Pericarditis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
Look out for this icon: for treatment options that are affected, or added, as a result of your patient's comorbidities.
suspected pericarditis
triage and consider admission to hospital
Organise admission to hospital for any patient with:
A clinical presentation that suggests an underlying aetiology requiring inpatient management[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Any of the following high-risk features:[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Major risk factors (associated with poor prognosis after multivariate analysis):
High fever (i.e., >38°C [>100.4°F])
Subacute course (i.e., symptoms over several days without a clear-cut acute onset)
Evidence of a large pericardial effusion (i.e., diastolic echo-free space >20 mm)
Cardiac tamponade
Failure to respond within 7 days to a non-steroidal anti-inflammatory drug
Minor risk factors (based on expert opinion and literature review)
Pericarditis associated with myocarditis (myopericarditis; associated with a rise in troponin)
Immunosuppression
Trauma
Oral anticoagulant therapy.
Ensure a patient with any of these high-risk features has investigation of the underlying cause, as well as careful observation and follow-up.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Otherwise, if the patient does not have any high-risk features or a clinical presentation that suggests an underlying aetiology requiring inpatient management, consider outpatient management. Start treatment (i.e., empirical anti-inflammatories) and arrange follow-up after 1 week to assess the response to treatment.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
pericardiocentesis
Additional treatment recommended for SOME patients in selected patient group
If you suspect cardiac tamponade, a life-threatening complication of pericarditis, get help immediately from a senior colleague; these patients require urgent pericardiocentesis.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com See Cardiac tamponade.
Other indications for pericardiocentesis include suspected purulent pericarditis, high suspicion of neoplastic pericarditis, or a large or symptomatic pericardial effusion in a patient with non-purulent pericarditis.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Although very rare in the antibiotic era, purulent pericarditis is life-threatening and requires a high index of suspicion. Seek early input from a senior or specialist colleague.[44]Kanwal A, Avgeropoulos D, Kaplan JG, et al. Idiopathic purulent pericarditis: a rare diagnosis. Am J Case Rep. 2020 Feb 28;21:e921633. http://www.ncbi.nlm.nih.gov/pubmed/32107365?tool=bestpractice.com
idiopathic or viral (non-purulent)
non-steroidal anti-inflammatory drug (NSAID)
Start an NSAID (as long as there are no contraindications) immediately after diagnosis for symptom management.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
To guide treatment duration, evaluate the patient’s symptoms and their C-reactive protein levels. In general, for a patient with uncomplicated pericarditis, continue the NSAID at the initial dose for 1 to 2 weeks before tapering gradually.
Practical tip
A common error is to taper the NSAID too quickly, which can result in recurrence of symptoms.
Choice of drug is based on patient characteristics (e.g., contraindications, previous efficacy, or side effects), presence of concomitant diseases (e.g., favour aspirin over other NSAIDs if antiplatelet therapy is required), and physician expertise.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [18]Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020 Jan 7;75(1):76-92. https://www.jacc.org/doi/full/10.1016/j.jacc.2019.11.021 http://www.ncbi.nlm.nih.gov/pubmed/31918837?tool=bestpractice.com
Practical tip
Aspirin is preferred for patients developing pericarditis after a myocardial infarction, as other NSAIDs adversely affect myocardial healing and are associated with increased risk of future cardiac events.[58]Lilly LS. Treatment of acute and recurrent idiopathic pericarditis. Circulation. 2013 Apr 23;127(16):1723-6. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.111.066365 http://www.ncbi.nlm.nih.gov/pubmed/23609551?tool=bestpractice.com If high-dose aspirin is not effective, consider paracetamol or an opioid analgesic.
NSAIDs reduce fever, chest pain, and inflammation but do not prevent tamponade, constriction, or recurrent pericarditis.
Primary options
aspirin: 750-1000 mg orally every 8 hours for 1-2 weeks, then decrease by 250-500 mg/dose every 1-2 weeks
OR
ibuprofen: 600 mg orally every 8 hours for 1-2 weeks, then decrease by 200-400 mg/dose every 1-2 weeks
These drug options and doses relate to a patient with no comorbidities.
Primary options
aspirin: 750-1000 mg orally every 8 hours for 1-2 weeks, then decrease by 250-500 mg/dose every 1-2 weeks
OR
ibuprofen: 600 mg orally every 8 hours for 1-2 weeks, then decrease by 200-400 mg/dose every 1-2 weeks
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
aspirin
OR
ibuprofen
proton-pump inhibitor
Treatment recommended for ALL patients in selected patient group
Due to the high doses of NSAIDs used, give a proton-pump inhibitor (e.g., omeprazole) alongside NSAID therapy to protect against gastrointestinal ulcer formation.[11]Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004 Nov 18;351(21):2195-202. http://www.ncbi.nlm.nih.gov/pubmed/15548780?tool=bestpractice.com [13]Little WC, Freeman GL. Pericardial disease. Circulation. 2006 Mar 28;113(12):1622-32. http://circ.ahajournals.org/cgi/content/full/113/12/1622 http://www.ncbi.nlm.nih.gov/pubmed/16567581?tool=bestpractice.com [39]Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010 Feb 23;121(7):916-28. http://www.ncbi.nlm.nih.gov/pubmed/20177006?tool=bestpractice.com [40]Imazio M, Brucato A, Trinchero R, et al. Diagnosis and management of pericardial diseases. Nat Rev Cardiol. 2009 Dec;6(12):743-51. http://www.ncbi.nlm.nih.gov/pubmed/19859068?tool=bestpractice.com
Primary options
omeprazole: 20 mg orally once daily
These drug options and doses relate to a patient with no comorbidities.
Primary options
omeprazole: 20 mg orally once daily
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
omeprazole
colchicine
Treatment recommended for ALL patients in selected patient group
If the patient has idiopathic or viral pericarditis, add colchicine and continue it for 3 months.[20]Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA. 2015 Oct 13;314(14):1498-506. https://iris.unito.it/handle/2318/1576078#.XAFHbdv7S70 http://www.ncbi.nlm.nih.gov/pubmed/26461998?tool=bestpractice.com [59]Galluzzo A, Imazio M. Advances in medical therapy for pericardial diseases. Expert Rev Cardiovasc Ther. 2018 Sep;16(9):635-43. http://www.ncbi.nlm.nih.gov/pubmed/30103638?tool=bestpractice.com [60]Bayes-Genis A, Adler Y, de Luna AB, et al. Colchicine in pericarditis. Eur Heart J. 2017 Jun 7;38(22):1706-9. https://academic.oup.com/eurheartj/article/38/22/1706/3861991 http://www.ncbi.nlm.nih.gov/pubmed/30052886?tool=bestpractice.com
Colchicine is crucial to prevent recurrent pericarditis, improve response, and increase remission rates.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Order a baseline full blood count before starting treatment because colchicine may cause neutropenia and bone marrow suppression.
Use colchicine with caution in patients with renal and hepatic impairment because it may be contraindicated with certain medications. A dose reduction may be required.
In practice, avoid colchicine where possible in patients who are very frail or have impaired mobility, due to the high likelihood of treatment-related diarrhoea.
While tapering the dose is not mandatory, consider doing so in the last few weeks of treatment to prevent persistence of symptoms and recurrence.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Practical tip
Warn the patient that colchicine may cause gastrointestinal side effects such as diarrhoea.[62]Hemkens LG, Ewald H, Gloy VL, et al. Colchicine for prevention of cardiovascular events. Cochrane Database Syst Rev. 2016 Jan 27;(1):CD011047. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011047.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/26816301?tool=bestpractice.com Gradually increase the dose until onset of side effects. Consider reducing the dose if the patient is unable to tolerate the drug at full initial dose.[63]Markel G, Imazio M, Brucato A, et al. Prevention of recurrent pericarditis with colchicine in 2012. Clin Cardiol. 2013 Mar;36(3):125-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6649517 http://www.ncbi.nlm.nih.gov/pubmed/23404655?tool=bestpractice.com
Primary options
colchicine: <70 kg body weight: 0.5 mg orally once daily for 3 months, then may taper to 0.5 mg once daily on alternate days in the last weeks; ≥70 kg body weight: 0.5 mg orally twice daily for 3 months, then may taper to 0.5 mg once daily in the last weeks
These drug options and doses relate to a patient with no comorbidities.
Primary options
colchicine: <70 kg body weight: 0.5 mg orally once daily for 3 months, then may taper to 0.5 mg once daily on alternate days in the last weeks; ≥70 kg body weight: 0.5 mg orally twice daily for 3 months, then may taper to 0.5 mg once daily in the last weeks
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
colchicine
exercise restriction
Treatment recommended for ALL patients in selected patient group
Advise the patient to restrict strenuous physical activities:[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [64]Pelliccia A, Solberg EE, Papadakis M, et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2019 Jan 1;40(1):19-33. https://academic.oup.com/eurheartj/article/40/1/19/5248228 http://www.ncbi.nlm.nih.gov/pubmed/30561613?tool=bestpractice.com
Non-athletes: until symptoms have resolved and C-reactive protein has normalised, while also taking into account the patient’s previous history and other clinical conditions[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Athletes: for a minimum of 3 months until symptoms have resolved and C-reactive protein, ECG, and echocardiography have normalised.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
corticosteroid
Additional treatment recommended for SOME patients in selected patient group
Only consider using a low-dose corticosteroid with specialist guidance from a rheumatologist and a cardiologist.
A corticosteroid is an appropriate option for a small proportion of patients, specifically if:
An infectious cause has been excluded and there is failure of, or contraindication to, NSAIDs and/or colchicine[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
There is a specific indication for use (e.g., the presence of an autoimmune disease). Corticosteroids are used in combination with colchicine in this scenario.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Do not use corticosteroids in a patient with viral pericarditis because of the risk of re-activation of the viral infection and ongoing inflammation.
Use corticosteroids at low to moderate doses.[18]Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020 Jan 7;75(1):76-92. https://www.jacc.org/doi/full/10.1016/j.jacc.2019.11.021 http://www.ncbi.nlm.nih.gov/pubmed/31918837?tool=bestpractice.com Continue with the initial dose until symptoms have resolved and the patient’s C-reactive protein level has normalised. Once this is achieved, taper the dose gradually.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Primary options
prednisolone: 0.2 to 0.5 mg/kg/day orally until resolution of symptoms, then gradually taper according to local protocols
These drug options and doses relate to a patient with no comorbidities.
Primary options
prednisolone: 0.2 to 0.5 mg/kg/day orally until resolution of symptoms, then gradually taper according to local protocols
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
prednisolone
not idiopathic or viral (non-purulent)
treatment of the underlying cause
Treat the underlying cause if known. Pericarditis can be caused by:
Tuberculosis (a common cause in the developing world)
Secondary immune processes (e.g., rheumatic fever, post-cardiotomy syndrome, post-myocardial infarction syndrome)
Metabolic disorders (e.g., uraemia, myxoedema), radiotherapy
Cardiac surgery
Percutaneous cardiac interventions
Systemic autoimmune disorders (e.g., rheumatoid arthritis, systemic sclerosis, reactive arthritis, familial Mediterranean fever, systemic vasculitides, inflammatory bowel disease)
Bacterial/fungal/parasitic infections
Trauma
Certain drugs (e.g., hydralazine, antineoplastic drugs, clozapine, tumour necrosis factor-alpha inhibitors, phenytoin)[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Neoplasms.
Seek specialist advice as needed.
If the patient has tuberculous pericarditis, first-line treatment is 4 to 6 weeks of antituberculous therapy.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
When tuberculous pericarditis is confirmed in a non-endemic area, a suitable 6-month regimen is effective; empirical therapy is not required in the absence of an established diagnosis in non-endemic areas.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Adjunctive therapy with corticosteroids and immunotherapy has not been shown to be beneficial.[66]Mayosi BM, Ntsekhe M, Bosch J, et al. Prednisolone and Mycobacterium indicus pranii in tuberculous pericarditis. N Engl J Med. 2014 Sep 18;371(12):1121-30. http://www.nejm.org/doi/full/10.1056/NEJMoa1407380#t=article http://www.ncbi.nlm.nih.gov/pubmed/25178809?tool=bestpractice.com However, corticosteroids may be considered for a patient with tuberculous pericarditis who is HIV-negative.[68]Wiysonge CS, Ntsekhe M, Thabane L, et al. Interventions for treating tuberculous pericarditis. Cochrane Database Syst Rev. 2017 Sep 13;(9):CD000526. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000526.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/28902412?tool=bestpractice.com [
 ]
What are the benefits and harms of steroids for people with tuberculous pericarditis?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1937/fullShow me the answer
]
What are the benefits and harms of steroids for people with tuberculous pericarditis?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1937/fullShow me the answer Pericardiectomy is recommended if the patient does not improve or is deteriorating after 4 to 8 weeks of antituberculosis therapy.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Most patients with uraemic pericarditis respond to intensive dialysis within 1 to 2 weeks.
Autoimmune disorders are treated with corticosteroids and/or another immunosuppressive therapy depending on the specific condition.
Treatment of neoplasms may involve any combination of radiotherapy, chemotherapy, or surgery depending on the type of tumour identified.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [39]Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010 Feb 23;121(7):916-28. http://www.ncbi.nlm.nih.gov/pubmed/20177006?tool=bestpractice.com [40]Imazio M, Brucato A, Trinchero R, et al. Diagnosis and management of pericardial diseases. Nat Rev Cardiol. 2009 Dec;6(12):743-51. http://www.ncbi.nlm.nih.gov/pubmed/19859068?tool=bestpractice.com
non-steroidal anti-inflammatory drug (NSAID)
Treatment recommended for ALL patients in selected patient group
Start an NSAID (as long as there are no contraindications) immediately after diagnosis for symptom management.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
To guide treatment duration, evaluate the patient’s symptoms and their C-reactive protein levels. In general, for a patient with uncomplicated pericarditis, continue the NSAID at the initial dose for 1 to 2 weeks before tapering gradually.
Practical tip
A common error is to taper the NSAID too quickly, which can result in recurrence of symptoms.
Choice of drug is based on patient characteristics (e.g., contraindications, previous efficacy, or side effects), presence of concomitant diseases (e.g., favour aspirin over other NSAIDs if antiplatelet therapy is required), and physician expertise.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [18]Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020 Jan 7;75(1):76-92. https://www.jacc.org/doi/full/10.1016/j.jacc.2019.11.021 http://www.ncbi.nlm.nih.gov/pubmed/31918837?tool=bestpractice.com
Practical tip
Aspirin is preferred for patients developing pericarditis after a myocardial infarction, as other NSAIDs adversely affect myocardial healing and are associated with increased risk of future cardiac events.[58]Lilly LS. Treatment of acute and recurrent idiopathic pericarditis. Circulation. 2013 Apr 23;127(16):1723-6. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.111.066365 http://www.ncbi.nlm.nih.gov/pubmed/23609551?tool=bestpractice.com If high-dose aspirin is not effective, consider paracetamol or an opioid analgesic.
NSAIDs reduce fever, chest pain, and inflammation but do not prevent tamponade, constriction, or recurrent pericarditis.
Primary options
aspirin: 750-1000 mg orally every 8 hours for 1-2 weeks, then decrease by 250-500 mg/dose every 1-2 weeks
OR
ibuprofen: 600 mg orally every 8 hours for 1-2 weeks, then decrease by 200-400 mg/dose every 1-2 weeks
These drug options and doses relate to a patient with no comorbidities.
Primary options
aspirin: 750-1000 mg orally every 8 hours for 1-2 weeks, then decrease by 250-500 mg/dose every 1-2 weeks
OR
ibuprofen: 600 mg orally every 8 hours for 1-2 weeks, then decrease by 200-400 mg/dose every 1-2 weeks
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
aspirin
OR
ibuprofen
proton-pump inhibitor
Treatment recommended for ALL patients in selected patient group
Due to the high doses of NSAIDs used, give a proton-pump inhibitor (e.g., omeprazole) alongside NSAID therapy to protect against gastrointestinal ulcer formation.[11]Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004 Nov 18;351(21):2195-202. http://www.ncbi.nlm.nih.gov/pubmed/15548780?tool=bestpractice.com [13]Little WC, Freeman GL. Pericardial disease. Circulation. 2006 Mar 28;113(12):1622-32. http://circ.ahajournals.org/cgi/content/full/113/12/1622 http://www.ncbi.nlm.nih.gov/pubmed/16567581?tool=bestpractice.com [39]Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010 Feb 23;121(7):916-28. http://www.ncbi.nlm.nih.gov/pubmed/20177006?tool=bestpractice.com [40]Imazio M, Brucato A, Trinchero R, et al. Diagnosis and management of pericardial diseases. Nat Rev Cardiol. 2009 Dec;6(12):743-51. http://www.ncbi.nlm.nih.gov/pubmed/19859068?tool=bestpractice.com
Primary options
omeprazole: 20 mg orally once daily
These drug options and doses relate to a patient with no comorbidities.
Primary options
omeprazole: 20 mg orally once daily
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
omeprazole
Plus – colchicine (unless the patient has TB pericarditis)
colchicine (unless the patient has TB pericarditis)
Treatment recommended for ALL patients in selected patient group
Add colchicine, unless the patient has tuberculosis pericarditis.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [20]Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA. 2015 Oct 13;314(14):1498-506. https://iris.unito.it/handle/2318/1576078#.XAFHbdv7S70 http://www.ncbi.nlm.nih.gov/pubmed/26461998?tool=bestpractice.com [59]Galluzzo A, Imazio M. Advances in medical therapy for pericardial diseases. Expert Rev Cardiovasc Ther. 2018 Sep;16(9):635-43. http://www.ncbi.nlm.nih.gov/pubmed/30103638?tool=bestpractice.com [60]Bayes-Genis A, Adler Y, de Luna AB, et al. Colchicine in pericarditis. Eur Heart J. 2017 Jun 7;38(22):1706-9. https://academic.oup.com/eurheartj/article/38/22/1706/3861991 http://www.ncbi.nlm.nih.gov/pubmed/30052886?tool=bestpractice.com [61]Andreis A, Imazio M, Casula M, et al. Colchicine efficacy and safety for the treatment of cardiovascular diseases. Intern Emerg Med. 2021 Sep;16(6):1691-700. https://www.doi.org/10.1007/s11739-021-02654-7 http://www.ncbi.nlm.nih.gov/pubmed/33704674?tool=bestpractice.com See Treatment of the underlying cause above. Continue colchicine for 3 months.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [20]Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA. 2015 Oct 13;314(14):1498-506. https://iris.unito.it/handle/2318/1576078#.XAFHbdv7S70 http://www.ncbi.nlm.nih.gov/pubmed/26461998?tool=bestpractice.com [59]Galluzzo A, Imazio M. Advances in medical therapy for pericardial diseases. Expert Rev Cardiovasc Ther. 2018 Sep;16(9):635-43. http://www.ncbi.nlm.nih.gov/pubmed/30103638?tool=bestpractice.com [60]Bayes-Genis A, Adler Y, de Luna AB, et al. Colchicine in pericarditis. Eur Heart J. 2017 Jun 7;38(22):1706-9. https://academic.oup.com/eurheartj/article/38/22/1706/3861991 http://www.ncbi.nlm.nih.gov/pubmed/30052886?tool=bestpractice.com
Colchicine is crucial to prevent recurrent pericarditis, improve response, and increase remission rates.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Order a baseline full blood count before starting treatment because colchicine may cause neutropenia and bone marrow suppression.
Use colchicine with caution in patients with renal and hepatic impairment because it may be contraindicated with certain medications. A dose reduction may be required.
In practice, avoid colchicine where possible in patients who are very frail or have impaired mobility, due to the high likelihood of treatment-related diarrhoea.
While tapering the dose is not mandatory, consider doing so in the last few weeks of treatment to prevent persistence of symptoms and recurrence.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Practical tip
Warn the patient that colchicine may cause gastrointestinal side effects such as diarrhoea.[62]Hemkens LG, Ewald H, Gloy VL, et al. Colchicine for prevention of cardiovascular events. Cochrane Database Syst Rev. 2016 Jan 27;(1):CD011047. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011047.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/26816301?tool=bestpractice.com Gradually increase the dose until onset of side effects. Consider reducing the dose if the patient is unable to tolerate the drug at full initial dose.[63]Markel G, Imazio M, Brucato A, et al. Prevention of recurrent pericarditis with colchicine in 2012. Clin Cardiol. 2013 Mar;36(3):125-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6649517 http://www.ncbi.nlm.nih.gov/pubmed/23404655?tool=bestpractice.com
Primary options
colchicine: <70 kg body weight: 0.5 mg orally once daily for 3 months, then may taper to 0.5 mg once daily on alternate days in the last weeks; ≥70 kg body weight: 0.5 mg orally twice daily for 3 months, then may taper to 0.5 mg once daily in the last weeks
These drug options and doses relate to a patient with no comorbidities.
Primary options
colchicine: <70 kg body weight: 0.5 mg orally once daily for 3 months, then may taper to 0.5 mg once daily on alternate days in the last weeks; ≥70 kg body weight: 0.5 mg orally twice daily for 3 months, then may taper to 0.5 mg once daily in the last weeks
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
colchicine
corticosteroid
Additional treatment recommended for SOME patients in selected patient group
Only consider using a low-dose corticosteroid with specialist guidance from a rheumatologist and a cardiologist.
A corticosteroid is an appropriate option for a small proportion of patients, specifically if:
An infectious cause has been excluded and there is failure of, or contraindication to, NSAIDs and/or colchicine[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
There is a specific indication for use (e.g., the presence of an autoimmune disease). Corticosteroids are used in combination with colchicine in this scenario.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Use corticosteroids at low to moderate doses.[18]Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020 Jan 7;75(1):76-92. https://www.jacc.org/doi/full/10.1016/j.jacc.2019.11.021 http://www.ncbi.nlm.nih.gov/pubmed/31918837?tool=bestpractice.com Continue with the initial dose until symptoms have resolved and the patient’s C-reactive protein level has normalised. Once this is achieved, taper the dose gradually.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Primary options
prednisolone: 0.2 to 0.5 mg/kg/day orally until resolution of symptoms, then gradually taper according to local protocols
These drug options and doses relate to a patient with no comorbidities.
Primary options
prednisolone: 0.2 to 0.5 mg/kg/day orally until resolution of symptoms, then gradually taper according to local protocols
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
prednisolone
exercise restriction
Treatment recommended for ALL patients in selected patient group
Advise the patient to restrict strenuous physical activities:[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [64]Pelliccia A, Solberg EE, Papadakis M, et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2019 Jan 1;40(1):19-33. https://academic.oup.com/eurheartj/article/40/1/19/5248228 http://www.ncbi.nlm.nih.gov/pubmed/30561613?tool=bestpractice.com
Non-athletes: until symptoms have resolved and C-reactive protein has normalised, while also taking into account the patient’s previous history and other clinical conditions[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Athletes: for a minimum of 3 months until symptoms have resolved and C-reactive protein, ECG, and echocardiography have normalised.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
purulent
intravenous antibiotic therapy
Start empirical intravenous antibiotics as soon as you suspect purulent pericarditis. Use an anti-staphylococcal antibiotic plus an aminoglycoside.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com Seek advice from a microbiologist.
Tailor the antibiotics once the underlying pathogens are identified from pericardial fluid and blood cultures.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Continue intravenous antibiotics until fever and clinical signs of infection, including leukocytosis, have resolved.[3]Imazio M, Brucato A, Mayosi BM, et al. Medical therapy of pericardial diseases: part I: idiopathic and infectious pericarditis. J Cardiovasc Med (Hagerstown). 2010 Oct;11(10):712-22. http://www.ncbi.nlm.nih.gov/pubmed/20736783?tool=bestpractice.com
specialist management
Treatment recommended for ALL patients in selected patient group
Specialist management may include pericardiocentesis or surgical pericardial intervention.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
recurrent disease
non-steroidal anti-inflammatory drug (NSAID)
Start an NSAID immediately after diagnosis for symptom management.
Choice of drug is based on patient characteristics (e.g., contraindications, previous efficacy, or side effects), the presence of concomitant diseases (e.g., aspirin is favoured over other NSAIDs if antiplatelet therapy is required), and physician expertise.[18]Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020 Jan 7;75(1):76-92. https://www.jacc.org/doi/full/10.1016/j.jacc.2019.11.021 http://www.ncbi.nlm.nih.gov/pubmed/31918837?tool=bestpractice.com
Practical tip
Aspirin is the preferred NSAID for patients developing pericarditis after a myocardial infarction, or if ischaemic heart disease is a concern.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [39]Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010 Feb 23;121(7):916-28. http://www.ncbi.nlm.nih.gov/pubmed/20177006?tool=bestpractice.com [40]Imazio M, Brucato A, Trinchero R, et al. Diagnosis and management of pericardial diseases. Nat Rev Cardiol. 2009 Dec;6(12):743-51. http://www.ncbi.nlm.nih.gov/pubmed/19859068?tool=bestpractice.com
Continue treatment until symptoms resolve and C-reactive protein has settled.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com Taper drug therapy gradually according to the patient’s symptoms and their C-reactive protein level.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
NSAIDs reduce fever, chest pain, and inflammation but do not prevent tamponade, constriction, or recurrent pericarditis.[39]Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010 Feb 23;121(7):916-28. http://www.ncbi.nlm.nih.gov/pubmed/20177006?tool=bestpractice.com [40]Imazio M, Brucato A, Trinchero R, et al. Diagnosis and management of pericardial diseases. Nat Rev Cardiol. 2009 Dec;6(12):743-51. http://www.ncbi.nlm.nih.gov/pubmed/19859068?tool=bestpractice.com
Primary options
aspirin: 750-1000 mg orally every 8 hours for 1-2 weeks, then decrease by 250-500 mg/dose every 1-2 weeks
OR
ibuprofen: 600 mg orally every 8 hours for 1-2 weeks, then decrease by 200-400 mg/dose every 1-2 weeks
proton-pump inhibitor
Treatment recommended for ALL patients in selected patient group
Due to the high doses of NSAIDs used, give a proton-pump inhibitor (e.g., omeprazole) alongside NSAID therapy to protect against gastrointestinal ulcer formation.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [11]Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004 Nov 18;351(21):2195-202. http://www.ncbi.nlm.nih.gov/pubmed/15548780?tool=bestpractice.com [13]Little WC, Freeman GL. Pericardial disease. Circulation. 2006 Mar 28;113(12):1622-32. http://circ.ahajournals.org/cgi/content/full/113/12/1622 http://www.ncbi.nlm.nih.gov/pubmed/16567581?tool=bestpractice.com [39]Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010 Feb 23;121(7):916-28. http://www.ncbi.nlm.nih.gov/pubmed/20177006?tool=bestpractice.com [40]Imazio M, Brucato A, Trinchero R, et al. Diagnosis and management of pericardial diseases. Nat Rev Cardiol. 2009 Dec;6(12):743-51. http://www.ncbi.nlm.nih.gov/pubmed/19859068?tool=bestpractice.com
Primary options
omeprazole: 20 mg orally once daily
Plus – colchicine (unless the patient has TB pericarditis)
colchicine (unless the patient has TB pericarditis)
Treatment recommended for ALL patients in selected patient group
Add colchicine, unless the patient has tuberculosis pericarditis.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [61]Andreis A, Imazio M, Casula M, et al. Colchicine efficacy and safety for the treatment of cardiovascular diseases. Intern Emerg Med. 2021 Sep;16(6):1691-700. https://www.doi.org/10.1007/s11739-021-02654-7 http://www.ncbi.nlm.nih.gov/pubmed/33704674?tool=bestpractice.com Continue colchicine for 6 months in patients with recurrent disease.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Colchicine is crucial to reduce recurrences, improve response, and increase remission rates.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
If indicated, consider a longer duration of treatment with colchicine according to the patient’s clinical response.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Use colchicine with caution in patients with renal and hepatic impairment because it may be contraindicated with certain medications. A dose reduction may be required.
In practice, avoid colchicine where possible in patients who are very frail or have impaired mobility, due to the high likelihood of treatment-related diarrhoea.
Before commencing treatment, order a baseline full blood count because colchicine may cause neutropenia and bone marrow suppression.
Primary options
colchicine: <70 kg body weight: 0.5 mg orally once daily for 3 months, then may taper to 0.5 mg once daily on alternate days in the last weeks; ≥70 kg body weight: 0.5 mg orally twice daily for 3 months, then may taper to 0.5 mg once daily in the last weeks
treatment of the underlying cause
Treatment recommended for ALL patients in selected patient group
Treat the underlying cause if known. Pericarditis can be caused by:
Tuberculosis (a common cause in the developing world)
Secondary immune processes (e.g., rheumatic fever, post-cardiotomy syndrome, post-myocardial infarction syndrome)
Metabolic disorders (e.g., uraemia, myxoedema), radiotherapy
Cardiac surgery
Percutaneous cardiac interventions
Systemic autoimmune disorders (e.g., rheumatoid arthritis, systemic sclerosis, reactive arthritis, familial Mediterranean fever, systemic vasculitides, inflammatory bowel disease)
Bacterial/fungal/parasitic infections
Trauma
Certain drugs (e.g., hydralazine, antineoplastic drugs, clozapine, tumour necrosis factor-alpha inhibitors, phenytoin)[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Neoplasms.
Seek specialist advice as needed.
If the patient has tuberculous pericarditis, first-line treatment is 4 to 6 weeks of antituberculous therapy.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
When tuberculous pericarditis is confirmed in a non-endemic area, a suitable 6-month regimen is effective; empirical therapy is not required in the absence of an established diagnosis in non-endemic areas.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Adjunctive therapy with corticosteroids and immunotherapy has not been shown to be beneficial.[66]Mayosi BM, Ntsekhe M, Bosch J, et al. Prednisolone and Mycobacterium indicus pranii in tuberculous pericarditis. N Engl J Med. 2014 Sep 18;371(12):1121-30. http://www.nejm.org/doi/full/10.1056/NEJMoa1407380#t=article http://www.ncbi.nlm.nih.gov/pubmed/25178809?tool=bestpractice.com However, corticosteroids may be considered for a patient with tuberculous pericarditis who is HIV-negative.[68]Wiysonge CS, Ntsekhe M, Thabane L, et al. Interventions for treating tuberculous pericarditis. Cochrane Database Syst Rev. 2017 Sep 13;(9):CD000526. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000526.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/28902412?tool=bestpractice.com [
 ]
What are the benefits and harms of steroids for people with tuberculous pericarditis?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1937/fullShow me the answer
]
What are the benefits and harms of steroids for people with tuberculous pericarditis?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1937/fullShow me the answer Pericardiectomy is recommended if the patient does not improve or is deteriorating after 4 to 8 weeks of antituberculosis therapy.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Most patients with uraemic pericarditis respond to intensive dialysis within 1 to 2 weeks.
Autoimmune disorders are treated with corticosteroids and/or another immunosuppressive therapy depending on the specific condition.
Patients developing pericarditis after a myocardial infarction are treated with high-dose aspirin.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com If high-dose aspirin is not effective, paracetamol or an opioid analgesic should be considered.[58]Lilly LS. Treatment of acute and recurrent idiopathic pericarditis. Circulation. 2013 Apr 23;127(16):1723-6. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.111.066365 http://www.ncbi.nlm.nih.gov/pubmed/23609551?tool=bestpractice.com
Treatment of neoplasms may involve any combination of radiotherapy, chemotherapy, or surgery depending on the type of tumour identified.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [39]Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010 Feb 23;121(7):916-28. http://www.ncbi.nlm.nih.gov/pubmed/20177006?tool=bestpractice.com [40]Imazio M, Brucato A, Trinchero R, et al. Diagnosis and management of pericardial diseases. Nat Rev Cardiol. 2009 Dec;6(12):743-51. http://www.ncbi.nlm.nih.gov/pubmed/19859068?tool=bestpractice.com
exercise restriction
Treatment recommended for ALL patients in selected patient group
Advise the patient to restrict strenuous physical activities:[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [64]Pelliccia A, Solberg EE, Papadakis M, et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2019 Jan 1;40(1):19-33. https://academic.oup.com/eurheartj/article/40/1/19/5248228 http://www.ncbi.nlm.nih.gov/pubmed/30561613?tool=bestpractice.com
Non-athletes: until symptoms have resolved and C-reactive protein has normalised, while also taking into account the patient’s previous history and other clinical conditions[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Athletes: for a minimum of 3 months until symptoms have resolved and C-reactive protein, ECG, and echocardiography have normalised.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
corticosteroid
Additional treatment recommended for SOME patients in selected patient group
If the patient does not respond completely to an NSAID plus colchicine, revisit the diagnosis of pericarditis and ensure other causes are ruled out. If there is ongoing inflammation on computed tomography/magnetic resonance imaging, seek advice from a rheumatologist to consider adding a corticosteroid at a low to moderate dose.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Avoid corticosteroids if infections, particularly bacterial infections and tuberculosis, cannot be excluded.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
In general, restrict corticosteroid use to patients with specific indications (including systemic inflammatory diseases, post-cardiotomy syndromes, and pregnancy), NSAID contraindications (true allergy, recent peptic ulcer or gastrointestinal bleeding, oral anticoagulant therapy when the bleeding risk is considered high or unacceptable) or intolerance, or persistent disease despite appropriate doses.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Continue the initial dose until symptoms have resolved and the C-reactive protein level has normalised. Once this is achieved, taper the dose gradually.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
Primary options
prednisolone: 0.2 to 0.5 mg/kg/day orally until resolution of symptoms, then gradually taper according to local protocols
immunosuppressant
Additional treatment recommended for SOME patients in selected patient group
Alternative therapies for recurrent pericarditis are immunosuppressants – including intravenous immunoglobulin, interleukin-1 inhibitors (e.g., anakinra), and azathioprine – but these should only be started by a rheumatologist.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [20]Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA. 2015 Oct 13;314(14):1498-506. https://iris.unito.it/handle/2318/1576078#.XAFHbdv7S70 http://www.ncbi.nlm.nih.gov/pubmed/26461998?tool=bestpractice.com [59]Galluzzo A, Imazio M. Advances in medical therapy for pericardial diseases. Expert Rev Cardiovasc Ther. 2018 Sep;16(9):635-43. http://www.ncbi.nlm.nih.gov/pubmed/30103638?tool=bestpractice.com [69]Vianello F, Cinetto F, Cavraro M, et al. Azathioprine in isolated recurrent pericarditis: a single centre experience. Int J Cardiol. 2011 Mar 17;147(3):477-8. http://www.ncbi.nlm.nih.gov/pubmed/21296434?tool=bestpractice.com [70]Lazaros G, Vasileiou P, Koutsianas C, et al. Anakinra for the management of resistant idiopathic recurrent pericarditis. Initial experience in 10 adult cases. Ann Rheum Dis. 2014 Dec;73(12):2215-7. http://www.ncbi.nlm.nih.gov/pubmed/25165036?tool=bestpractice.com [71]Lazaros G, Imazio M, Brucato A, et al. Anakinra: an emerging option for refractory idiopathic recurrent pericarditis: a systematic review of published evidence. J Cardiovasc Med (Hagerstown). 2016 Apr;17(4):256-62. http://www.ncbi.nlm.nih.gov/pubmed/26090915?tool=bestpractice.com [72]Imazio M, Lazaros G, Picardi E, et al. Intravenous human immunoglobulins for refractory recurrent pericarditis: a systematic review of all published cases. J Cardiovasc Med (Hagerstown). 2016 Apr;17(4):263-9. http://www.ncbi.nlm.nih.gov/pubmed/26090917?tool=bestpractice.com [73]Imazio M, Lazaros G, Brucato A, et al. Recurrent pericarditis: new and emerging therapeutic options. Nat Rev Cardiol. 2016 Feb;13(2):99-105. http://www.ncbi.nlm.nih.gov/pubmed/26259934?tool=bestpractice.com [74]Emmi G, Urban ML, Imazio M, et al. Use of interleukin-1 blockers in pericardial and cardiovascular diseases. Curr Cardiol Rep. 2018 Jun 14;20(8):61. http://www.ncbi.nlm.nih.gov/pubmed/29904899?tool=bestpractice.com [75]Imazio M, Lazaros G, Gattorno M, et al. Anti-interleukin-1 agents for pericarditis: a primer for cardiologists. Eur Heart J. 2022 Aug 14;43(31):2946-57. http://www.ncbi.nlm.nih.gov/pubmed/34528670?tool=bestpractice.com
Primary options
azathioprine: consult specialist for guidance on dose
OR
anakinra: consult specialist for guidance on dose
OR
normal immunoglobulin human: consult specialist for guidance on dose
pericardiectomy
Additional treatment recommended for SOME patients in selected patient group
Pericardiectomy can be considered if the patient has persistent symptomatic recurrent pericarditis (particularly where constriction is present, e.g., following cardiac surgery or radiotherapy), but is a significant and invasive procedure which should be carried out only after careful consideration by the multidisciplinary team including a full evaluation of risks and benefits.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com [53]Kumar S, Khubber S, Reyaldeen R, et al. Advances in imaging and targeted therapies for recurrent pericarditis: a review. JAMA Cardiol. 2022 Sep 1;7(9):975-85. http://www.ncbi.nlm.nih.gov/pubmed/35976625?tool=bestpractice.com [76]Tzani A, Doulamis IP, Tzoumas A, et al. Meta-analysis of population characteristics and outcomes of patients undergoing pericardiectomy for constrictive pericarditis. Am J Cardiol. 2021 May 1;146:120-7. http://www.ncbi.nlm.nih.gov/pubmed/33539860?tool=bestpractice.com Operative mortality is high.[77]Szabó G, Schmack B, Bulut C, et al. Constrictive pericarditis: risks, aetiologies and outcomes after total pericardiectomy: 24 years of experience. Eur J Cardiothorac Surg. 2013 Dec;44(6):1023-8. https://academic.oup.com/ejcts/article/44/6/1023/520799 http://www.ncbi.nlm.nih.gov/pubmed/23761416?tool=bestpractice.com
Pericardiectomy is also indicated if a patient has tuberculous pericarditis with recurrent effusions or evidence of constrictive physiology despite medical therapy.[3]Imazio M, Brucato A, Mayosi BM, et al. Medical therapy of pericardial diseases: part I: idiopathic and infectious pericarditis. J Cardiovasc Med (Hagerstown). 2010 Oct;11(10):712-22. http://www.ncbi.nlm.nih.gov/pubmed/20736783?tool=bestpractice.com See Extrapulmonary tuberculosis.
Pericardiectomy is particularly recommended if the patient’s condition is not improving or is deteriorating after 4 to 8 weeks of antituberculosis therapy.
Standard antituberculosis drugs for 6 months are recommended for the prevention of tuberculous pericardial constriction.[1]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015 Nov 7;36(42):2921-64. https://academic.oup.com/eurheartj/article/36/42/2921/2293375 http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Pericardiectomy in a 56-year-old male patient with idiopathic calcific constrictive pericarditis. The pericardium is thickened and calcifiedPatanwala I, Crilley J, Trewby PN. BMJ Case Reports 2009; doi:10.1136/bcr.06.2008.0015 [Citation ends].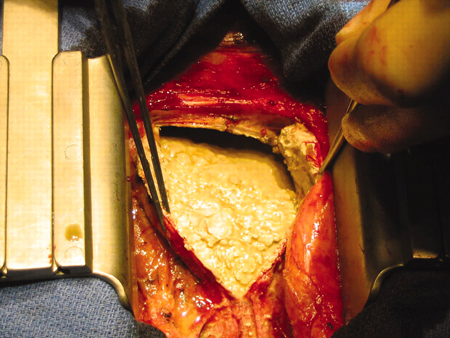

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer
