Characteristic clinical presentation and skin biopsy results are sufficient to diagnose SJS/TEN. Consider transfer to a burn unit in more severe cases.
History
A thorough history is essential, focusing on recent drug or medication use, bacterial or viral infection, and vaccinations. Common historic factors associated with SJS and TEN include comorbidities such as seizures, systemic lupus erythematosus, HIV-positivity, collagen vascular disease, active cancer, and certain treatments including radiation therapy and bone marrow transplantation.[50]Ziemer M, Kardaun SH, Liss Y, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis in patients with lupus erythematosus: a descriptive study of 17 cases from a national registry and review of the literature. Br J Dermatol. 2012 Mar;166(3):575-600.
http://www.ncbi.nlm.nih.gov/pubmed/22014091?tool=bestpractice.com
[51]Vern-Gross TZ, Kowal-Vern A. Erythema multiforme, Stevens Johnson syndrome, and toxic epidermal necrolysis syndrome in patients undergoing radiation therapy: a literature review. Am J Clin Oncol. 2014 Oct;37(5):506-13.
http://www.ncbi.nlm.nih.gov/pubmed/22892429?tool=bestpractice.com
[52]Demiral AN, Yerebakan O, Simsir V, et al. Amifostine-induced toxic epidermal necrolysis during radiotherapy: a case report. Jpn J Clin Oncol. 2002 Nov;32(11):477-9.
http://jjco.oxfordjournals.org/cgi/content/full/32/11/477
http://www.ncbi.nlm.nih.gov/pubmed/12499421?tool=bestpractice.com
The most frequently implicated drugs for SJS/TEN are listed in the etiology section. See Etiology.
The most common anticonvulsants precipitating SJS and TEN are carbamazepine, phenobarbital, phenytoin, lamotrigine, and valproic acid.[25]Roujeau JC, Kelly JP, Naldi L, et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995 Dec 14;333(24):1600-7.
https://www.nejm.org/doi/10.1056/NEJM199512143332404
http://www.ncbi.nlm.nih.gov/pubmed/7477195?tool=bestpractice.com
[26]Calabrese JR, Sullivan JR, Bowden CL, et al. Rash in multicenter trials of lamotrigine in mood disorders: clinical relevance and management. J Clin Psychiatry. 2002 Nov;63(11):1012-9.
http://www.ncbi.nlm.nih.gov/pubmed/12444815?tool=bestpractice.com
SJS and TEN usually develop in individuals who have started taking the medication for 1-14 days as a new drug; if drugs are used for months or years, the risk for developing SJS and TEN usually occurs in the first 2 months of treatment.[24]Mockenhaupt M. Stevens-Johnson syndrome and toxic epidermal necrolysis: clinical patterns, diagnostic considerations, etiology, and therapeutic management. Semin Cutan Med Surg. 2014 Mar;33(1):10-6.
http://www.ncbi.nlm.nih.gov/pubmed/25037254?tool=bestpractice.com
[26]Calabrese JR, Sullivan JR, Bowden CL, et al. Rash in multicenter trials of lamotrigine in mood disorders: clinical relevance and management. J Clin Psychiatry. 2002 Nov;63(11):1012-9.
http://www.ncbi.nlm.nih.gov/pubmed/12444815?tool=bestpractice.com
The index day for developing SJS and TEN is less than 1 month after starting medication (15 days for carbamazepine, 24 days for phenytoin, 17 days for phenobarbital).[24]Mockenhaupt M. Stevens-Johnson syndrome and toxic epidermal necrolysis: clinical patterns, diagnostic considerations, etiology, and therapeutic management. Semin Cutan Med Surg. 2014 Mar;33(1):10-6.
http://www.ncbi.nlm.nih.gov/pubmed/25037254?tool=bestpractice.com
Assessment of disease severity
Pulmonary status
Patients with SJS/TEN should be assessed in the same way as a patient with cutaneous burns, using a structured approach to evaluate airway, breathing, and circulation. See Cutaneous burns (Diagnosis approach).
One potential complication of SJS/TEN is mucosal involvement of the upper and lower respiratory tract, with vesicle formation, ulceration, and mucosal sloughing that may lead to laryngeal stridor, along with possible retractions and edema of the nasopharynx. If there is respiratory distress or edema of the oropharyngeal tissues, intubation may be necessary to maintain the airway.[54]de Prost N, Mekontso-Dessap A, Valeyrie-Allanore L, et al. Acute respiratory failure in patients with toxic epidermal necrolysis: clinical features and factors associated with mechanical ventilation. Crit Care Med. 2014 Jan;42(1):118-28.
http://www.ncbi.nlm.nih.gov/pubmed/23989174?tool=bestpractice.com
Arterial blood gases and oxygen saturation will help determine the patient's clinical respiratory status.
Total body surface area (TBSA)
Determination of the TBSA percent affected by SJS/TEN is important for severity assessment. Various methods have been used.
Wallace's rule of 9s SJS/TEN
[Figure caption and citation for the preceding image starts]: Rule of ninesFrom Dr Sheridan's personal collection [Citation ends].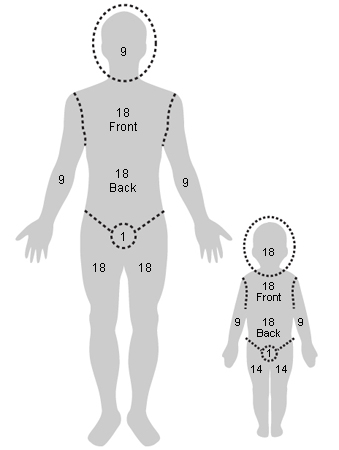
This provides a quick approximation of the area of skin burnt.[55]Lund CC, Browder NC. The estimation of areas of burns. Surg Gynecol Obst. 1944;79:352-8. Arbitrarily, it divides the body into units of surface area divisible by 9, with the exception of the perineum. Usually, charts of area are available in most burn units.
Wallace rule of 9s
Opens in new window
In an adult, the following are the respective percentages of the TBSA:
Head and neck total for front and back: 9%
Each upper limb total for front and back: 9%
Thorax and abdomen front: 18%
Thorax and abdomen back: 18%
Perineum: 1%
Each lower limb total for front and back: 18%.
The rule of 9s is relatively accurate for adults but not for children, because of the relative disproportion of body-part surface area.
Palmar surface
The surface area of a patient's palm (including fingers) is roughly 0.8% of TBSA. Palmar surface can be used to estimate relatively small burns (<15% of total surface area) or very large burns (>85%, when unburnt skin is counted). For medium-sized burns, it is inaccurate.[56]Hettiaratchy S, Papini R. Initial management of a major burn: II - assessment and resuscitation. BMJ. 2004 Jul 10;329(7457):101-3.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC449823
http://www.ncbi.nlm.nih.gov/pubmed/15242917?tool=bestpractice.com
Lund-Browder burn estimate chart
[Figure caption and citation for the preceding image starts]: Lund-Browder diagramFrom Dr Sheridan's personal collection [Citation ends]. This chart compensates for the variation in body shape with age, and therefore can give an accurate assessment of burns area in children.[55]Lund CC, Browder NC. The estimation of areas of burns. Surg Gynecol Obst. 1944;79:352-8.[57]Wachtel TL, Berry CC, Wachtel EE, et al. The inter-rater reliability of estimating the size of burns from various burn area chart drawings. Burns. 2000 Mar;26(2):156-70.
http://www.ncbi.nlm.nih.gov/pubmed/10716359?tool=bestpractice.com
This chart compensates for the variation in body shape with age, and therefore can give an accurate assessment of burns area in children.[55]Lund CC, Browder NC. The estimation of areas of burns. Surg Gynecol Obst. 1944;79:352-8.[57]Wachtel TL, Berry CC, Wachtel EE, et al. The inter-rater reliability of estimating the size of burns from various burn area chart drawings. Burns. 2000 Mar;26(2):156-70.
http://www.ncbi.nlm.nih.gov/pubmed/10716359?tool=bestpractice.com
SCORTEN
Starting within the first 24 hours of hospitalization, and continued for the first 5 days of admission, this severity of illness score is supposed to predict the risk of mortality for patients who develop SJS/TEN. The patient gets 1 point for each of the following:[58]Sekula P, Liss Y, Davidovici B, et al. Evaluation of SCORTEN on a cohort of patients with Stevens-Johnson Syndrome and toxic epidermal necrolysis included in the RegiSCAR study. J Burn Care Res. 2011 Mar-Apr;32(2):237-45.
http://www.ncbi.nlm.nih.gov/pubmed/21228709?tool=bestpractice.com
[59]Guegan S, Bastuji-Garin S, Poszepczynska-Guigne E, et al. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol. 2006 Feb;126(2):272-6.
https://www.jidonline.org/article/S0022-202X(15)32753-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/16374461?tool=bestpractice.com
Age >40 years
Malignancy
>120 bpm tachycardia
Initial % TBSA >10%
Serum BUN >10 mmol/L
Serum glucose >14 mmol/L
HCO3 <20 mmol/L.
Although the group originating the SCORTEN score, and some others, have found the scoring system useful, others have not.[60]Cartotto R, Mayich M, Nickerson D, et al. SCORTEN accurately predicts mortality among toxic epidermal necrolysis patients treated in a burn center. J Burn Care Res. 2008 Jan-Feb;29(1):141-6.
http://www.ncbi.nlm.nih.gov/pubmed/18182912?tool=bestpractice.com
[61]George SM, Harrison DA, Welch CA, et al. Dermatological conditions in intensive care: a secondary analysis of the Intensive Care National Audit and Research Centre (ICNARC) case mix programme database. Crit Care. 2008;12(suppl 1):S1.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2607109
http://www.ncbi.nlm.nih.gov/pubmed/19105799?tool=bestpractice.com
[62]Imahara SD, Holmes JH, Heimbach DM, et al. SCORTEN overestimates mortality in the setting of a standardized treatment protocol. J Burn Care Res. 2006 May-Jun;27(3):270-5.
http://www.ncbi.nlm.nih.gov/pubmed/16679892?tool=bestpractice.com
More than likely, the more frequent recent use of intravenous immune globulin in these patients has impacted some of the validity of this scoring system for TEN.
Physical exam
When patients present in the early course of disease, signs and symptoms may appear relatively mild. However, the condition typically progresses over several days, so close monitoring and regular reassessment is essential.
Initial symptoms include a sudden rash or a rash that develops after a new medication is started. There is a wide variation of lesion type and skin involvement. Common sites of skin involvement are:[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Upper torso
Proximal limbs
Face
Lesions spread from these sites to involve the rest of the trunk and distal limbs; involvement of the palms of the hands and soles of the feet is often prominent.[20]Auquier-Dunant A, Mockenhaupt M, Naldi L, et al. Correlations between clinical patterns and causes of erythema multiforme majus, Stevens-Johnson syndrome, and toxic epidermal necrolysis: results of an international prospective study. Arch Dermatol. 2002 Aug;138(8):1019-24.
http://www.ncbi.nlm.nih.gov/pubmed/12164739?tool=bestpractice.com
[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Blisters or macules and flat atypical target lesions, diffuse erythema, and Nikolsky sign (epidermal layer easily sloughs off when pressure is applied to the affected area) may be noted.[20]Auquier-Dunant A, Mockenhaupt M, Naldi L, et al. Correlations between clinical patterns and causes of erythema multiforme majus, Stevens-Johnson syndrome, and toxic epidermal necrolysis: results of an international prospective study. Arch Dermatol. 2002 Aug;138(8):1019-24.
http://www.ncbi.nlm.nih.gov/pubmed/12164739?tool=bestpractice.com
[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Mucosal involvement presents with erosions or ulceration of the eyes, lips, mouth, pharynx, esophagus, gastrointestinal tract, kidneys, liver, anus, genital area, or urethra.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Other potential presenting features include:
Fever
Swelling of the tongue
Diarrhea
Vomiting
Dysuria
Enlarged lymph nodes
Arthralgias
Arthritis
Bronchitis
Shortness of breath
Wheezing
Hypotension
Dehydration.
Laboratory tests and imaging
Laboratory tests include:[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Complete blood count
Metabolic panel (glucose, electrolytes [phosphate/magnesium], blood urea nitrogen, creatinine, calcium, bicarbonate)
Liver function tests (alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, total protein, albumin)
C-reactive protein (CRP)
Coagulation studies
Arterial blood gas and saturation of oxygen - to assess for respiratory compromise
Blood culture - to rule out toxic shock syndrome and scalded skin syndrome, which would show positive culture for Staphylococcus or Streptococcus species
Skin swab from lesional skin
Mycoplasma serology
Skin biopsy - definitive test for SJS, SJS/TEN overlap, and TEN (assessed in conjunction with clinical presentation).[19]Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994 Nov 10;331(19):1272-85.
http://www.ncbi.nlm.nih.gov/pubmed/7794310?tool=bestpractice.com
A dermatologist should take a biopsy at the transition point of blistering, to assess the level of skin desquamation. The separation will occur at the epidermal-papillary dermal junction, with the presence of necrotic cells and lymphocytes.
Direct immunofluorescence - may be performed on the perilesional biopsy to exclude autoimmune blistering disease.[2]Dodiuk-Gad RP, Chung WH, Valeyrie-Allanore L, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis: an update. Am J Clin Dermatol. 2015 Dec;16(6):475-93.
http://www.ncbi.nlm.nih.gov/pubmed/26481651?tool=bestpractice.com
[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
Do not order erythrocyte sedimentation rate (ESR) to detect acute phase inflammation. Order CRP instead as it is more sensitive and specific than ESR for detecting the acute phase of inflammation in patients with SJS/TEN. In the first 24 hours of a disease process, CRP will be elevated, whereas ESR may be normal. If the source of inflammation is removed, CRP will return to normal within a day or so, whereas ESR will remain elevated for several days until excess fibrinogen is removed from the serum.[64]American Society for Clinical Pathology. Thirty five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2021 [internet publication].
https://web.archive.org/web/20230316185857/https://www.choosingwisely.org/societies/american-society-for-clinical-pathology
Imaging tests
Due to the high risk of pneumonia and interstitial pneumonitis all patients should have a chest x-ray.[63]Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016 Jun;174(6):1194-227.
https://onlinelibrary.wiley.com/doi/10.1111/bjd.14530
http://www.ncbi.nlm.nih.gov/pubmed/27317286?tool=bestpractice.com
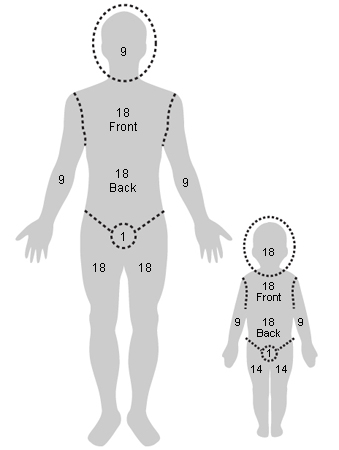
 This chart compensates for the variation in body shape with age, and therefore can give an accurate assessment of burns area in children.[55][57]
This chart compensates for the variation in body shape with age, and therefore can give an accurate assessment of burns area in children.[55][57]