Approach
Diagnosis of dystonia is based on physical examination, and distinguishing it from other types of movement disorders is essential. The next step is to determine whether the dystonia is idiopathic, inherited, or acquired and identify an etiologic cause with selected investigations.
History
A history of abnormal muscle posture and movement, varying with different tasks, often worsening upon action of the same or a remote body part, is suggestive of dystonia. Pain in the affected muscles may be a prominent feature. Twisting of the dystonic body part frequently occurs if the limb, trunk, or neck is involved. Patients with dystonia are often able to temporarily suppress dystonic posturing or movements by touching the involved region or an adjacent body part. The sensory trick ("geste antagoniste") becomes less effective the more severe the dystonia.[Figure caption and citation for the preceding image starts]: Rotational torticollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends]. [Figure caption and citation for the preceding image starts]: The torticollis improves with a sensory trick: gently touching his chinFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: The torticollis improves with a sensory trick: gently touching his chinFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
The dystonia may be focal (a single body part or region), multifocal (multiple nonadjacent regions), segmental (multiple adjacent regions), hemidystonia (multiple ipsilateral body parts, e.g., arm and leg), or generalized (one or both legs, the trunk, and at least one other body part). Focal dystonia may spread to adjacent body parts, becoming segmental or even generalizing over time. This is particularly true with childhood-onset dystonia. Focal dystonias may be:
Axial; blepharospasm; cervical (torticollis), usually a combination of rotational torticollis, anterocollis and/or laterocollis, and retrocollis[Figure caption and citation for the preceding image starts]: BlepharospasmFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
 [Figure caption and citation for the preceding image starts]: Rotational torticollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Rotational torticollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends]. [Figure caption and citation for the preceding image starts]: Cervical dystonia: anterolateralcollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Cervical dystonia: anterolateralcollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends]. [Figure caption and citation for the preceding image starts]: Cervical dystonia: retrocollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Cervical dystonia: retrocollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
Limb dystonia that can be task-related (e.g., writer's cramp); foot dystonia; orofacial dystonia; and oromandibular dystonia.[Figure caption and citation for the preceding image starts]: Writer's cramp: a focal taskFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
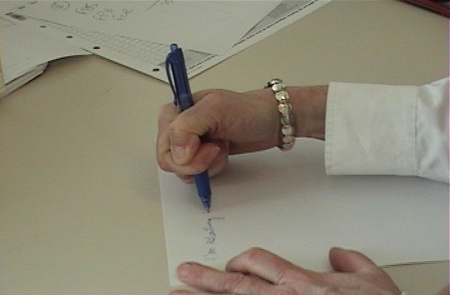 [Figure caption and citation for the preceding image starts]: Writer's cramp: a focal taskFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Writer's cramp: a focal taskFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends]. [Figure caption and citation for the preceding image starts]: Foot dystonia with involuntary plantar flexion and foot inversionFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Foot dystonia with involuntary plantar flexion and foot inversionFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
Other hyperkinetic movement disorders such as chorea, tremor, tics, and myoclonus should be distinguished, although these disorders can occur in association with dystonia. Dystonia is distinguishable from chorea in that movements are often sustained in postures rather than constantly moving. Myoclonus consists of a much briefer jerking movement, while tremor is a rhythmic oscillation of a body part.
In children, idiopathic dystonia often begins in a limb while in adults, idiopathic dystonia manifests almost exclusively in the head and neck region. A pattern of presentation deviating from this general rule may suggest the presence of an acquired dystonia.[35]
A thorough drug history is necessary to exclude the possibility of a dystonia induced by an antipsychotic or antiemetic drug. Associated medications include both typical and atypical antipsychotic agents and dopamine-receptor blocker antiemetics such as metoclopramide and prochlorperazine. These dystonias can either be acute dystonic reactions or a form of late-onset (tardive) dystonia.
Acute dystonic reactions, most commonly (but not exclusively) in younger male patients, may include torticollis, tongue or jaw dystonia, oculogyric crisis, or opisthotonus.[30][31][32] Patients presenting with an acute dystonic reaction typically provide history of current antipsychotics or antiemetic use; typically dystonias are self-limiting and stop within hours after medication discontinuation. In tardive dystonia, history of concurrent or recent neuroleptic exposure is necessary for diagnosis; dystonia may initially present upon the first discontinuation of the agent.
Presence of dementia, seizures, spasticity, pyramidal weakness, and development delay raises the suspicion of an acquired dystonia, either a heredodegenerative dystonia or related to perinatal or birth injury.
Presence of parkinsonism may indicate Parkinson disease (PD)-related dystonia or dystonia that occurs in several of the atypical parkinsonian syndromes.
A positive family history of dystonia is a significant risk factor, particularly for early-onset cases, and may signify an underlying genetic cause.[13]
There may be, in what appears to be a focal dystonia of a body part, a history of traumatic injury days or weeks earlier, although the precise etiologic relationship between trauma and dystonia remains controversial.[19][20][21]
An occupational history should also be taken as people who frequently use fine motor skills (e.g., musicians), are at increased risk of developing focal dystonia.
Physical examination
Observation
Observing positions of trunk, neck, head, and limbs at rest and observing spontaneous movements are critical to making the diagnosis. Noting areas of hypertrophy and asymmetry are key aspects of the neurologic examination.
Palpating muscles may reveal more hypertrophy than simple observation.
Watching patients walk may elicit some dystonia or subtle features of an underlying neurologic process.
Examining skin and nails may give a clue to the extent of dystonia. For example, toe flexion dystonia, often seen in Parkinson disease, may cause calluses at the tips of the toes or thickened toenails.
Eliciting dystonia
Simultaneous contraction of agonist and antagonist muscles is a hallmark of dystonia, but may be better appreciated by electromyography than by clinical examination.
Action dystonia is a near-universal feature, and may be present only with specific tasks involving the dystonic body part or with activation of remote body parts. For example, certain dystonias can be triggered by playing a musical instrument or by writing. When more advanced, dystonia may appear at rest.
Specific examination techniques of the affected region should be undertaken, as the dystonia may become more evident with certain tasks.
Blepharospasm: forced eye closure, reading of text, bright light, watching television.[Figure caption and citation for the preceding image starts]: BlepharospasmFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].

Spasmodic dysphonia: reading a passage, making a sustained "eee" sound, and counting out loud.
Orofacial and oromandibular dystonia: tongue protrusion, opening and closing the mouth repeatedly.
Cervical dystonia: examine patient seated with eyes closed allowing head to move on its own, rotating head to extreme left and right, full flexion, and extension of the neck.[Figure caption and citation for the preceding image starts]: Cervical dystonia: retrocollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
 [Figure caption and citation for the preceding image starts]: Cervical dystonia: anterolateralcollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Cervical dystonia: anterolateralcollisFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
Limb dystonia: arms extended supinated and pronated, finger to nose maneuver, finger tapping, handwriting, foot tapping, walking forward and backward; if appropriate, performing tasks related to the trigger of dystonia such as playing a musical instrument.[Figure caption and citation for the preceding image starts]: Writer's cramp: a focal taskFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
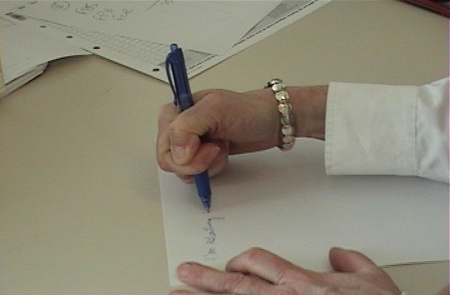 [Figure caption and citation for the preceding image starts]: Writer's cramp: a focal taskFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Writer's cramp: a focal taskFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends]. [Figure caption and citation for the preceding image starts]: Foot dystonia with involuntary plantar flexion and foot inversionFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
[Figure caption and citation for the preceding image starts]: Foot dystonia with involuntary plantar flexion and foot inversionFrom the personal teaching collections of David K. Simon, MD, Daniel Tarsy, MD, and Ludy C. Shih, MD; used with permissions [Citation ends].
Signs of a cause of acquired dystonia
Presence of other neurologic signs should be carefully sought. Accompanying parkinsonism suggests the possibility of PD-related dystonia. This usually manifests as foot dystonia, blepharospasm, or cervical dystonia, and rarely as a lateral axial dystonia.[36]
Dystonia can also occur in several of the atypical parkinsonism syndromes, such as multiple system atrophy (cranial, cervical, or axial dystonia), corticobasal degeneration (limb dystonia), or progressive supranuclear palsy (axial, limb, or hemidystonia).
Presence of myoclonus may indicate a distinct genetic entity called myoclonus-dystonia syndrome.
Posttraumatic dystonia is usually accompanied by other neurologic signs including tremor, weakness, and spasticity if head trauma is the cause. A relatively rapid-onset fixed dystonia accompanied by signs of complex regional pain syndrome is thought to comprise another form of posttraumatic dystonia, usually a focal limb dystonia.[18]
Ophthalmic examination may demonstrate the presence of Kayser-Fleischer rings in Wilson disease.
Investigations
Laboratory testing is not usually necessary for typical adult-onset idiopathic focal dystonia. Genetic testing for the TOR1A (also known as DYT1) mutations is appropriate when a focal or generalized dystonia is present in a person younger than 26 years of age or in someone older with a family history of early-onset dystonia. When available, referral to a genetic diagnostic testing service for testing of the other familial dystonias is advisable when features of a genetically identified dystonia syndrome are present (early onset, positive family history).
Investigations may also be indicated when Wilson disease is suspected (serum ceruloplasmin, urinary copper analysis), although tremor is a more common movement disorder manifestation in this disease.[37]
In early-onset dystonia (<40 years), a trial dose of levodopa can be offered.[37] It needs to be given for 4 weeks to assess responsiveness.[38] In addition, GCH1 genetic testing can be considered in some cases to confirm the presence of some causes of dopa-responsive dystonia.[16][17]
If an acquired dystonia is suspected, magnetic resonance imaging (MRI) of the brain is recommended.[39] It may be abnormal in the case of Wilson disease, heredodegenerative diseases causing dystonia, and cerebral infarction causing hemidystonia. Conventional T1- and T2-weighted MRI do not show any significant abnormalities in primary dystonia.
Several diagnostic algorithms have been proposed to ensure the proper evaluation for dystonia in childhood and adolescence.[40][41] The first step is to rule out mimics of dystonia in childhood and adolescence; the second, to rule out medication-induced dystonia; the third, to evaluate the likelihood of the presence of an acquired dystonia; and finally, biochemical and metabolic investigations are recommended before consideration of next-generation sequencing.
Use of this content is subject to our disclaimer