Approach
The diagnosis of uterine fibroids typically occurs after pelvic examination for evaluation of heavy menstrual bleeding or pelvic pain. Pelvic ultrasonography is the universal standard diagnostic test for confirmation.
Clinical history
Key historical factors for the diagnosis of uterine fibroids include heavy menstrual bleeding, pelvic pain (pain, pressure, or dysmenorrhoea), pelvic mass, or infertility.[23] Other symptoms may include bloating, urinary complaints, and constipation. Some patients may have a history of hypertension, infertility, or pregnancy wastage. There may be a family history of fibroids.
Less frequently, large fibroids may present with symptoms caused by pressure on surrounding organs, including urinary frequency or, more rarely, urinary retention (secondary to urethral obstruction), and rectal symptoms such as constipation and abdominal cramping. Rarely, large fibroids can cause compression of the great vessels or even compromise of pulmonary ventilation.
Physical examination
Findings of a firm, enlarged, and irregularly shaped uterus on bimanual pelvic examination are characteristic for uterine fibroids. In cases of large tumours, a central irregular mass can be palpated on transabdominal examination.[4]
Ultrasound imaging
Pelvic imaging by transabdominal and transvaginal ultrasound is the most common initial study obtained for the diagnosis of uterine fibroids and is universally available.[43][44] It is the least invasive outpatient technique available for imaging the pelvic organs including the uterus.[45] It is also inexpensive, reasonably painless, rapid, and accurate.[46] A thorough initial ultrasound examination should include both transvaginal and transabdominal views of the pelvis to ensure uterine pathology beyond the limits of the transvaginal probe is detected.[45][Figure caption and citation for the preceding image starts]: Solitary intramural fibroid as shown by transvaginal pelvic ultrasound (TVUS) demonstrating posterior intramural mass lying between a normal-appearing trilaminar endometrial stripe and posterior uterine serosaFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].
Submucosal fibroids are generally better visualised by transvaginal ultrasound and can still pose a diagnostic dilemma in differentiating these intracavitary lesions from endometrial polyps. [Figure caption and citation for the preceding image starts]: Transvaginal pelvic ultrasound (TVUS) shows a midline posterior fundal fibroid greatly distorting the endometrial cavityFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].
Additionally, transvaginal ultrasonography has been demonstrated to have 100% sensitivity and 94% specificity in the diagnosis of submucous fibroids. Less than perfect specificity is due to difficulty in distinguishing endometrial polyps from submucous fibroids by transvaginal ultrasound.[47]
Endometrial sampling
Endometrial carcinoma is the most common female genital tract cancer in the developed world and 90% of patients with this diagnosis develop symptomatic bleeding or discharge.[48] Because of the high prevalence of uterine fibroids in the general female population, a substantial number of patients will present with abnormal vaginal bleeding in association with uterine fibroids. It is therefore vital that consideration for endometrial sampling be a part of the initial diagnostic evaluation for any patient presenting with abnormal vaginal bleeding, regardless of the presence or absence of fibroids.
The accuracy of endometrial biopsy for the detection of endometrial carcinoma is about 90%.[49] Because 5% to 10% of endometrial cancers occur in women younger than the age of 40 years, candidates for histological evaluation of the endometrium would include irregular and heavy bleeding in patients younger than 40 years of age, as well as any abnormal bleeding during the perimenopausal years (age 40 years and older). Any postmenopausal bleeding should be considered endometrial cancer until proven otherwise by histological examination of the endometrium. Persistence of irregular vaginal bleeding despite a negative endometrial biopsy should be pursued by dilatation and curettage.[50]
Saline infusion sonohysterography
Sonohysterography is another excellent ancillary modality with high sensitivity for the detection of submucous and intramural fibroids.[43][51]
Saline infusion sonohysterography should be obtained for further evaluation of suspected uterine abnormalities noted during pelvic ultrasound, especially those associated with the endometrial cavity itself and in cases of suboptimal visualisation of the uterus and uterine cavity. It can also serve as an ancillary first-line imaging modality for the evaluation of premenopausal and postmenopausal women experiencing abnormal bleeding and women undergoing evaluation for infertility and recurrent abortion.[51][52] For intracavitary lesions detected by transvaginal ultrasound, the biggest challenge is in differentiating endometrial polyps from submucous uterine fibroids; both are space-occupying intracavitary lesions. Endometrial polyps are completely intraluminal in location and can be seen to freely move during injection of saline. [Figure caption and citation for the preceding image starts]: Sonohysterography shows several small intracavitary masses suspicious for polypsFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].
Transabdominal sonohysterography was found to have 100% sensitivity, specificity, and predictive values in a study of 52 women undergoing hysterectomy for benign gynaecological indications.[53] In one review of eight studies, sonohysterography displayed an overall sensitivity of 94% (range 91% to 100%) and specificity of 95% (range 88% to 100%) for the diagnosis of submucous uterine fibroids, higher than that of transvaginal ultrasound alone.[54] The authors of the review concluded that hysteroscopy and sonohysterography are equally effective in the detection of submucous fibroids. However, another study reported 100% sensitivity and 96% specificity of hysteroscopy for the diagnosis of submucous fibroids. In this study, the comparison was against vaginal ultrasonography not sonohysterography. Furthermore, advancements in ultrasound technology over the last few years might change the conclusions of studies performed using older ultrasound technology.[47]
Compared with simple transvaginal and transabdominal pelvic ultrasound, sonohysterography is a moderately invasive procedure consisting of placement of a semi-rigid sterile catheter (usually approximately 5 French) through the cervical os and into the uterine cavity to the fundus using sterile technique. Sterile saline is then injected through the catheter under real-time ultrasonographic imaging in at least two planes using a high-frequency endovaginal ultrasound probe.[52] Performance of this procedure can be uncomfortable in a minority of cases.[55] Contraindications to sonohysterography include pregnancy, pelvic infection, or unexplained pelvic tenderness. A baseline pelvic ultrasound should always precede performance of sonohysterography.[52]
Sonohysterography has largely replaced hysterosalpingography in the evaluation of the uterine cavity and subendometrial conditions including endometrial polyps and submucous uterine fibroids due to higher sensitivity, between 91% and 94%.[56][57][58] Along with uterine fibroids, endometrial polyps are a common cause of abnormal bleeding and can be difficult to distinguish from submucous fibroids.[51] Sonohysterography is extremely sensitive (sensitivity >90%) with somewhat lower specificity.[54] An important additional advantage of sonohysterography over hysterosalpingography and hysteroscopy is its ability to better define the intrauterine extent of submucous fibroids.
One systematic review and meta-analysis in 2017 concluded that 2D sonohysterography is a highly sensitive method for detecting endometrial polyps and submucosal uterine fibroids and suggested that it is a potential first-line diagnostic method in women with abnormal uterine bleeding. Low-quality evidence suggests that 3D saline infusion sonography may be very accurate in detecting intracavitary abnormalities.[59] More studies are needed on 3D sonohysterography.[60]
It is recommended that saline infusion sonography should not be used as a first-line diagnostic tool for heavy menstrual bleeding.[61]
Hysteroscopy
Hysteroscopy is generally considered to be a moderately invasive and uncomfortable procedure that has historically served as the standard and definitive test for the diagnosis of intrauterine pathology.[62]
Although an excellent tool for the diagnosis of endometrial polyps (sensitivity 92%), it performs significantly less favourably for the diagnosis of submucous fibroids, with a sensitivity of only 82% and a specificity of 87% (compared with 94% sensitivity and 95% specificity for sonohysterography).[54][Figure caption and citation for the preceding image starts]: Hysteroscopic examination of the uterine cavity demonstrates the presence of two contiguous submucous uterine fibroids in this patient with persistent heavy menstrual bleedingFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].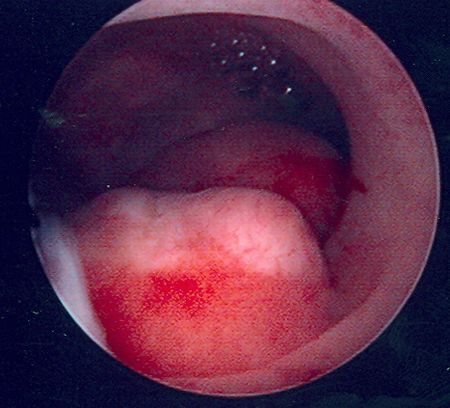 [Figure caption and citation for the preceding image starts]: Hysteroscopic image of a large pedunculated submucous uterine fibroidFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Hysteroscopic image of a large pedunculated submucous uterine fibroidFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].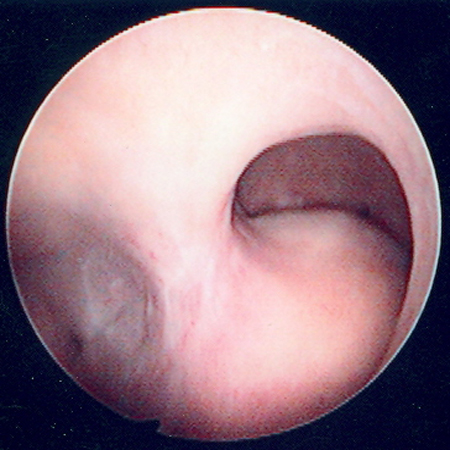 [Figure caption and citation for the preceding image starts]: Multiple polyps are identified on hysteroscopic examination of the uterine cavity in this patient with persistent vaginal spottingFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Multiple polyps are identified on hysteroscopic examination of the uterine cavity in this patient with persistent vaginal spottingFrom the personal collection of Dr M.F. Mitwally and Dr R.J. Fischer; used with permission [Citation ends].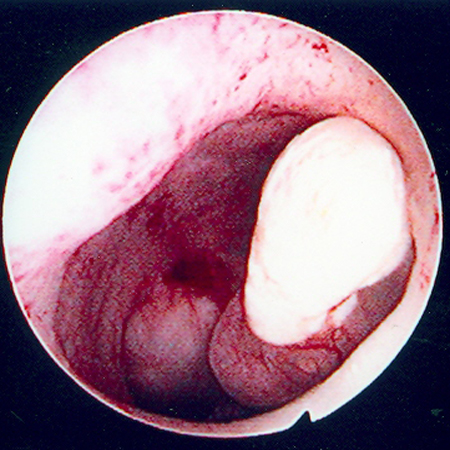
For diagnosis of endometrial polyps, hysteroscopy is extremely sensitive (sensitivity >90%) with somewhat lower specificities.[54]
Advantages of hysteroscopy include the ability to both visualise and obtain a surgical specimen for histological examination during the same procedure.[46] Hysteroscopy is important for the investigation of persistent abnormal uterine bleeding, particularly if fibroids are suspected, and endometrial biopsy can be considered at the same time in women who are at high risk of endometrial pathology.[61]
Magnetic resonance imaging (MRI)
Ancillary imaging by MRI can be helpful in special cases such as those involving pedunculated subserosal fibroids that may mimic an ovarian tumour, or cases in which uterine sarcoma is suspected.[63][64] MRI is a relatively expensive modality, but is superior for evaluating the degree and extent to which a submucous fibroid is embedded into the uterine wall.[43] This can be important preoperatively in determining which patients would benefit from minimally invasive treatment of uterine fibroids such as hysteroscopic resection of symptomatic submucous uterine fibroids.[54] In equivocal cases or those associated with cervical stenosis or large body habitus, MRI can be very helpful and accurate in diagnosing endometrial polyps.[65] Furthermore, MRI can be an excellent modality for cases in which ultrasound proves inadequate.[46]
MRI is very useful in the evaluation of indeterminate adnexal masses.[66] MRI may be helpful in differentiating uterine fibroids from adenomyosis or endometriosis, which can cause similar symptoms.[43]
Due to absence of ionising radiation, MRI during pregnancy is safe and can be particularly helpful in identifying fibroids otherwise not seen by conventional ultrasound because of an enlarged gravid uterus.[67]
Although MRI findings in cases of leiomyosarcoma are variable, there are a number of findings suggestive of this malignancy, which can aid in distinguishing benign fibroids from malignancy. Diffuse leiomyomatosis may also be diagnosed by this modality.[68]
Emerging tests
Sonoelastography: There are few studies of sonoelastography in diagnosing uterine fibroids. Elastography could be useful for discriminating adenomyosis from fibroids, but the results are conflicting. The addition of sonoelastography to ultrasound seems to be useful in the differentiation of fibroids, adenomyosis, and normal uteri, as reflected by an increase in accuracy and diagnostic agreement. The availability of sonoelastography in the differentiation of these two entities needs to be confirmed in larger trials before solid conclusions can be made.[69][70]
MR elastography: There are few studies of MRI elastography (MR-E). It seems the main value of MR-E is in evaluation of the response of uterine fibroids to treatment, especially high-intensity focused ultrasound therapy. Further studies are needed to determine whether fibroid stiffness determined by MR-E may serve as an imaging biomarker that helps to predict treatment response.[71]
Use of this content is subject to our disclaimer