Approach
The general aims of treatment of acute osteoporotic spinal compression fracture include:
Providing sufficient analgesia and physical support to facilitate rapid rehabilitation and return to normal activities
Reducing the risk of further fractures
Reducing progression of existing fractures.
Prolonged immobility should be avoided, as this only increases bone loss and the risk of subsequent fractures.
Vertebral fractures do not usually require hospitalisation.[11] In most patients, experts recommend non-operative interventions combined with radiographic and clinical follow-up at 6-week intervals for 3 months from injury are sufficient. However, surgical intervention may be required for potentially unstable acute fractures or if any of the following develop: worsening pain on mobilisation, significant deformity, or neurological involvement.
The occurrence of a spinal compression fracture should also trigger a review and optimisation of treatment of the underlying osteoporosis itself.[11] See Osteoporosis.
Acute isolated anterior column fracture
Almost all osteoporotic compression fractures are of this type. Most patients experience gradual improvement of pain over 6-12 weeks and are managed with analgesia and 24-48 hours of bed rest, followed by early mobilisation with continued analgesia and temporary use of a lumbosacral corset or thoracolumbar orthosis, if required. Prolonged immobility should be avoided, as this only increases bone loss, frailty, and the risk of subsequent fractures.[11]
Analgesia should begin with non-opioids such as paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs). Data from animal studies on the impairment of fracture healing by NSAIDs are inconclusive, and these agents are regularly used clinically for this indication.[67][68] NSAIDs should be used with caution in older people because of increased susceptibility to side effects such as gastrointestinal bleeding and cardiovascular events.[69][70] UK guidelines recommend to consider paracetamol ahead of oral NSAIDs, cyclo-oxygenase-2 (COX-2) inhibitors, or opioids.[57] If stronger analgesia is required, opioids such as oxycodone can be used in combination with paracetamol. If opioids are used, a laxative should also be prescribed and fluid intake encouraged to avoid constipation, as straining at defecation can cause further fractures. If used chronically, opioids lose potency, induce dependence, raise risk for addiction, and lead to falls and central sensitisation.[11] Opioids are recommended only for very short-term use with acute fractures. For persistent severe pain, use of centrally-acting therapies including tricyclic antidepressants and gabapentin should be considered after discussion about the potential risks and benefits.[57]
After the initial short period of bed rest, mobilisation should be encouraged.
Recommendations from guidelines vary with regard to bracing. The Bone Health and Osteoporosis Foundation states bracing can be used but there is no evidence that bracing improves physical function or disability.[11] UK guidelines recommend against routine use of bracing (e.g., rigid, dynamic, or soft orthoses) for patients with osteoporotic vertebral fractures and advise that bracing should be avoided in chronic stages post-fracture.[57] However, these guidelines also note that some clinicians believe that the use of a soft brace intermittently in the acute stage may reduces fear or gives the patient confidence to mobilise or resume activities.[57] An orthosis may be used temporarily as an aid to control pain, promote fracture consolidation, support posture and improve balance, physical function and quality of life.[11][57]
Patients who are deemed suitable for orthoses are typically instructed to wear them for up to 24 weeks until resolution of pain. Randomised controlled trial data are currently lacking to make evidence-based recommendations.[11] Orthoses should be discarded when no longer required, as prolonged use will encourage further bone loss. Walking aids will help compensate for loss of sagittal balance and impaired proprioception and reduce fall risk.
Some patients with chronic pain may benefit from referral to a multidisciplinary pain centre.[57] Such centres combine cognitive-behavioural therapy, patient education, supervised exercise, transcutaneous electrical nerve stimulation, acupuncture, and other strategies to restore function. See Chronic pain syndromes.
Increasing pain or deformity in people with anterior column fracture
Patients who develop severe (chronic) pain or significant deformity (e.g., >30° of kyphosis) despite optimal medical and conservative management can be considered for operative intervention.[1] The main surgical options in these cases are vertebroplasty, kyphoplasty, or open spinal fusion.
[  ]
]
Vertebroplasty and kyphoplasty are relatively recent techniques that offer a minimally invasive approach to this group of patients.[1] Balloon kyphoplasty and percutaneous vertebroplasty have both been found to be safe and effective surgical procedures for treating osteoporotic vertebral compression fractures in multiple studies with improvements in pain relief and respiratory function.[71][72][73][74][75] Serious complications reported with these procedures include cement pulmonary embolism, osteomyelitis, and epidural cement leak.[11]
UK guidelines from the Royal Osteoporosis Society, published in 2022, recommend to consider referral for vertebroplasty or kyphoplasty for hospitalised patients in whom pain is unremitting after 48 hours and severely compromising activities of daily living and mobility in spite of initiation of therapy and acute pain management, and where there is evidence of vertebral body oedema on MRI imaging.[9][57]
The American College of Radiology (ACR) recommends in its 2022 guidance to consider percutaneous vertebroplasty or percutaneous balloon kyphoplasty for pain relief and increased mobility.[9] This recommendation is based on a 2014 US multi-society task force of spine interventionalists reporting that percutaneous vertebroplasty and percutaneous balloon kyphoplasty could be considered generally interchangeable techniques for these indications.[9][76] Balloon kyphoplasty and percutaneous vertebroplasty are recommended by the ACR for instances of failed nonoperative medical therapy.[9] The multi-society panel stated in 2014 that additional factors could inform the choice of technique, such as the degree of compression deformity, the age of fracture, and the presence of neoplastic involvement.[76] However, the same task force reconvened in 2019, concluding that routine use of vertebral augmentation is not supported by current evidence. For patients with acutely painful vertebral fractures, the data reviewed by the panel in 2019 demonstrated that percutaneous vertebroplasty provides no demonstrable clinically significant benefit over placebo. There was insufficient evidence to recommend kyphoplasty over non-surgical management.[77] These latest findings are not yet reflected in the ACR guidance.
In the outpatient setting, National Institute for Health and Care Excellence (NICE) in the UK recommends in its 2013 guideline that percutaneous vertebroplasty and percutaneous balloon kyphoplasty (without stenting) are both options for treating osteoporotic vertebral compression fractures in patients who have severe ongoing pain after a recent, unhealed vertebral fracture despite optimal pain management, and in patients in whom the pain has been confirmed to be at the level of the fracture by physical examination and imaging.[78]
Vertebroplasty
Vertebroplasty involves the injection of bone cement into the vertebral body under fluoroscopic guidance and can be performed as a 1-day or overnight procedure. Reduction of the vertebral fracture is first attempted by carefully positioning the patient in the prone position on the operating table. Then, under fluoroscopic guidance, a needle is directed into the fractured vertebrae by a transpedicular or posterolateral extrapedicular approach. Between 2-8 mL of polymethylmethacrylate (PMMA) bone cement mixed with barium is then injected under direct visualisation into the body of the vertebra, with extreme care being taken to avoid extravasation of the cement into the spinal canal, neuroforamen, or central venous system (where it can cause potentially fatal pulmonary emboli). Pain relief results from stabilisation of the fracture, although thermal and chemical ablation of the nerve endings in the vertebral body may also contribute.[1]
Meta-analyses comparing percutaneous vertebroplasty with conservative therapy for the management of osteoporotic spinal fracture report significantly greater pain relief with vertebroplasty (up to 1 year postoperatively).[79][80] Percutaneous vertebroplasty was associated with greater functional recovery and health-related quality of life at early (<12 weeks) and late time points (6-12 months).[79] A subsequent Cochrane review found no clinically important benefits attributable to percutaneous vertebroplasty (with respect to pain or disability, compared with sham procedure).[81] However, this Cochrane review has been criticised for failing to accurately report the evidence for vertebroplasty in patients with severe symptoms and early fractures.[82] Individual studies[83][84] and one meta-analysis[85] suggest that a specific population may benefit from vertebral augmentation: older in-patients (mean age >80 years), with comorbidity (≥2 comorbid conditions), high pain scores on a visual analogue scale (>7), and whose fractures are difficult to manage with non-surgical treatments.
Kyphoplasty
Kyphoplasty is a similar technique to vertebroplasty, but involves an additional step in which an inflatable bone tamp is first inserted percutaneously into the collapsed vertebral body under fluoroscopic guidance. The tamp is then inflated, compressing the cancellous bone and elevating the endplates. The fracture is then fixed by the injection of bone cement in a similar manner to vertebroplasty.[1] Both procedures seem to be equally effective, but kyphoplasty seems to be safer than vertebroplasty.[86] Although the incidence of adverse events for these procedures is low, it seems that vertebroplasty is associated with a statistically significant increased rate of procedure-related complications and cement extravasation (symptomatic and asymptomatic).[87] Furthermore, prospective studies of low bias, with follow-up of ≥12 months, demonstrate that balloon kyphoplasty is at least as effective as vertebroplasty, and more effective than the medical management of osteoporotic vertebral compression fractures.[88] One randomised controlled trial comparing balloon kyphoplasty with non-operative care found that balloon kyphoplasty was an effective and safe procedure for patients with acute vertebral fractures.[89]
Optimal timing of surgical intervention remains unclear
Percutaneous vertebral augmentation guidelines suggest that, ideally, patients should present within 4 months of the fracture (as measured by the onset of pain) and have at least 3 weeks of failure of conservative treatment before undergoing vertebroplasty.[90] Intervention may, however, be considered within days of a painful fracture in patients at high risk for bed-rest complications including thrombophlebitis, deep vein thrombosis, pneumonia, and pressure ulcer.[90]
One small, randomised, double-blind trial found that percutaneous vertebroplasty significantly reduced pain compared with a placebo intervention (Numeric Rated Scale; between-group difference 23%, 95% CI 6 to 39; P=0.011) in patients presenting with acute painful osteoporotic fractures of less than 6 weeks' duration.[84]
Effectiveness of cement injection
Generally, indisputable evidence regarding the effectiveness of cement injection is still lacking.[91] In randomised controlled trials of patients with osteoporotic compression fractures, improvements in pain and pain-related disability with vertebroplasty may be similar to those in the placebo arm (e.g., simulated procedure [verbal/physical cues, pressure on the patient's back, opening of methacrylate monomer, but no needle placement or infusion]; or placement of a needle into the bone but without the injection of cement).[92][93] However, in one of the studies follow-up was limited to 3 months, there was a trend towards better pain scores in the vertebroplasty group, and crossover was higher in the control group.[92]
Open surgical management
Open surgical treatment of the osteoporotic spine is challenging and tends to be reserved for those cases where less-invasive approaches have not provided a satisfactory result in terms of relief of chronic pain. Open surgery is the initial surgical procedure for people with severe deformity, with or without vertebroplasty or kyphoplasty at the time of open surgery. It is often difficult to achieve reliable fixation, and bone grafts frequently subside into the weak osteoporotic bone.[1] Careful patient selection is critical to achieving satisfactory results. Preoperative health status must be carefully considered when deciding whether open surgery is a viable option.[1] Anterior, posterior, or combined anterior and posterior approaches can be used, depending on the exact configuration of the fracture(s). The aim is to eliminate motion by enabling the fractured vertebra to fuse to the adjacent vertebrae by using a combination of bone graft, screws, and plates. Extension osteotomy of the spine may be considered to compensate for loss of sagittal balance, but is associated with high complication rates.[Figure caption and citation for the preceding image starts]: Pre-operative sagittal T2-weighted magnetic resonance imaging showing osteoporotic spinal compression fractures of L1,2,4Personal collection of Nasir A. Quraishi [Citation ends].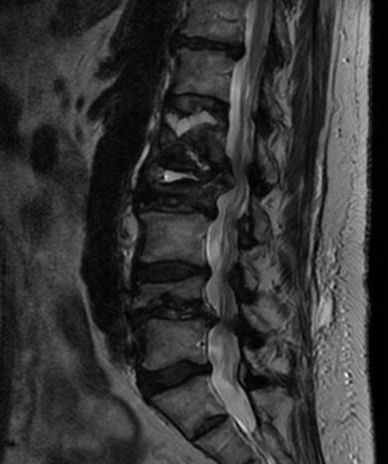 [Figure caption and citation for the preceding image starts]: Anteroposterior and lateral x-ray images of patient with osteoporotic spinal compression fractures of L1,2,4 following kyphoplastyPersonal collection of Nasir A. Quraishi [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior and lateral x-ray images of patient with osteoporotic spinal compression fractures of L1,2,4 following kyphoplastyPersonal collection of Nasir A. Quraishi [Citation ends].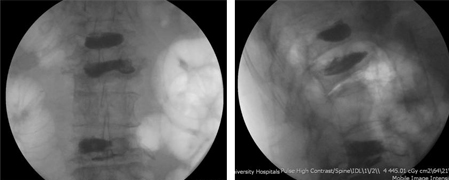
Acute multiple column fracture
Rarely, osteoporotic compression fractures can involve the middle and/or posterior spinal columns, in addition to the anterior column. These types of fracture are potentially unstable and prone to neurological involvement. The appearance or progression of neurological signs or symptoms following an osteoporotic compression fracture is an indication for open surgical decompression and reconstruction. Some surgeons may perform kyphoplasty or vertebroplasty as an additional measure during the open surgical procedure. Appropriate analgesia is prescribed to reduce pain, and patients are placed on strict bed rest while definitive treatment is planned.
Use of this content is subject to our disclaimer