Osteoporotic spinal compression fractures
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
anterior column involvement only
limited bed rest
Almost all osteoporotic spinal compression fractures are of this type. Spinal stability is not compromised with these fractures.
Most patients experience gradual improvement of pain over 6-12 weeks and are managed with analgesia and 24-48 hours of bed rest, followed by early mobilisation with continued analgesia and temporary use of a thoracolumbar extension orthosis, if required.
Prolonged immobility should be avoided, as this only increases bone loss, frailty, and the risk of subsequent fractures.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com See Osteoporosis.
analgesia
Treatment recommended for ALL patients in selected patient group
Analgesia is prescribed to reduce pain and encourage mobilisation.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com
Analgesia should begin with non-opioids such as paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs). Data from animal studies on the impairment of fracture healing by NSAIDs are inconclusive, and these agents are regularly used clinically for this indication.[67]Borgeat A, Ofner C, Saporito A, et al. The effect of nonsteroidal anti-inflammatory drugs on bone healing in humans: a qualitative, systematic review. J Clin Anesth. 2018 Jun 15;49:92-100. http://www.ncbi.nlm.nih.gov/pubmed/29913395?tool=bestpractice.com [68]Marquez-Lara A, Hutchinson ID, Nuñez F Jr, et al. Nonsteroidal anti-inflammatory drugs and bone-healing: a systematic review of research quality. JBJS Rev. 2016 Mar 15;4(3):01874474-201603000-00005. https://journals.lww.com/jbjsreviews/fulltext/2016/03000/Nonsteroidal_Anti_Inflammatory_Drugs_and.4.aspx http://www.ncbi.nlm.nih.gov/pubmed/27500434?tool=bestpractice.com NSAIDs should be used with caution in older people because of increased susceptibility to side effects such as gastrointestinal bleeding and cardiovascular events.[69]McCarberg BH. NSAIDs in the older patient: balancing benefits and harms. Pain Med. 2013 Dec;14 Suppl 1:S43-4. https://academic.oup.com/painmedicine/article/14/suppl_1/S43/1941495 http://www.ncbi.nlm.nih.gov/pubmed/24373111?tool=bestpractice.com [70]Davis A, Robson J. The dangers of NSAIDs: look both ways. Br J Gen Pract. 2016 Apr;66(645):172-3. https://bjgp.org/content/66/645/172 http://www.ncbi.nlm.nih.gov/pubmed/27033477?tool=bestpractice.com UK guidelines recommend to consider paracetemol ahead of oral NSAIDs, cyclo-oxygenase-2 (COX-2) inhibitors, or opioids.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf
If stronger analgesia is required, opioids such as oxycodone can be used in combination with paracetamol. If opioids are used, a laxative should also be prescribed and fluid intake encouraged to prevent constipation, as straining at defecation can cause further fractures. If used chronically, opioids lose potency, induce dependence, raise risk for addiction, and lead to falls and central sensitisation.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com Opioids are recommended only for very short-term use with acute fractures.
For persistent severe pain, use of centrally-acting therapies including tricyclic antidepressants and gabapentin should be considered after discussion about the potential risks and benefits.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf
Primary options
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
and
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
OR
diclofenac potassium: 50 mg orally (immediate-release) two to three times daily when required
and
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
oxycodone: 5 mg orally (immediate-release) every 6 hours when required
and
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Tertiary options
amitriptyline: 25-150 mg/day orally given in 1-2 divided doses
OR
gabapentin: 300-1200 mg orally three times daily
early mobilisation ± orthosis
Treatment recommended for ALL patients in selected patient group
After an initial short period of bed rest, mobilisation should be encouraged. Recommendations from guidelines vary with regard to bracing. The Bone Health and Osteoporosis Foundation states bracing can be used but there is no evidence that bracing improves physical function or disability.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com UK guidelines recommend against routine use of bracing (e.g., rigid, dynamic, or soft orthoses) for patients with osteoporotic vertebral fractures and advise that bracing should be avoided in chronic stages post-fracture.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf However, these guidelines also note that some clinicians believe that the use of a soft brace intermittently in the acute stage may reduce fear or give the patient confidence to mobilise or resume activities.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf An orthosis may be used temporarily as an aid to control pain, promote fracture consolidation, support posture, improve balance, physical function and quality of life. Patients who are deemed suitable for orthoses are typically instructed to wear orthoses for up to 24 weeks until resolution of pain. Randomised controlled trial data are currently lacking to make evidence-based recommendations.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com Orthoses should be discarded when no longer required, as prolonged use will encourage further bone loss. Walking aids will help compensate for loss of sagittal balance and impaired proprioception and reduce fall risk.
long-term osteoporosis prophylaxis
Treatment recommended for ALL patients in selected patient group
The occurrence of a spinal compression fracture should trigger a review and optimisation of treatment of the underlying osteoporosis.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com
Supplementing the diet with calcium and vitamin D, reducing alcohol consumption, and stopping smoking are advised to minimise loss of bone mass and maintain skeletal trabeculae microarchitecture and cortical thickness.[94]Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/ American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis: 2020 update. Endor Pract. 2020 May;26(suppl 1):1-46. https://www.endocrinepractice.org/article/S1530-891X(20)42827-7/fulltext http://www.ncbi.nlm.nih.gov/pubmed/32427503?tool=bestpractice.com
Medications such as bisphosphonates significantly reduce the incidence of new vertebral fractures by almost 50%.[43]Lippuner K. Medical treatment of vertebral osteoporosis. Eur Spine J. 2003 Oct;12 Suppl 2:S132-41. http://www.ncbi.nlm.nih.gov/pubmed/13680313?tool=bestpractice.com Other medications of benefit include denosumab, romosozumab, parathyroid hormone analogues (e.g., teriparatide, abaloparatide), and raloxifene.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87. http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com [94]Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/ American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis: 2020 update. Endor Pract. 2020 May;26(suppl 1):1-46. https://www.endocrinepractice.org/article/S1530-891X(20)42827-7/fulltext http://www.ncbi.nlm.nih.gov/pubmed/32427503?tool=bestpractice.com [95]Management of osteoporosis in postmenopausal women: The 2021 position statement of The North American Menopause Society’’ editorial panel. Management of osteoporosis in postmenopausal women: the 2021 position statement of The North American Menopause Society. Menopause. 2021 Sep 1;28(9):973-97. https://journals.lww.com/menopausejournal/Fulltext/2021/09000/Management_of_osteoporosis_in_postmenopausal.3.aspx http://www.ncbi.nlm.nih.gov/pubmed/34448749?tool=bestpractice.com
Oral bisphosphonates (e.g., alendronic acid, ibandronic acid, and risedronate) are recommended by the National Institute for Health and Care Excellence (NICE) for the treatment of osteoporosis.[42]National Institute for Health and Care Excellence. Bisphosphonates for treating osteoporosis. April 2019 [internet publication]. https://www.nice.org.uk/guidance/ta464 NICE recommends raloxifene and teriparatide as alternative treatment options for secondary prevention of osteoporotic fragility fractures in postmenopausal women who are unable to adhere to the special instructions for the administration of alendronic acid and risedronate, or who have a contraindication to or are intolerant of alendronic acid and risedronate and who also have a combination of T-score, age, and number of independent clinical risk factors for fracture.[96]National Institute for Health and Care Excellence. Raloxifene and teriparatide for the secondary prevention of osteoporotic fragility fractures in postmenopausal women. Feb 2018 [internet publication]. https://www.nice.org.uk/guidance/ta161 NICE recommends romosozumab as an option for treating severe osteoporosis in people after menopause who are at high risk of fracture, only if: they have had a major osteoporotic fracture (spine, hip, forearm, or humerus fracture) within 24 months (so are at imminent risk of another fracture).[97]National Institute for Health and Care Excellence. Romosozumab for treating severe osteoporosis - technology appraisal guidance [TA791]. May 2022 [internet publication]. https://www.nice.org.uk/guidance/TA791/chapter/1-Recommendations
The European Medicines Agency no longer recommends calcitonin for the treatment of osteoporosis due to an increased risk of various types of cancer in patients using the drug long-term.[46]European Medicines Agency. European Medicines Agency recommends limiting long-term use of calcitonin medicines. Jul 2012 [internet publication]. https://www.ema.europa.eu/en/news/european-medicines-agency-recommends-limiting-long-term-use-calcitonin-medicines [47]Overman RA, Borse M, Gourlay ML. Salmon calcitonin use and associated cancer risk. Ann Pharmacother. 2013 Dec;47(12):1675-84. http://www.ncbi.nlm.nih.gov/pubmed/24259626?tool=bestpractice.com Calcitonin is still approved in the US but is infrequently used and is considered second-line therapy reserved for women in whom alternative treatments are not suitable.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com
specialist pain centre referral
Additional treatment recommended for SOME patients in selected patient group
Some patients with chronic pain may benefit from referral to a multi-disciplinary pain centre.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf Such centres combine cognitive-behavioural therapy, patient education, supervised exercise, transcutaneous electrical nerve stimulation, acupuncture, specialist walking aids, and other strategies to try to restore normal function. See Chronic pain syndromes.
vertebroplasty/kyphoplasty or open surgical stabilisation
Additional treatment recommended for SOME patients in selected patient group
Vertebroplasty and kyphoplasty offer a minimally invasive approach for patients with severe (chronic) pain despite optimal medical and conservative measures.
[  ]
In people with osteoporotic vertebral compression fracture, how does percutaneous vertebroplasty compare with placebo?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2376/fullShow me the answer Vertebroplasty and kyphoplasty are relatively recent techniques that offer a minimally invasive approach to this group of patients.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87.
http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com
Balloon kyphoplasty and percutaneous vertebroplasty have both been found to be safe and effective surgical procedures for treating osteoporotic vertebral compression fractures in multiple studies with improvements in pain relief and respiratory function.[71]Ma XL, Xing D, Ma JX, et al. Balloon kyphoplasty versus percutaneous vertebroplasty in treating osteoporotic vertebral compression fracture: grading the evidence through a systematic review and meta-analysis. Eur Spine J. 2012 Sep;21(9):1844-59.
http://www.ncbi.nlm.nih.gov/pubmed/22832872?tool=bestpractice.com
[72]Kanayama M, Oha F, Iwata A, et al. Does balloon kyphoplasty improve the global spinal alignment in osteoporotic vertebral fracture? Int Orthop. 2015 Jun;39(6):1137-43.
http://www.ncbi.nlm.nih.gov/pubmed/25787683?tool=bestpractice.com
[73]Yokoyama K, Kawanishi M, Yamada M, et al. In not only vertebroplasty but also kyphoplasty, the resolution of vertebral deformities depends on vertebral mobility. AJNR Am J Neuroradiol. 2013 Jul;34(7):1474-8.
https://www.ajnr.org/content/34/7/1474
http://www.ncbi.nlm.nih.gov/pubmed/23391839?tool=bestpractice.com
[74]Yokoyama K, Kawanishi M, Yamada M, et al. Postoperative change in sagittal balance after Kyphoplasty for the treatment of osteoporotic vertebral compression fracture. Eur Spine J. 2015 Apr;24(4):744-9.
http://www.ncbi.nlm.nih.gov/pubmed/25404372?tool=bestpractice.com
[75]Tanigawa N, Kariya S, Komemushi A, et al. Added value of percutaneous vertebroplasty: effects on respiratory function. AJR Am J Roentgenol. 2012 Jan;198(1):W51-4.
https://www.ajronline.org/doi/10.2214/AJR.11.6730
http://www.ncbi.nlm.nih.gov/pubmed/22194515?tool=bestpractice.com
Serious complications reported with these procedures include cement pulmonary embolism, osteomyelitis, and epidural cement leak.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102.
https://link.springer.com/article/10.1007/s00198-021-05900-y
http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com
]
In people with osteoporotic vertebral compression fracture, how does percutaneous vertebroplasty compare with placebo?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2376/fullShow me the answer Vertebroplasty and kyphoplasty are relatively recent techniques that offer a minimally invasive approach to this group of patients.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87.
http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com
Balloon kyphoplasty and percutaneous vertebroplasty have both been found to be safe and effective surgical procedures for treating osteoporotic vertebral compression fractures in multiple studies with improvements in pain relief and respiratory function.[71]Ma XL, Xing D, Ma JX, et al. Balloon kyphoplasty versus percutaneous vertebroplasty in treating osteoporotic vertebral compression fracture: grading the evidence through a systematic review and meta-analysis. Eur Spine J. 2012 Sep;21(9):1844-59.
http://www.ncbi.nlm.nih.gov/pubmed/22832872?tool=bestpractice.com
[72]Kanayama M, Oha F, Iwata A, et al. Does balloon kyphoplasty improve the global spinal alignment in osteoporotic vertebral fracture? Int Orthop. 2015 Jun;39(6):1137-43.
http://www.ncbi.nlm.nih.gov/pubmed/25787683?tool=bestpractice.com
[73]Yokoyama K, Kawanishi M, Yamada M, et al. In not only vertebroplasty but also kyphoplasty, the resolution of vertebral deformities depends on vertebral mobility. AJNR Am J Neuroradiol. 2013 Jul;34(7):1474-8.
https://www.ajnr.org/content/34/7/1474
http://www.ncbi.nlm.nih.gov/pubmed/23391839?tool=bestpractice.com
[74]Yokoyama K, Kawanishi M, Yamada M, et al. Postoperative change in sagittal balance after Kyphoplasty for the treatment of osteoporotic vertebral compression fracture. Eur Spine J. 2015 Apr;24(4):744-9.
http://www.ncbi.nlm.nih.gov/pubmed/25404372?tool=bestpractice.com
[75]Tanigawa N, Kariya S, Komemushi A, et al. Added value of percutaneous vertebroplasty: effects on respiratory function. AJR Am J Roentgenol. 2012 Jan;198(1):W51-4.
https://www.ajronline.org/doi/10.2214/AJR.11.6730
http://www.ncbi.nlm.nih.gov/pubmed/22194515?tool=bestpractice.com
Serious complications reported with these procedures include cement pulmonary embolism, osteomyelitis, and epidural cement leak.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102.
https://link.springer.com/article/10.1007/s00198-021-05900-y
http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com
UK guidelines from the Royal Osteoporosis Society, published in 2022, recommend to consider referral for vertebroplasty or kyphoplasty for hospitalised patients in whom pain is unremitting after 48 hours and severely compromising activities of daily living and mobility in spite of initiation of therapy and acute pain management, and where there is evidence of vertebral body oedema on MRI imaging.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf
The American College of Radiology (ACR) recommends in its 2022 guidance to consider percutaneous vertebroplasty or percutaneous balloon kyphoplasty for pain relief and increased mobility.[9]American College of Radiology. ACR Appropriateness Criteria: management of vertebral compression fractures. 2022 [internet publication]. https://acsearch.acr.org/docs/70545/Narrative This recommendation is based on a 2014 US multi-society task force of spine interventionalists reporting that percutaneous vertebroplasty and percutaneous balloon kyphoplasty could be considered generally interchangeable techniques for these indications.[9]American College of Radiology. ACR Appropriateness Criteria: management of vertebral compression fractures. 2022 [internet publication]. https://acsearch.acr.org/docs/70545/Narrative [76]Barr JD, Jensen ME, Hirsch JA, et al. Position statement on percutaneous vertebral augmentation: a consensus statement developed by the Society of Interventional Radiology (SIR), American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS), American College of Radiology (ACR), American Society of Neuroradiology (ASNR), American Society of Spine Radiology (ASSR), Canadian Interventional Radiology Association (CIRA), and the Society of NeuroInterventional Surgery (SNIS). J Vasc Interv Radiol. 2014 Feb;25(2):171-81. https://www.jvir.org/article/S1051-0443(13)01487-5/fulltext http://www.ncbi.nlm.nih.gov/pubmed/24325929?tool=bestpractice.com Balloon kyphoplasty and percutaneous vertebroplasty are recommended by the ACR for instances of failed non-operative medical therapy.[9]American College of Radiology. ACR Appropriateness Criteria: management of vertebral compression fractures. 2022 [internet publication]. https://acsearch.acr.org/docs/70545/Narrative The multi-society panel stated in 2014 that additional factors could inform the choice of technique, such as the degree of compression deformity, the age of fracture, and the presence of neoplastic involvement.[76]Barr JD, Jensen ME, Hirsch JA, et al. Position statement on percutaneous vertebral augmentation: a consensus statement developed by the Society of Interventional Radiology (SIR), American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS), American College of Radiology (ACR), American Society of Neuroradiology (ASNR), American Society of Spine Radiology (ASSR), Canadian Interventional Radiology Association (CIRA), and the Society of NeuroInterventional Surgery (SNIS). J Vasc Interv Radiol. 2014 Feb;25(2):171-81. https://www.jvir.org/article/S1051-0443(13)01487-5/fulltext http://www.ncbi.nlm.nih.gov/pubmed/24325929?tool=bestpractice.com However, the same task force reconvened in 2019, concluding that routine use of vertebral augmentation is not supported by current evidence. For patients with acutely painful vertebral fractures, the data reviewed by the panel in 2019 demonstrated that percutaneous vertebroplasty provides no demonstrable clinically significant benefit over placebo. There was insufficient evidence to recommend kyphoplasty over non-surgical management.[77]Ebeling PR, Akesson K, Bauer DC, et al. The efficacy and safety of vertebral augmentation: a second ASBMR task force report. J Bone Miner Res. 2019 Jan;34(1):3-21. https://asbmr.onlinelibrary.wiley.com/doi/10.1002/jbmr.3653 http://www.ncbi.nlm.nih.gov/pubmed/30677181?tool=bestpractice.com These latest findings are not yet reflected in the ACR guidance.
In the outpatient setting, the National Institute for Health and Care Excellence (NICE) in the UK recommends in its 2013 guideline that percutaneous vertebroplasty and percutaneous balloon kyphoplasty (without stenting) are both options for treating osteoporotic vertebral compression fractures in patients who have severe ongoing pain after a recent, unhealed vertebral fracture despite optimal pain management, and in patients in whom the pain has been confirmed to be at the level of the fracture by physical examination and imaging.[78]National Institute for Health and Care Excellence. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoporotic vertebral compression fractures. Apr 2013 [internet publication]. https://www.nice.org.uk/guidance/TA279
Vertebroplasty involves the injection of bone cement into the vertebral body under fluoroscopic guidance and can be performed as a 1-day or overnight procedure. The mechanism of pain relief is mainly from fracture stabilisation, although thermal and chemical ablation of the nerve endings in the vertebral body may also contribute.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87. http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com
Individual studies and one meta-analysis suggest that a specific population may benefit from vertebral augmentation: older inpatients (mean age >80 years), with comorbidity (≥2 comorbid conditions), high pain scores on a visual analogue scale (>7), and whose fractures are difficult to manage with non-surgical treatments.[83]Rousing R, Andersen MO, Jespersen SM, et al. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine (Phila Pa 1976). 2009 Jun 1;34(13):1349-54. http://www.ncbi.nlm.nih.gov/pubmed/19478654?tool=bestpractice.com [84]Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016 Aug 17;388(10052):1408-16. http://www.ncbi.nlm.nih.gov/pubmed/27544377?tool=bestpractice.com [85]Ong T, Kantachuvesiri P, Sahota O, et al. Characteristics and outcomes of hospitalised patients with vertebral fragility fractures: a systematic review. Age Ageing. 2018 Jan 1;47(1):17-25. https://academic.oup.com/ageing/article/47/1/17/3811072 http://www.ncbi.nlm.nih.gov/pubmed/29253103?tool=bestpractice.com
With kyphoplasty, an inflatable bone tamp is first inserted percutaneously into the collapsed vertebral body under fluoroscopic guidance. The endplates are then elevated as the tamp is inflated. The fracture is then fixed by the injection of bone cement in a manner similar to vertebroplasty.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87. http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com Both procedures seem to be equally effective, but kyphoplasty seems to be safer than vertebroplasty.[86]Felder-Puig R, Piso B, Guba B, et al. Kyphoplasty and vertebroplasty for the management of osteoporotic vertebral compression fractures: a systematic review [in German]. Orthopade. 2009 Jul;38(7):606-15. http://www.ncbi.nlm.nih.gov/pubmed/19517091?tool=bestpractice.com Generally, indisputable evidence in favour of or against the effectiveness of cement injection is still lacking.[91]Muijs SP, van Erkel AR, Dijkstra PD. Treatment of painful osteoporotic vertebral compression fractures: a brief review of the evidence for percutaneous vertebroplasty. J Bone Joint Surg Br. 2011 Sep;93(9):1149-53. http://www.ncbi.nlm.nih.gov/pubmed/21911522?tool=bestpractice.com
The optimal timing of surgical intervention remains unclear. Percutaneous vertebral augmentation guidelines suggest that, ideally, patients should present within 4 months of the fracture (as measured by the onset of pain) and have at least 3 weeks of failure of conservative treatment before undergoing vertebroplasty.[90]Tsoumakidou G, Too CW, Koch G, et al. CIRSE guidelines on percutaneous vertebral augmentation. Cardiovasc Intervent Radiol. 2017 Jan 19;40(3):331-42. http://www.ncbi.nlm.nih.gov/pubmed/28105496?tool=bestpractice.com Intervention may, however, be considered within days of a painful fracture in patients at high risk for bed-rest complications including thrombophlebitis, deep vein thrombosis, pneumonia, and pressure ulcer.[90]Tsoumakidou G, Too CW, Koch G, et al. CIRSE guidelines on percutaneous vertebral augmentation. Cardiovasc Intervent Radiol. 2017 Jan 19;40(3):331-42. http://www.ncbi.nlm.nih.gov/pubmed/28105496?tool=bestpractice.com
Open surgical treatment of the osteoporotic spine is challenging and tends to be reserved for those cases where less-invasive approaches have not provided a satisfactory result.
open surgical reconstruction ± vertebroplasty/kyphoplasty
Additional treatment recommended for SOME patients in selected patient group
Significant deformity is an indication for open surgical reconstruction, with or without vertebroplasty or kyphoplasty at the time of open surgery.
It is often difficult to achieve reliable fixation, and bone grafts frequently subside into the weak osteoporotic bone.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87. http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com Careful patient selection is critical to achieving satisfactory results. Pre-operative health status must be carefully considered when deciding whether open surgery is a viable option.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87. http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com
Anterior, posterior, or combined anterior and posterior approaches can be used, depending on the exact configuration of the fracture(s). The aim is to eliminate motion by enabling the fractured vertebra to fuse to the adjacent vertebrae by using a combination of bone graft, screws, and plates. Extension osteotomy of the spine may be considered to compensate for loss of sagittal balance but is associated with high complication rates. [Figure caption and citation for the preceding image starts]: Pre-operative sagittal T2-weighted magnetic resonance imaging showing osteoporotic spinal compression fractures of L1,2,4Personal collection of Nasir A. Quraishi [Citation ends].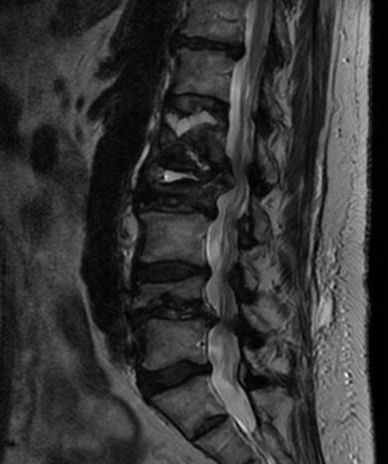 [Figure caption and citation for the preceding image starts]: Anteroposterior and lateral x-ray images of patient with osteoporotic spinal compression fractures of L1,2,4 following kyphoplastyPersonal collection of Nasir A. Quraishi [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior and lateral x-ray images of patient with osteoporotic spinal compression fractures of L1,2,4 following kyphoplastyPersonal collection of Nasir A. Quraishi [Citation ends].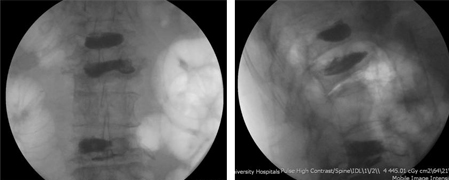
multiple column involvement
strict bed rest
Rarely, osteoporotic compression fractures can involve the middle and/or posterior spinal columns in addition to the anterior column. These types of fractures are potentially unstable.
Patients are placed on strict bed rest and given analgesia while definitive treatment is planned.
analgesia
Treatment recommended for ALL patients in selected patient group
Analgesia should begin with non-opioids such as paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs). Data from animal studies on the impairment of fracture healing by NSAIDs are inconclusive, and these agents are regularly used clinically for this indication.[67]Borgeat A, Ofner C, Saporito A, et al. The effect of nonsteroidal anti-inflammatory drugs on bone healing in humans: a qualitative, systematic review. J Clin Anesth. 2018 Jun 15;49:92-100. http://www.ncbi.nlm.nih.gov/pubmed/29913395?tool=bestpractice.com [68]Marquez-Lara A, Hutchinson ID, Nuñez F Jr, et al. Nonsteroidal anti-inflammatory drugs and bone-healing: a systematic review of research quality. JBJS Rev. 2016 Mar 15;4(3):01874474-201603000-00005. https://journals.lww.com/jbjsreviews/fulltext/2016/03000/Nonsteroidal_Anti_Inflammatory_Drugs_and.4.aspx http://www.ncbi.nlm.nih.gov/pubmed/27500434?tool=bestpractice.com NSAIDs should be used with caution in older people because of increased susceptibility to side effects such as gastrointestinal bleeding and cardiovascular events.[69]McCarberg BH. NSAIDs in the older patient: balancing benefits and harms. Pain Med. 2013 Dec;14 Suppl 1:S43-4. https://academic.oup.com/painmedicine/article/14/suppl_1/S43/1941495 http://www.ncbi.nlm.nih.gov/pubmed/24373111?tool=bestpractice.com [70]Davis A, Robson J. The dangers of NSAIDs: look both ways. Br J Gen Pract. 2016 Apr;66(645):172-3. https://bjgp.org/content/66/645/172 http://www.ncbi.nlm.nih.gov/pubmed/27033477?tool=bestpractice.com UK guidelines recommend to consider paracetemol ahead of oral NSAIDs, cyclo-oxygenase-2 (COX-2) inhibitors, or opioids.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf
If stronger analgesia is required, opioids such as oxycodone can be used in combination with paracetamol. If opioids are used, a laxative should also be prescribed and fluid intake encouraged to prevent constipation, as straining at defecation can cause further fractures. If used chronically, opioids lose potency, induce dependence, raise risk for addiction, and lead to falls and central sensitisation.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com Opioids are recommended only for very short-term use with acute fractures. For persistent severe pain, use of centrally-acting therapies including tricyclic antidepressants and gabapentin should be considered after discussion about the potential risks and benefits.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf
Primary options
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
and
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
OR
diclofenac potassium: 50 mg orally (immediate-release) two to three times daily when required
and
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
oxycodone: 5 mg orally (immediate-release) every 6 hours when required
and
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Tertiary options
amitriptyline: 25-150 mg/day orally given in 1-2 divided doses
OR
gabapentin: 300-1200 mg orally three times daily
open surgical reconstruction ± decompression
Treatment recommended for ALL patients in selected patient group
Osteoporotic compression fractures involving ≥2 columns of the spine are potentially unstable and are prone to neurological involvement. These cases should be treated by open spinal reconstruction. Open decompression is required if there is neurological involvement, and is followed by augmentation and fixation of the spinal column.
Anterior, posterior, or combined anterior and posterior approaches can be used, depending on the exact configuration of the fracture(s). The aim is to eliminate movement of the fractured vertebra by enabling it to fuse to the adjacent vertebrae, by using a combination of bone graft, screws, and plates. Extension osteotomy of the spine may be considered to compensate for loss of sagittal balance, but is associated with high complication rates. [Figure caption and citation for the preceding image starts]: Pre-operative sagittal T2-weighted magnetic resonance imaging showing osteoporotic spinal compression fractures of L1,2,4Personal collection of Nasir A. Quraishi [Citation ends].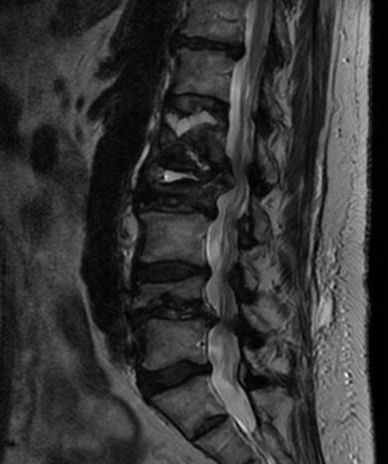 [Figure caption and citation for the preceding image starts]: Anteroposterior and lateral x-ray images of patient with osteoporotic spinal compression fractures of L1,2,4 following kyphoplastyPersonal collection of Nasir A. Quraishi [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior and lateral x-ray images of patient with osteoporotic spinal compression fractures of L1,2,4 following kyphoplastyPersonal collection of Nasir A. Quraishi [Citation ends].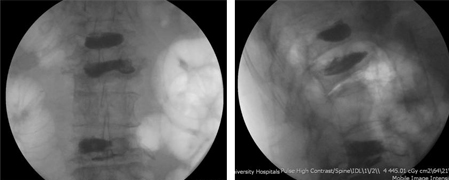
vertebroplasty/kyphoplasty
Additional treatment recommended for SOME patients in selected patient group
Some surgeons may perform kyphoplasty or vertebroplasty as an additional measure during the open surgical procedure.
long-term osteoporosis prophylaxis
Treatment recommended for ALL patients in selected patient group
The occurrence of a spinal compression fracture should trigger a review and optimisation of treatment of the underlying osteoporosis.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com
Supplementing the diet with calcium and vitamin D, reducing alcohol consumption, and stopping smoking are advised to minimise loss of bone mass and maintain skeletal trabeculae microarchitecture and cortical thickness.[94]Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/ American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis: 2020 update. Endor Pract. 2020 May;26(suppl 1):1-46. https://www.endocrinepractice.org/article/S1530-891X(20)42827-7/fulltext http://www.ncbi.nlm.nih.gov/pubmed/32427503?tool=bestpractice.com
Medications such as bisphosphonates significantly reduce the incidence of new vertebral fractures by almost 50%.[43]Lippuner K. Medical treatment of vertebral osteoporosis. Eur Spine J. 2003 Oct;12 Suppl 2:S132-41. http://www.ncbi.nlm.nih.gov/pubmed/13680313?tool=bestpractice.com Other medications of benefit include denosumab, romosozumab, parathyroid hormone analogues (e.g., teriparatide, abaloparatide), and raloxifene.[1]Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J. 2006 Sep-Oct;6(5):479-87. http://www.ncbi.nlm.nih.gov/pubmed/16934715?tool=bestpractice.com [18]North American Menopause Society. Management of osteoporosis in postmenopausal women: the 2021 position statement of The North American Menopause Society. Menopause. 2021 Sep 1;28(9):973-97. https://journals.lww.com/menopausejournal/Fulltext/2021/09000/Management_of_osteoporosis_in_postmenopausal.3.aspx http://www.ncbi.nlm.nih.gov/pubmed/34448749?tool=bestpractice.com [94]Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/ American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis: 2020 update. Endor Pract. 2020 May;26(suppl 1):1-46. https://www.endocrinepractice.org/article/S1530-891X(20)42827-7/fulltext http://www.ncbi.nlm.nih.gov/pubmed/32427503?tool=bestpractice.com
Oral bisphosphonates (e.g., alendronic acid, ibandronic acid, and risedronate) are recommended by the National Institute for Health and Care Excellence (NICE) for the treatment of osteoporosis.[42]National Institute for Health and Care Excellence. Bisphosphonates for treating osteoporosis. April 2019 [internet publication]. https://www.nice.org.uk/guidance/ta464 NICE recommends raloxifene and teriparatide as alternative treatment options for secondary prevention of osteoporotic fragility fractures in postmenopausal women who are unable to adhere to the special instructions for the administration of alendronic acid and risedronate, or who have a contraindication to or are intolerant of alendronic acid and risedronate and who also have a combination of T-score, age, and number of independent clinical risk factors for fracture.[96]National Institute for Health and Care Excellence. Raloxifene and teriparatide for the secondary prevention of osteoporotic fragility fractures in postmenopausal women. Feb 2018 [internet publication]. https://www.nice.org.uk/guidance/ta161 NICE recommends romosozumab as an option for treating severe osteoporosis in people after menopause who are at high risk of fracture, only if: they have had a major osteoporotic fracture (spine, hip, forearm, or humerus fracture) within 24 months (so are at imminent risk of another fracture).[97]National Institute for Health and Care Excellence. Romosozumab for treating severe osteoporosis - technology appraisal guidance [TA791]. May 2022 [internet publication]. https://www.nice.org.uk/guidance/TA791/chapter/1-Recommendations
The European Medicines Agency no longer recommends calcitonin for the treatment of osteoporosis due to an increased risk of various types of cancer in patients using the drug long-term.[46]European Medicines Agency. European Medicines Agency recommends limiting long-term use of calcitonin medicines. Jul 2012 [internet publication]. https://www.ema.europa.eu/en/news/european-medicines-agency-recommends-limiting-long-term-use-calcitonin-medicines [47]Overman RA, Borse M, Gourlay ML. Salmon calcitonin use and associated cancer risk. Ann Pharmacother. 2013 Dec;47(12):1675-84. http://www.ncbi.nlm.nih.gov/pubmed/24259626?tool=bestpractice.com Calcitonin is still approved in the US but is infrequently used and is considered second-line therapy reserved for women in whom alternative treatments are not suitable.[11]LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102. https://link.springer.com/article/10.1007/s00198-021-05900-y http://www.ncbi.nlm.nih.gov/pubmed/35478046?tool=bestpractice.com
specialist pain centre referral
Additional treatment recommended for SOME patients in selected patient group
Some patients with chronic pain may benefit from referral to a multidisciplinary pain centre.[57]Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication]. https://strwebprdmedia.blob.core.windows.net/media/kuphgv1u/ros-guidance-on-managing-symptoms-of-vertebral-fractures-2022.pdf Such centres combine cognitive-behavioural therapy, patient education, supervised exercise, transcutaneous electrical nerve stimulation, acupuncture, and other strategies to try to restore normal function. See Chronic pain syndromes.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer