Aetiology
SJS may be a consequence of a disease process or medication use. A thorough history is essential.
Several aetiological factors exist.
1. Infection
SJS can be a sequela of several conditions, including:[19][20][21]
Upper respiratory tract infections
Pharyngitis
Otitis media
Mycoplasma pneumoniae
Herpes
Epstein-Barr virus
Cytomegaloviruses.
2. Vaccination
3. Medicine
The most frequent drugs implicated in SJS and TEN are:[10][15][19][24][25][26][27][28][29][30][31][32][33][34][35][36][37][38][39]
Anticonvulsants (e.g., carbamazepine, phenobarbital, phenytoin, valproic acid, lamotrigine)
Antibiotics (e.g., sulfonamides, aminopenicillins, fluoroquinolones, cephalosporins)
Antifungals
Antiretrovirals (e.g., nevirapine, abacavir) and antivirals (e.g., aciclovir)
Anthelmintics
Analgesics (e.g., paracetamol)
Non-steroidal anti-inflammatory drugs and selective COX-2 inhibitors
Antimalarials
Azathioprine
Sulfasalazine
Allopurinol
Tranexamic acid
Corticosteroids
Psychotropic agents
Chlormezanone
Anticancer drugs (e.g., bendamustine, busulfan, chlorambucil)
Targeted therapy (e.g., rituximab, imatinib, vemurafenib)
Retinoids.
Pathophysiology
Although there is general agreement that SJS and TEN result from an immunological response, the exact pathophysiology of the interactions between drugs, their metabolites, viruses, cytokines, lymphocytes, genetic predisposition, pharmacogenomics, and keratinocyte apoptosis has not been fully unravelled.
Both SJS and TEN are characterised by the detachment of epidermis from the papillary dermis at the epidermal-dermal junction, manifesting as a papulomacular rash and bullae as a result of keratinocyte apoptosis.[40][41][Figure caption and citation for the preceding image starts]: Histopathology of Stevens-Johnson syndrome/toxic epidermal necrolysisFrom the personal collection of Dr A. Kowal-Vern [Citation ends].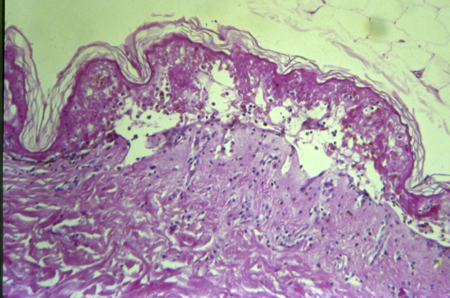 Keratinocyte apoptosis mediated by cytotoxic T-lymphocytes (CD8) in SJS and TENS is modulated by plasma tumour necrosis factor-alpha and interferon-gamma, which are increased in patients with SJS and TEN.[42][43] This process is currently hypothesised to occur through 3 possible pathways:[24][42][44][45][46][47]
Keratinocyte apoptosis mediated by cytotoxic T-lymphocytes (CD8) in SJS and TENS is modulated by plasma tumour necrosis factor-alpha and interferon-gamma, which are increased in patients with SJS and TEN.[42][43] This process is currently hypothesised to occur through 3 possible pathways:[24][42][44][45][46][47]
Fas-Fas ligand interaction
Perforin/granzyme B
Granulysin-mediated.
The main pathway is thought to be granulysin-mediated, but the issue remains controversial and the potential involvement of one or several pathways has not been resolved.
There are markers under investigation that may correlate with SJS/TEN disease severity and serve as possible mediators and biomarkers for diagnosis: a protein, galectin-7, and receptor-interacting kinase 3 (RIP3).[48][49]
Progress in delineating the pathophysiology of SJS/TEN has addressed the possible risk factors interacting with natural killer and cytotoxic T-cells, such as drug structure and metabolism (CYP), and the immunogenic characteristics of the human leukocyte antigen molecules.[2]
There may be multiple pathways at play depending on the genetic disposition of the patient and/or the type of drug precipitating the immunological response.
Classification
Cutaneous Involvement Spectrum - clinically accepted classification[3]
There is no formal classification. It is considered that there is a spectrum of exfoliative diseases, with the mild form being erythema multiforme major, the severe form being TEN, and SJS the mid-point. This has now become a clinically accepted definition and classification of the disease spectrum.
Erythema multiforme major
Target lesions
SJS
<10% total body surface area (TBSA) involvement.
SJS/TEN overlap
10% to 30% TBSA involvement.
TEN
>30% TBSA involvement.
Use of this content is subject to our disclaimer