1):100-4.
http://www.ncbi.nlm.nih.gov/pubmed/20061843?tool=bestpractice.com
Regardless of the calculated quantity of fluid required, the clinical evaluation of patient response is extremely important. Fluid resuscitation is monitored by urine output. It is important that an adult has a urine output of 0.5 mL/kg/hour (30-50 mL/hour) and children weighing <30 kg have an output of 1 mL/kg/hour.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Increase or decrease fluid resuscitation based on the urine output.
Management of pain
Analgesia should be given based on the severity of symptoms to ensure comfort at rest. Pain level should be evaluated once every 4 hours, and assessed at least once daily using a validated pain tool.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Patients will require more pain medication during dressing changes.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
If mild pain is not controlled with acetaminophen, an oral opioid such as tramadol should be considered.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Morphine or fentanyl may be necessary for patients with moderate to severe pain scores. Low-dose ketamine can be considered as an alternative or adjuvant therapy for SJS/TEN pain.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Gabapentin and pregabalin both address neuropathic pain and may decrease opioid consumption in both the acute and healing phases for patients with SJS.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Nonsteroidal anti-inflammatory drugs should be avoided due to the increased risk of renal or gastric injury.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Intravenous immune globulin and cyclosporine
There are no clear indications regarding administration of intravenous immune globulin (IVIG). Some clinicians give IVIG to patients with a rapidly progressing rash involving at least 6% TBSA. Others only give IVIG when 20% TBSA is affected. There are no definitive randomized controlled trials to guide treatment. The current literature consists of small retrospective and prospective series. Reviews of these small clinical trials have shown some benefit and no major complications with the use of IVIG.[2]Dodiuk-Gad RP, Chung WH, Valeyrie-Allanore L, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis: an update. Am J Clin Dermatol. 2015 Dec;16(6):475-93.
http://www.ncbi.nlm.nih.gov/pubmed/26481651?tool=bestpractice.com
[24]Mockenhaupt M. Stevens-Johnson syndrome and toxic epidermal necrolysis: clinical patterns, diagnostic considerations, etiology, and therapeutic management. Semin Cutan Med Surg. 2014 Mar;33(1):10-6.
http://www.ncbi.nlm.nih.gov/pubmed/25037254?tool=bestpractice.com
[42]Schwartz RA, McDonough PH, Lee BW. Toxic epidermal necrolysis. Part I: introduction, history, classification, clinical features, systemic manifestations, etiology, and immunopathogenesis. J Am Acad Dermatol. 2013 Aug;69(2):173.
http://www.ncbi.nlm.nih.gov/pubmed/23866878?tool=bestpractice.com
[44]Schwartz RA, McDonough PH, Lee BW. Toxic epidermal necrolysis. Part II: prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J Am Acad Dermatol. 2013 Aug;69(2):187.
http://www.ncbi.nlm.nih.gov/pubmed/23866879?tool=bestpractice.com
[80]Barron SJ, Del Vecchio MT, Aronoff SC. Intravenous immunoglobulin in the treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis: a meta-analysis with meta-regression of observational studies. Int J Dermatol. 2015 Jan;54(1):108-15.
http://www.ncbi.nlm.nih.gov/pubmed/24697283?tool=bestpractice.com
[81]Aires DJ, Fraga G, Korentager R, et al. Early treatment with nonsucrose intravenous immunoglobulin in a burn unit reduces toxic epidermal necrolysis mortality. J Drugs Dermatol. 2013 Jun 1;12(6):679-84.
http://www.ncbi.nlm.nih.gov/pubmed/23839186?tool=bestpractice.com
[82]Enk A, Hadaschik E, Eming R, et al. European guidelines (S1) on the use of high-dose intravenous immunoglobulin in dermatology. J Dtsch Dermatol Ges. 2017 Feb;15(2):228-41.
http://www.ncbi.nlm.nih.gov/pubmed/28036140?tool=bestpractice.com
For SJS/TEN overlap and TEN patients, many burn centers give IVIG when there is rapid progression of the rash, and when the patient is clinically deemed a candidate.
There have been sporadic case reports of successful treatment of TEN with cyclosporine. In a retrospective chart review of 71 patients with SJS/TEN, cyclosporine was associated with fewer deaths than expected (standardized mortality ratio 0.43) while IVIG was associated with excess mortality (standardized mortality ratio 1.43).[83]Kirchhof MG, Miliszewski MA, Sikora S, et al. Retrospective review of Stevens-Johnson syndrome/toxic epidermal necrolysis treatment comparing intravenous immunoglobulin with cyclosporine. J Am Acad Dermatol. 2014 Nov;71(5):941-7.
http://www.ncbi.nlm.nih.gov/pubmed/25087214?tool=bestpractice.com
Another study of 16 patients treated with cyclosporine demonstrated a lower mortality rate than predicted by the SCORTEN score.[84]Balai M, Meena M, Mittal A, et al. Cyclosporine in Stevens-Johnson syndrome and toxic epidermal necrolysis: experience from a tertiary care centre of South Rajasthan. Indian Dermatol Online J. 2021 Jan-Feb;12(1):116-22.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7982025
http://www.ncbi.nlm.nih.gov/pubmed/33768032?tool=bestpractice.com
Results from one small (n=29) phase 2 open-label trial suggest that cyclosporine can reduce mortality and the progression of epidermal detachment among patients with SJS/TEN. There was one death in a small study of 12 patients with an average TBSA of 77% treated with cyclosporine and plasmapheresis.[85]Valeyrie-Allanore L, Wolkenstein P, Brochard L, et al. Open trial of ciclosporin treatment for Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2010 Oct;163(4):847-53.
http://www.ncbi.nlm.nih.gov/pubmed/20500799?tool=bestpractice.com
Other meta-analyses suggest that cyclosporine use in epidermal necrolysis is effective in reducing the risk of death.[76]Zimmermann S, Sekula P, Venhoff M, et al. Systemic immunomodulating therapies for Stevens-Johnson syndrome and toxic epidermal necrolysis: a systematic review and meta-analysis. JAMA Dermatol. 2017 Jun 1;153(6):514-22.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5817620
http://www.ncbi.nlm.nih.gov/pubmed/28329382?tool=bestpractice.com
[86]Ng QX, De Deyn MLZQ, Venkatanarayanan N, et al. A meta-analysis of cyclosporine treatment for Stevens-Johnson syndrome/toxic epidermal necrolysis. J Inflamm Res. 2018 Mar 28;11:135-42.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5880515
http://www.ncbi.nlm.nih.gov/pubmed/29636627?tool=bestpractice.com
[87]González-Herrada C, Rodríguez-Martín S, Cachafeiro L, et al. Cyclosporine use in epidermal necrolysis is associated with an important mortality reduction: evidence from three different approaches. J Invest Dermatol. 2017 Oct;137(10):2092-100.
https://www.jidonline.org/article/S0022-202X(17)31645-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/28634032?tool=bestpractice.com
[88]Roujeau JC, Mockenhaupt M, Guillaume JC, et al. New evidence supporting cyclosporine efficacy in epidermal necrolysis. J Invest Dermatol. 2017 Oct;137(10):2047-9.
https://www.jidonline.org/article/S0022-202X(17)32758-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/28941473?tool=bestpractice.com
Oral involvement
Oral involvement occurs in the majority of patients with SJS/TEN, resulting in pain, impaired oral intake, and poor oral hygiene. Patients should have an oral exam on presentation and on a daily basis during the acute phase of the illness.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Applying petrolatum ointment on the lips every 2 hours throughout the acute illness is recommended.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Pain management
To provide short-term pain relief, oral rinses or sprays with local anesthetic, anti-inflammatory, and analgesic properties (e.g., viscous lidocaine, benzydamine) should be given, particularly before eating or oral cleansing.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Topical oral coating agents are recommended for pain reduction in patients with oral mucosal involvement.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Oral hygiene
The patient’s mouth should be cleaned daily with warm saline mouthwashes or an oral sponge.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
To reduce bacterial colonization of the mucosa an antiseptic oral rinse should be used (e.g., diluted chlorhexidine).[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Either a potent topical corticosteroid mouthwash (e.g., dexamethasone) or an ultrapotent topical corticosteroid ointment is recommended during the acute phase of the illness.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Nutrition
Nutritional support should be administered orally if possible. For patients unable to tolerate oral intake, provide enteral feeding through a nasogastric tube.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Nasogastric tube placement should be avoided in patients with nasopharyngeal mucosa involvement.
Nutritional support of 30-35 kcal/kg should be delivered, maintaining close glycemic control.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
If the patient's caloric intake is not sufficient with enteral nutrition, it should be supplemented via the parenteral route.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Ocular involvement
All patients manifesting signs and symptoms of SJS/TEN should have an ophthalmologic consultation and a full exam upon admission, and on a daily basis during the acute phase of illness, until it is established that there is no visual deterioration.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
[89]Gregory DG. New grading system and treatment guidelines for the acute ocular manifestations of Stevens-Johnson syndrome. Ophthalmology. 2016 Aug;123(8):1653-8.
http://www.ncbi.nlm.nih.gov/pubmed/27297404?tool=bestpractice.com
Follow-up should be determined on a case-by-case basis.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Ocular lubricants (drops and ointments) should be administered every 2 hours during the acute stage of illness for patients with ocular involvement.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Daily exam of the entire ocular surface (eyelid skin, eyelid margin, conjunctiva, and cornea) is recommended.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
This should include assessing for forniceal and tarsal conjunctival epithelial defects and early symblephara by everting the eyelids with eyes rotated.
All patients should have fluorescein staining to detect corneal injuries, small foreign objects or particles in the eye, and abnormal tear production.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Resting eyelid position should be assessed for lagophthalmos, especially in unconscious patients, as prevention of corneal exposure is essential.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Amniotic membrane transplantation should be considered during the initial evaluation of any patient thought to have SJS/TEN, and at each follow-up exam during the acute phase.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Coverage of the entire ocular surface with amniotic membrane, together with intensive short-term topical corticosteroids, during the acute phase of SJS and TEN has been shown to be associated with preservation of good visual acuity and an intact ocular surface.[89]Gregory DG. New grading system and treatment guidelines for the acute ocular manifestations of Stevens-Johnson syndrome. Ophthalmology. 2016 Aug;123(8):1653-8.
http://www.ncbi.nlm.nih.gov/pubmed/27297404?tool=bestpractice.com
Urogenital involvement
Urogenital involvement occurs in approximately 70% of women and men with SJS/TEN.[90]Van Batavia JP, Chu DI, Long CJ, et al. Genitourinary involvement and management in children with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Pediatr Urol. 2017 Oct;13(5):490.e1-7.
http://www.ncbi.nlm.nih.gov/pubmed/28314701?tool=bestpractice.com
[91]Meneux E, Wolkenstein P, Haddad B, et al. Vulvovaginal involvement in toxic epidermal necrolysis: a retrospective study of 40 cases. Obstet Gynecol. 1998 Feb;91(2):283-7.
http://www.ncbi.nlm.nih.gov/pubmed/9469290?tool=bestpractice.com
This can result in erosions of the scrotum/labia, penis/vulva; dysuria; hematuria; urinary retention; and long-term sequelae such as urethral stenosis and scarring, xerosis, phimosis, dyspareunia, chronic pain, bleeding, sexual dysfunction, infertility, and anxiety.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Exam of the urogenital tract of all patients with SJS/TEN is recommended upon initial assessment and daily during hospitalization.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
A urinary catheter should be inserted if urogenital involvement is causing significant dysuria/retention.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
The vulvar/urogenital skin/mucosa should be coated with an ointment and/or ointment gauze to help reduce pain, reduce adhesion formation, and facilitate healing during the acute phase of the disease.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
For women with suspected vaginal involvement, an intravaginal dilator can be used to apply either:[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
A nonsteroidal ointment (e.g., petrolatum jelly), with reapplication as frequently as necessary to maintain barrier protection, and/or
A high-potency corticosteroid ointment if active inflammation is observed.
Tapering of the topical corticosteroid should be based on clinical improvement.
If vaginal candidiasis is suspected, obtain a potassium hydroxide preparation and fungal culture and initiate treatment with a suitable antifungal medication.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Medication can be alternated with estrogen cream to encourage healing of the vaginal mucosa.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Intravaginal dilators can be in place for a maximum of 24 hours before replacement.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
If patients are not comfortable using an intravaginal dilator, medication can be applied with a vaginal applicator.
Menstrual suppression may reduce the risk of vaginal adenosis and endometriosis and can be considered in women with severe genital mucosal involvement.[75]Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020 Jun;82(6):1553-67.
http://www.ncbi.nlm.nih.gov/pubmed/32151629?tool=bestpractice.com
Occupational and physical therapy
Patients can develop limitations in mobility with decreased strength. Arrange for daily exercises within the patient's capability with a physical therapist and, if needed, an occupational therapist.[44]Schwartz RA, McDonough PH, Lee BW. Toxic epidermal necrolysis. Part II: prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J Am Acad Dermatol. 2013 Aug;69(2):187.
http://www.ncbi.nlm.nih.gov/pubmed/23866879?tool=bestpractice.com