Investigations
1st investigations to order
ECG
Test
Perform an ECG in any patient with suspected acute pericarditis.[1]
Typical ECG changes occur in up to 60% of patients.[1]
The classic ECG changes are:
Global upwardly concave (saddle shaped) ST-segment (J-point) elevations with PR-segment depressions in most leads[45]
J-point depression and PR elevation in leads aVR and V1.
If the patient is seen soon after symptom onset, PR depressions may be noted prior to ST elevation.
The ECG may evolve over 4 phases: stage 1 consists of ST elevation and upright T waves that may resolve to normal (stage 2) over a period of several days or evolve further to T-wave inversion (stage 3) and then to normal (stage 4).
[Figure caption and citation for the preceding image starts]: ECG in a patient with acute pericarditis, showing diffuse ST-segment elevation in the precordial leads. There is also PR-segment depression in leads V2-V6 (arrows)Rathore S, Dodds PA. BMJ Case Reports 2009; doi:10.1136/bcr.2006.097071 [Citation ends].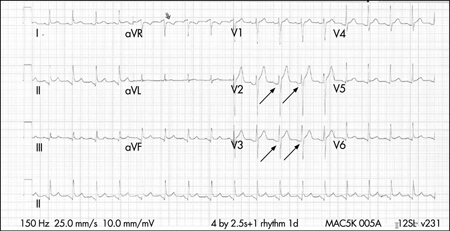
Be aware of the ECG signs of cardiac tamponade, a life-threatening complication of pericarditis. These include:
Low voltage, electrical alternans
Electromechanical dissociation (associated with end-stage tamponade).
See Cardiac tamponade.
Result
upwards concave ST-segment elevation globally with PR depressions in most leads; J-point depression and PR elevation in leads aVR and V1
serum troponin
Test
Order a troponin in any patient with suspected pericarditis.[1]
Serial troponin measurement may be necessary in some patients.[47] However, a patient may not require this if the initial troponin is negative and diagnosis of pericarditis is clear.[47]
Elevated levels may be present in 35% to 50% of patients with pericarditis and reflect myocardial involvement (myopericarditis).[56] However, this test is not specific or sensitive.
The level of elevation correlates with the extent of ST-segment elevation and can be in the range considered diagnostic of acute myocardial infarction in some patients. Elevated levels do not appear to confer prognostic significance. Levels return to normal within 1 to 2 weeks of diagnosis (often within days).
Result
elevation indicates myopericarditis or other aetiologies such as acute coronary syndrome[56]
pericardiocentesis
Test
If you suspect cardiac tamponade, a life-threatening complication of pericarditis, get help immediately from a senior colleague; these patients require urgent pericardiocentesis.[1]
Other indications for pericardiocentesis include suspected purulent pericarditis, high suspicion of neoplastic pericarditis, or a large or symptomatic pericardial effusion in a patient with non-purulent pericarditis.[1]
Send pericardial fluid for analysis, which should include testing for bacterial, fungal, autoimmune, and tuberculous causes, and protein content and microscopy/cytology:[1]
Tuberculous pericarditis: diagnostic accuracy can be improved with identification of the organism from pericardial fluid.[49][50][57] Adenosine deaminase activity within the pericardial effusion may also aid in the diagnosis as an adjunctive marker[1][51]
Viral pericarditis: consider a comprehensive work-up of histological, cytological, immunohistological, and molecular investigations in pericardial fluid for definitive diagnosis[1]
Neoplastic pericarditis: obtain cytological analysis of pericardial fluid for confirmation of malignant pericardial disease.[1]
Result
acid-fast bacilli, positive culture of Mycobacterium tuberculosis
transudate or exudate
C-reactive protein
serum urea and electrolytes
Test
Elevated levels of urea (particularly >21.4 mmol/L [>60 mg/dL]) suggest a uraemic cause.[14]
Result
elevated >21.4 mmol/L (>60 mg/dL) in renal failure
full blood count
liver function tests
Test
Liver congestion may be present if the patient is developing cardiac tamponade.[46]
Result
elevated with liver congestion
chest x-ray
Test
Order a chest x-ray for any patient with suspected acute pericarditis.[1]
Chest x-ray is usually normal, unless a large pericardial effusion (>300 mL) is present, in which case the cardiothoracic ratio will be increased.[1]
Classic flask-shaped heart in large pericardial effusion
Chest x-ray can also demonstrate pleuropericardial disease, signs of heart failure (if there is an indolent onset), concomitant lung pathology providing evidence of tuberculosis, fungal disease, pneumonia, or neoplasm that may be related to the disease.
Result
normal, increased cardiothoracic ratio (if large pericardial effusion is present)
echocardiography
Test
Organise transthoracic echocardiography for any patient with suspected acute pericarditis. If you suspect cardiac tamponade, a life-threatening complication of pericarditis, this should be performed urgently at the bedside.[1]
The European Society of Cardiology recommends echocardiography in all patients in order to complete a full risk stratification prior to discharge.[1] However, in practice, a patient who is young, fit, and well can be discharged without an echocardiography.
Echocardiography is important in detecting pericardial effusions, which are found in up to 60% of cases and are generally small in size.[1][52] Presence of a pericardial effusion is consistent with acute pericarditis and is one of the criteria for its diagnosis.[1]
Echocardiography can also help differentiate pericarditis from acute coronary syndromes. Global ST elevations in the absence of left ventricular wall motion abnormalities and a trivial pericardial effusion supports the diagnosis of acute pericarditis. However, around 5% of patients with acute pericarditis and myocardial involvement may demonstrate wall motion abnormalities.[1]
Echocardiography is insensitive to pericardial inflammation in dry pericarditis; CT or MRI should be used to detect pericardial inflammation (see below).[52]
[Figure caption and citation for the preceding image starts]: Echocardiogram in a baby with purulent pericarditis, showing a pericardial collection. LV = left ventricle, RV = right ventricleKaruppaswamy V, Shauq A, Alphonso N. BMJ Case Reports 2009; doi:10.1136/bcr.2007.136564 [Citation ends].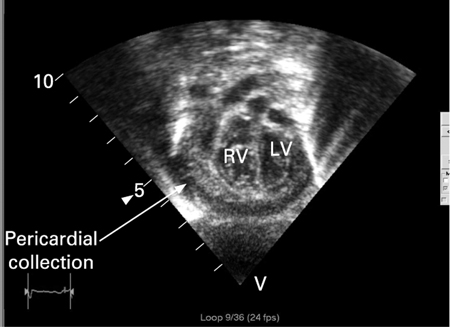
Result
pericardial effusion, absence of left ventricular wall motion abnormalities, thickened and/or bright appearance of pericardium if actively inflamed, evidence of respiratory variation in ventricular filling
Investigations to consider
blood cultures
Test
If you suspect purulent pericarditis and the patient has signs of sepsis, take blood cultures.[1]
Result
positive if infectious cause
erythrocyte sedimentation rate
Test
Elevated erythrocyte sedimentation rate is consistent with an inflammatory state.[1][14]
Serial measurements may be helpful for monitoring disease activity and response to therapy.[1]
In practice, if C-reactive protein is raised, ESR may not be necessary to confirm the presence of inflammation.
Result
may be elevated
creatine kinase
Test
Elevated creatine kinase indicates myocardial injury.
Result
elevated with myocardial injury
autoimmune screen
Test
Order if you suspect an autoimmune cause of pericarditis.
Result
may be positive
viral screen
Test
Order a viral screen (including HIV) if you suspect a viral cause of pericarditis.
Result
may be positive
chest CT or cardiac MRI
Test
Consider chest CT or cardiac MRI especially if the clinical presentation suggests complicated pericarditis or the presentation is atypical.[1][18][52][53]
The key finding in acute pericarditis is pericardial thickening.[18] Pericardial enhancement may be seen on cardiac magnetic resonance late gadolinium enhancement imaging.[54]
CT/MRI may also detect complications such as pericardial effusion or constrictive pericarditis, especially when the echocardiographic findings are inconclusive.[1] MRI is more sensitive for constrictive pericarditis.[18]
Additional diagnostic information may also be obtained when there is associated chest trauma, particularly when penetrating; or in the setting of acute myocardial infarction, carcinoma, pulmonary or thoracic infection, or pancreatitis. In cases of suspected constrictive pericarditis, CT and MRI provide accurate measurements of pericardial thickness and extent of pericardial thickening, which can be helpful for preoperative planning prior to pericardiectomy.
[Figure caption and citation for the preceding image starts]: Chest CT showing a double layer of pericardial calcification in a 56-year-old male patient with idiopathic calcific constrictive pericarditisPatanwala I, Crilley J, Trewby PN. BMJ Case Reports 2009; doi:10.1136/bcr.06.2008.0015 [Citation ends].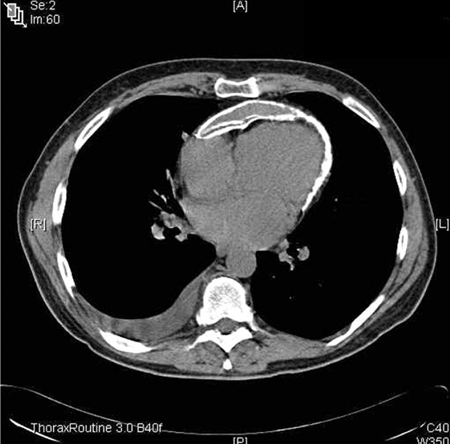 [Figure caption and citation for the preceding image starts]: Chest CT in a baby with purulent pericarditis, showing a pericardial collection with compression of the left (LV) and right (RV) ventriclesKaruppaswamy V, Shauq A, Alphonso N. BMJ Case Reports 2009; doi:10.1136/bcr.2007.136564 [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest CT in a baby with purulent pericarditis, showing a pericardial collection with compression of the left (LV) and right (RV) ventriclesKaruppaswamy V, Shauq A, Alphonso N. BMJ Case Reports 2009; doi:10.1136/bcr.2007.136564 [Citation ends].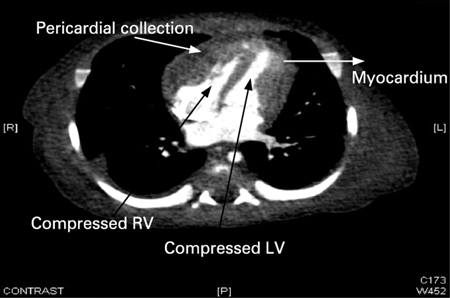
Result
pericardial effusion or constrictive pericarditis (findings include increased pericardial thickness, calcification, abnormal respiratory septal shift or septal bounce), dilatation of the inferior vena cava, and pleural effusions
pericardial oedema on cardiac MRI
pericardial biopsy
Test
In practice, biopsy is rarely required and has been superseded by other specialist investigations, such as cardiac MRI.
Result
may be positive (depending on the underlying cause, such as pericarditis due to tuberculosis, malignant pericardial disease)
Use of this content is subject to our disclaimer