Aetiology
Acute pericarditis can be idiopathic or due to an underlying systemic condition (e.g., systemic lupus erythematosus). As many as 90% of cases are either idiopathic or due to viral infections (e.g., coxsackievirus A9 or B1-4, echovirus, mumps, Epstein-Barr virus, cytomegalovirus, varicella, rubella, HIV, parvovirus-19, SARS-CoV-2).[2][3][5][13][19][20] Onset is frequently post-viral, with no evidence of virus present in the pericardium. Systemic autoimmune disorders (e.g., rheumatoid arthritis, systemic sclerosis, reactive arthritis, familial Mediterranean fever, systemic vasculitides, inflammatory bowel disease) are also a common cause.[21][22] However, there are numerous other less common causes, including bacterial/fungal/parasitic infections, secondary immune processes (e.g., rheumatic fever, post-cardiotomy syndrome, post-myocardial infarction syndrome), pericarditis and pericardial effusions in diseases of surrounding organs (e.g., acute myocardial infarction, myocarditis, paraneoplastic syndromes), metabolic disorders (e.g., uraemia, myxoedema), trauma, neoplasms, and certain drugs (e.g., hydralazine, antineoplastic drugs, clozapine, tumour necrosis factor-alpha inhibitors, phenytoin).[1] Rarely, pericarditis occurs after vaccination (including influenza and mRNA COVID-19 vaccination).[23][24][25][26] Fungal and drug causes are rare.
In developed countries, other causes include radiotherapy, cardiac surgery, percutaneous cardiac interventions, and HIV. Mycobacterium tuberculosis is a common cause in developing countries.[12][14] Pericarditis commonly occurs 1 to 3 days after a myocardial infarction (MI). It can also occur weeks or months later (Dressler's syndrome).[13] Post-cardiac injury syndrome is a broad term that describes pericarditis with or without effusion that results from an MI or iatrogenic injury to the pericardium. It includes post-MI syndrome (Dressler's), post-cardiotomy syndrome, and post-traumatic pericarditis (due to percutaneous coronary intervention or implantable electronic device placement, i.e., pacemaker or defibrillator).[18][27]
Pathophysiology
The pericardium consists of a 2-layered pliable, fibroserous sac that covers the surface of the heart. The inner layer, the visceral pericardium, is adherent to the myocardium. It has a microvillous surface that secretes pericardial fluid. The outer layer, or parietal pericardium, is contiguous with the inner layer. It is composed of collagen layers with interspersed elastin fibrils. Both layers are normally only 1 to 2 mm thick and a space containing 15 to 35 mL of pericardial fluid separates them. The pericardium is perfused by the internal mammary arteries and innervated by the phrenic nerve. The pericardium protects and restrains the heart. In addition, it determines cardiac filling patterns, limits chamber dilatation, and equilibrates compliance between the 2 ventricles.
Signs and symptoms of acute pericarditis result from inflammation of the pericardial tissue. The pericardium is well-innervated and inflammation causes severe pain. Pericarditis can be either fibrinous (dry) or effusive with a purulent, serous, or haemorrhagic exudate. The formation of a concomitant effusion is usually due to a response to the inflammation. The normal pericardium is permeable to water and electrolytes and pericardial fluid is in dynamic equilibrium with the blood serum. Inflamed pericardial tissue impairs this equilibrium. Local production of inflammatory mediators such as cytokines, tumour necrosis factor, and interleukins can cause weeping of fluid from the visceral pericardium, as well as exudation of larger molecules that attract additional fluid and impair resorption.[12][13][28] Constrictive pericarditis impedes normal diastolic filling and can be a medium to late complication of acute pericarditis.[Figure caption and citation for the preceding image starts]: Constrictive pericarditis identified at autopsy; the right section is scar tissue cut from the very front of the heartXu JD, Cao XX, Liu XP, et al. BMJ Case Reports 2009; doi:10.1136/bcr.03.2009.1688 [Citation ends].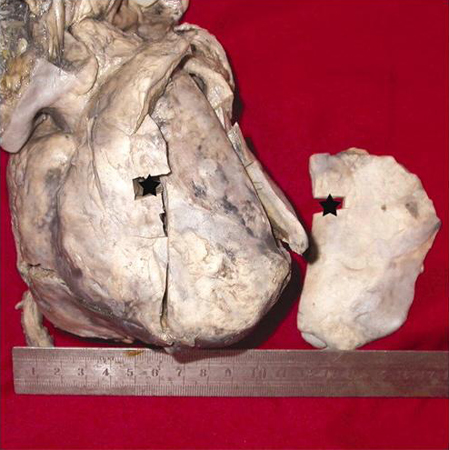
Classification
Clinical classification[1]
Pericarditis can be classified by duration of inflammation as well as by aetiology and complications/sequelae.
A. Acute pericarditis (new onset, <4-6 weeks)
Inflammatory pericardial syndrome associated with at least 2 of the following 4 criteria:
Characteristic chest pain: typically sharp, pleuritic; relieved by sitting forwards and worsened by lying flat
Pericardial friction rub; 'like walking through crunchy snow'
New widespread diffuse concave upwards ST elevation (saddle-shaped) or PR depression on ECG
New or worsening pericardial effusion.
Additional supporting findings include:
Elevated inflammatory markers (i.e., C-reactive protein, erythrocyte sedimentation rate, white blood cell count)
Evidence of pericardial thickening/inflammation by advanced imaging techniques (i.e., cardiac computed tomography or magnetic resonance imaging).
Can be associated with a pericardial effusion that is fibrinous or effusive (serous or serosanguinous).
B. Incessant pericarditis
Signs and symptoms lasting >4 to 6 weeks but <3 months without remission.
C. Recurrent pericarditis
Recurrence of signs and symptoms after an initial documented episode of acute pericarditis with an intervening symptom-free interval of ≥4 to 6 weeks.
D. Chronic pericarditis
Signs and symptoms persisting for >3 months.
Subtypes:
Constrictive (due to chronically thickened pericardium)
Effusive-constrictive (combination of tense effusion in the pericardial space and constriction by the thickened pericardium)
Adhesive (non-constrictive).
Aetiological classification[1][2][3][4][5][6][7][8][9][10]
A. Infectious
Viral
Coxsackievirus A9 or B1-4
Echovirus
Mumps
Epstein-Barr virus
Cytomegalovirus
Varicella
Rubella
HIV
Parvovirus-19
Dengue
Zika
SARS-CoV-2
Bacterial
Pneumococcal
Meningococcal
Gonocococcal
Haemophilus
Chlamydial
Tuberculous
Treponema
Borreliosis
Propionibacteria
Fungal
Candida
Histoplasma
Parasitic
Entamoeba histolytica
Echinococcus
B. Associated with systemic autoimmune disorders
Systemic lupus erythematosus
Rheumatoid arthritis
Systemic sclerosis
Reactive arthritis
Familial Mediterranean fever
Systemic vasculitides
Inflammatory bowel disease
Sarcoidosis
C. Secondary immune process
Rheumatic fever
Post-cardiotomy syndrome
Post-myocardial infarction (MI) syndrome
Post-cardiac ablation or percutaneous coronary intervention
D. Pericarditis and pericardial effusions in diseases of surrounding organs
Acute MI
Myocarditis
Paraneoplastic syndrome
E. Associated with metabolic disorders
Uraemia
Myxoedema
F. Traumatic
Direct injury
Penetrating thoracic injury
Oesophageal perforations
Indirect injury
Non-penetrating thoracic injury
Mediastinal radiation
G. Neoplastic
Primary tumours (rare)
Mesothelioma
Angiosarcoma
Fibrosarcoma
Secondary metastases
Lung carcinoma
Breast carcinoma
Leukaemia and lymphoma
Gastric and colon
Melanoma
Others, including carcinoid
Pericarditis in cancer patients is often non-malignant (e.g., secondary to mediastinal radiation or opportunistic infection)
H. Drug-related
Lupus-like syndrome
Procainamide
Hydralazine
Methyldopa
Isoniazid
Phenytoin
Chemotherapeutic agents (usually with associated cardiomyopathy)
Doxorubicin
Daunorubicin
Cyclophosphamide
Fluorouracil
Cytarabine
Hypersensitivity reaction with eosinophilia
Penicillins
Other
Amiodarone
Thiazides
Sulfa drugs
Ciclosporin
Tumour necrosis factor-alpha inhibitors
Immune checkpoint inhibitors (e.g., CTLA-4 inhibitors, PD-1 inhibitors, and PD-L1 inhibitors)
I. Idiopathic
Idiopathic and viral causes are the most common. Autoimmune disorders are also a common cause. Drugs are a rare cause, and fungi are a very rare cause.
Use of this content is subject to our disclaimer