Approach
Assess burn severity by the burn size (% total body surface area [TBSA]) and depth (first to fourth degree). Associated injuries, such as inhalation injury or trauma, adversely affect the prognosis.
Initially sort burn patients into those who can be reasonably managed in the outpatient setting and those who require inpatient care. This important practicality is based on:
A proper and complete evaluation of the patient
A careful evaluation of the wound.
Most burn injuries are minor, and patients are discharged following outpatient treatment.
Evaluation of the patient
Systematically evaluate burn patients using the primary and secondary surveys recommended by the American Burn Association alongside any immediately necessary treatment.
Primary survey (ABCDE):[24]
Airway maintenance; with cervical spine protection if a fall or blunt force trauma is suspected.
Breathing and ventilation.
Circumferential full-thickness burns of the trunk and neck may impair ventilation and require close monitoring.
Circulation and cardiac status.
Increased circulating catecholamines often elevate the adult heart rate to 100-120 bpm; higher heart rates may indicate hypovolemia from an associated trauma, inadequate oxygenation, or unrelieved pain or anxiety.
Abnormal cardiac rhythms may be due to electrical injuries, underlying cardiac abnormalities or electrolyte imbalances.
Circulation in a limb with a circumferential or nearly circumferential full-thickness burn may be impaired by oedema.
Typical indicators of compromised circulation (pain, pallor, paresthesia) may not be reliable in a burned extremity.
Absence of a radial pulse below an upper limb circumferential burn suggests impaired circulation.
Disability, neurological deficit and gross deformity. Typically, the patient with burns is initially alert and oriented. If not, consider associated injury, carbon monoxide poisoning, substance abuse, hypoxia, or pre-existing medical conditions.
Determine the patient’s level of consciousness using the AVPU method:
A – Alert
V – Responds to verbal stimuli
P – Respond only to painful stimuli
U – Unresponsive
The Glasgow Coma Scale (GCS) is a more definitive tool used to assess the depth and duration of coma and should be used to follow the patient’s level of consciousness.
Exposure and environmental control. Expose and completely undress the patient, and examine for major associated injuries. Stop the burning process, if applicable
Maintain a warm environment to prevent hypothermia.[25]
Secondary survey: (burn-specific; begins after the primary survey is completed and after initial fluids are started):[24]
History (injury circumstances including time and mechanism of injury, and medical history) and accurate pre-injury weight.
Complete head-to-toe evaluation of the patient.
Determination of burn severity, including percentage TBSA burned and burn depth.
Initial investigations to assess for dysfunction of other organ systems, or establish baseline function (e.g., full blood count [FBC], metabolic panel including urea and glucose).
Consideration of the possibility of abuse or neglect.
Consideration of associated trauma, with additional specialised tests (e.g, blood tests, imaging) as needed.
Management elements of the secondary survey include further adjustment and monitoring of fluid resuscitation (after TBSA determination), pain and anxiety management, psychosocial support, and wound care. See Management approach for further details.
The burn may be the most obvious injury, but other serious and life-threatening injuries may be present. A thorough history and physical examination are necessary to ensure that all injuries and pre-existing diseases are identified.[24]
Evaluation for abuse or neglect
Consider the possibility of abuse or neglect as the injury mechanism as part of the evaluation of every burn patient.[26] Although more common in young children, abuse is also seen in the setting of domestic violence. File suspicious injuries with the appropriate government agency.[27]
Data can be obtained during the initial evaluation and may be helpful later. This includes water temperature (if there is scalding), duration of contact, caretakers involved, conflicting reports from involved caretakers, delay in seeking treatment, and prior injuries.[28]
Important points of examination include uniformity of burn depth, absence of splash marks, sharply defined wound margins, porcelain contact sparing (which occurs when flesh in forced contact with a basin or bath is protected from the surrounding hot water), flexor sparing, stocking or glove patterns, dorsal location of contact burns of the hand, and localised very deep contact burns.[29] Stressful social circumstances are often a factor.[30] Child maltreatment has been shown to be associated with TBSA burned >20%, and with burns of the lower limbs.[31] Photographic documentation is ideal.
Admit patients to hospital for evaluation even if the injury is of little physiological significance. Consider screening radiography.
Evaluation of the burn wound
Make initial estimates of burn wound extent and depth.[32] Although a wide variety of devices have been advocated to help determine burn depth and vascularity, none have been widely adopted, as burn thickness and vascularity are only two of the many variables that determine the likelihood of a burn to heal, which is the variable that drives decision-making in burn care. Note the presence of fully or near-circumferential components. Decisions regarding outpatient care, hospitalisation, or transfer depend on this information.
Burn extent:
Most accurately estimated using a Lund-Browder diagram that compensates for changes in body proportions with age [Figure caption and citation for the preceding image starts]: Lund-Browder diagramFrom Dr Sheridan's personal collection [Citation ends].
A simpler alternative is the 'rule of nines': [Figure caption and citation for the preceding image starts]: Rule of ninesFrom Dr Sheridan's personal collection [Citation ends].
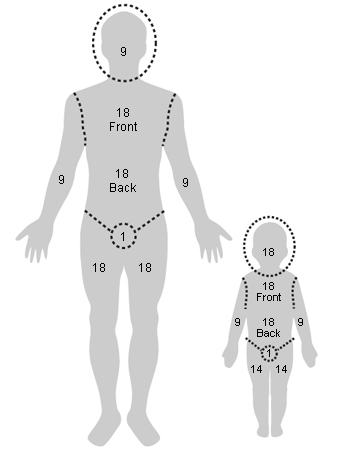
The head and neck represents 9% TBSA (18% in infants)
Each lower extremity is 18% (15% in infants)
Each upper extremity is 9% (10% in infants)
The anterior and posterior torso are 18% each (16% in infants), and
For scattered or irregular burns the palmar surface of the patient's hand represents approximately 1%.
Burn depth:
First-degree burns [Figure caption and citation for the preceding image starts]: First-degree burnFrom Dr Sheridan's personal collection [Citation ends].

Erythema involving the epidermis only
Usually dry and painful.
Second-degree burns [Figure caption and citation for the preceding image starts]: Second-degree burnFrom Dr Sheridan's personal collection [Citation ends].

Superficial partial-thickness burns involving the epidermis and upper dermis
Deep partial-thickness burns involving the epidermis and dermis
Usually wet and painful.
Third-degree burns [Figure caption and citation for the preceding image starts]: Third-degree burnFrom Dr Sheridan's personal collection [Citation ends].

Full-thickness burns involving the epidermis and dermis and damage to appendages
Usually dry and insensate.
Fourth-degree burns [Figure caption and citation for the preceding image starts]: Fourth-degree burnFrom Dr Sheridan's personal collection [Citation ends].

Involve underlying subcutaneous tissue, tendon, or bone.
Burns are commonly deeper than they appear at first examination, so often it is prudent to describe initial impressions and re-evaluate wounds the following day.[33]
Burn location:
Near- or completely circumferential burns should be identified for special monitoring [Figure caption and citation for the preceding image starts]: Circumferential burnFrom Dr Sheridan's personal collection [Citation ends].

If involving the torso, such wounds can interfere with ventilation, or even contribute to intra-abdominal hypertension
When burns involve an extremity, limb-threatening ischaemia may occur 12 to 24 hours after the injury.
Burn wound sepsis:
Can be diagnosed by clinical examination, cultures of wound biopsies, and burn wound histology. Most authors advocate diagnosis by clinical examination only
Most common organisms are Staphylococcus aureus and Pseudomonas aeruginosa
A classification scheme includes:[34]
'Burn impetigo' or superficial infection with loss of epithelium (usually associated with S aureus and Streptococcus pyogenes and particularly common in burns of the scalp)
Open burn-related surgical wound infection (develops in excised wounds and donor sites)
Burn wound cellulitis (spreading dermal infection in uninjured skin around a burn wound or donor site)
Invasive burn wound infection.
Investigations in patients with significant burns
Inspect the globes of the eyes prior to the development of facial oedema, which can make evaluation difficult. A clouded cornea suggests a serious burn. Subtle corneal burns require fluorescein staining. Any suspicion of eye injury warrants an ophthalmological consultation.
A computed tomography scan of the head and axial spine may be indicated based on injury mechanism and history.
The torso should be assessed for stiffness and expansion. Extensive and deep torso burns can interfere with ventilation and may require escharotomy. Rarely, usually in patients with very large injuries and delayed resuscitation, abdominal compartment syndrome can develop.
Carboxyhaemoglobin and arterial blood gas determinations are important if inhalation injury is suspected.
Initial routine electrolyte and haematological testing may be useful.
Use of this content is subject to our disclaimer