Differentials
Acute coronary syndrome
SIGNS / SYMPTOMS
A careful history is key to determine features of acute coronary syndrome such as chest pain, sweating, or nausea.
In addition, the patient may have risk factors for coronary artery disease such as smoking, hypertension, or diabetes.
INVESTIGATIONS
Right coronary artery or left anterior descending artery ischaemia in particular may produce precordial lead changes with ST segment elevation on ECG which may be confused for Brugada pattern (BrP).
Cardiac biomarkers will be elevated with ST-elevation myocardial infarction (MI) and non-ST elevation MI.[Figure caption and citation for the preceding image starts]: 12-Lead ECG with ST-segment elevation lead V1 to V4From the personal collection of Dr Mahi Ashwath; used with permission [Citation ends].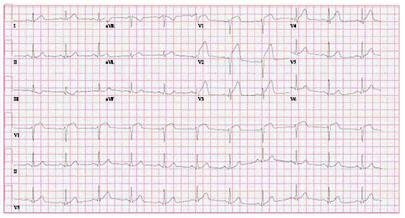
Arrhythmogenic cardiomyopathy
SIGNS / SYMPTOMS
Inherited cardiomyopathy resulting from defective desmosomal proteins[49]
Fibrofatty replacement of myocytes lead to scar-related ventricular arrhythmias, often in the young
Up to 16% of patients with had a positive sodium-channel blocker challenge in one study.[73]
INVESTIGATIONS
Cardiac MRI assessment may show structural right ventricular or right ventricular outflow tract changes with arrhythmogenic right ventricular cardiomyopathy (AVRC), whereas in Brugada syndrome (BrS) structural abnormalities may not be easily detected.
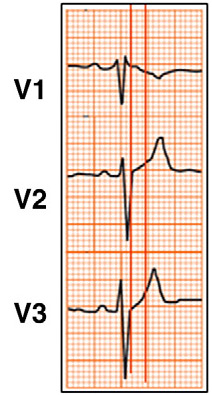
There may also be differences seen in the precordial leads on ECG, particularly leads V1 and V2. With ARVC T-wave inversion in right precordial leads usually has no preceding or mildly upward ST-segment, with BrS there is characteristically a high take off and ST segment elevation that is downsloping.[74] There may also be epsilon waves with ARVC. ECG changes are typically fixed with AVRC, rather than dynamic.
[Figure caption and citation for the preceding image starts]: 3-lead ECG showing findings suggestive of arrhythmogenic right ventricular cardiomyopathyBayés de Luna A et al. J Electrocardiol. 2012 Sep;45(5):433-42; used with permission [Citation ends].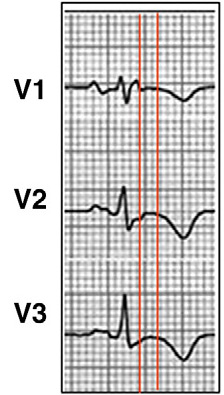
Athlete’s heart
SIGNS / SYMPTOMS
Typically seen in male endurance athletes without cardiac symptoms.
No family history of HCM or sudden death.
Hypertrophy will regress with cessation of exercise.[75]
INVESTIGATIONS
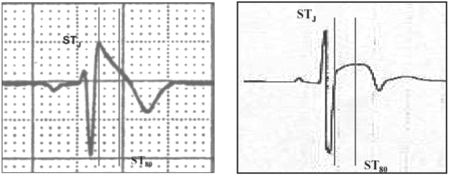
ECG: There will be upsloping ST segment elevation of early repolarisation whereas in type 1 Brugada syndrome coved ST segment elevation would be seen, resulting in a broad R wave. The ‘Corrado index’ measures the ST elevation at the start of the ST segment/J-point (STJ) and 80 ms after the start of the ST segment (ST80). The downsloping ST segment will have a STJ/ST80 ratio >1 in type 1 Brugada syndrome, but <1 in the athlete.[76]
Echocardiography: Will characteristically show increased left ventricular (LV) chamber dimension (LV end-diastolic dimension or LV end-diastolic >55 mm), symmetric left ventricular hypertrophy (LVH) with a homogeneous-appearing myocardium.
Wall thicknesses may occasionally exceed upper normal limits (12 mm).
LV filling pattern is most often normal.[75]
[Figure caption and citation for the preceding image starts]: Brugada type 1 ECG (left) in comparison to early repolarisation with ‘convex’ ST segment elevation in a trained athlete (right). [Vertical lines mark the J-point (STJ) and 80 ms after the J-point (ST80). The ‘downsloping’ ST segment elevation in Brugada pattern has an STJ/ST80 ratio >1. Early repolarisation patterns in the athlete shows an initial ‘upsloping’ ST segment elevation with STJ/ST80 ratio <1].Drezner JA et al. Br J Sports Med 2017 May;51(9):704-31; used with permission [Citation ends].
Pectus excavatum
SIGNS / SYMPTOMS
A congenital chest wall deformity may be seen on examination.
INVESTIGATIONS
ECG findings in pectus excavatum may include a negative P wave in V1 (with V1 lead in the standard position i.e., fourth intercostal space to the right of the sternum), a well defined, peaked R wave in V1 which may be followed by a mildly elevated ST segment. The T wave is usually negative or biphasic in V1 and positive in V2 with pectus excavatum.
CT scan will show depression of the sternum.
[Figure caption and citation for the preceding image starts]: 3-lead ECG showing findings suggestive of pectus excavatumBayés de Luna A et al. J Electrocardiol. 2012 Sep;45(5):433-42; used with permission [Citation ends].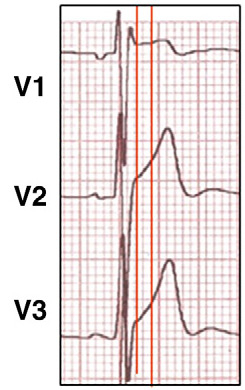
Incomplete right bundle branch block (RBBB)
SIGNS / SYMPTOMS
Diagnosis is primarily distinguished from Brugada syndrome (BrS) on ECG rather than clinical findings.
INVESTIGATIONS
On ECG look for the following features of RBBB:
Peaked positive terminal R wave. In type 2 Brugada pattern, the R wave is rounded, wide, and usually of relatively low voltage compared with RBBB.
Identical QRS complex duration in leads V1-V2 to that observed in lead V6.
Characteristic widened S wave, which is absent in most cases of Brugada syndrome.[77]
[Figure caption and citation for the preceding image starts]: 3-lead ECG showing right bundle branch blockBayés de Luna A et al. J Electrocardiol. 2012 Sep;45(5):433-42; used with permission [Citation ends].
Hypokalaemia
SIGNS / SYMPTOMS
Hypokalaemia can produce ECG patterns that mimic the Brugada ECG patterns but is clinically distinct from BrS.[78] The cause of hypokalaemia is often apparent from the history, this may include the use of known causative medications (such as diuretics, corticosteroids, beta-2 agonists, amphotericin B, chloroquine or theophylline toxicity, laxatives), a history of gastrointestinal losses (such as vomiting or diarrhoea), or underlying medical conditions leading to urinary loss of potassium (such as renal tubular acidosis).
INVESTIGATIONS
Serum potassium levels <3.5 mmol/L (<3.5 mEq/L).
The ECG in patients with hypokalemia may typically show ST segment depression, decrease in the amplitude of the T wave, and an increase in the amplitude of U waves (often seen in the lateral precordial leads V4 to V6).
[Figure caption and citation for the preceding image starts]: 12-lead ECG demonstrating prominent U-waves in a patient with hypokalaemiaFrom: Lin HW, Chau T, Lin CS, Lin SH, Recurring paralysis, BMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0577 [Citation ends].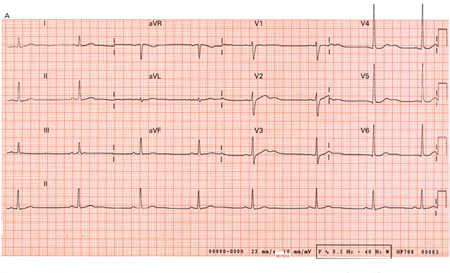 Other patterns of arrhythmias with hypokalaemia, include sinus bradycardia, premature atrial and ventricular beats, paroxysmal atrial or junctional tachycardia, atrioventricular block, ventricular tachycardia, or fibrillation.[79]
Other patterns of arrhythmias with hypokalaemia, include sinus bradycardia, premature atrial and ventricular beats, paroxysmal atrial or junctional tachycardia, atrioventricular block, ventricular tachycardia, or fibrillation.[79]
Use of this content is subject to our disclaimer