History and exam
Key diagnostic factors
common
presence of risk factors
Strong risk factors include a family history of hyperlipidaemia or diabetes, a diet high in fat and carbohydrates, insulin resistance, excessive alcohol consumption, overweight/obesity, liver and renal disease, hypothyroidism, HIV, and use of causative medications.
uncommon
eruptive xanthomas
These are characteristic small yellowish papules, frequently surrounded by an erythematous base, that appear predominantly on the buttocks, elbows, and other pressure-sensitive areas. These are caused by deposition of large amounts of chylomicron triglyceride in cutaneous histiocytes in patients with severe HTG.
[Figure caption and citation for the preceding image starts]: Eruptive xanthomasFrom the personal collection of Professor Hegele; used with permission [Citation ends].
lipaemia retinalis
When viewed through the ophthalmoscope, the retina in patients with severe HTG due to chylomicronaemia is pale pink, and the retinal vessels appear white or pink.
[Figure caption and citation for the preceding image starts]: Lipaemia retinalis. Pinkish-white discolouration of retinal blood vessels on ophthalmoscopyFrom the personal collection of Professor Hegele, used with permission [Citation ends].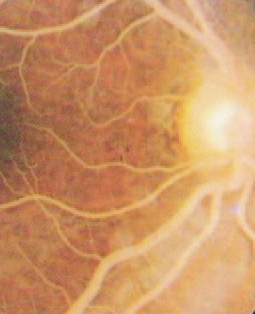
Other diagnostic factors
common
increased BMI/waist circumference
Prevalence of HTG increases with the severity of obesity, which is reflected by increased body mass index.[55] Furthermore, elevated triglyceride (TG) is more common in the setting of abdominal obesity, which is reflected by increased waist circumference, a 'vital sign' to be included with each physical examination.[56]
lipodystrophy
In patients with partial lipodystrophy, characteristic features such as paucity of fat on extremities and gluteal region with preservation of central subcutaneous fat store, acanthosis nigricans and hepatosplenomegaly are present.
features of coronary artery disease
Elevated triglyceride (TG) and TG-rich remnant particles in particular have been implicated as causal factors in the pathogenesis of atherosclerotic cardiovascular disease (ASCVD), such as coronary artery disease and stroke.[23][53] Clinical suspicion for HTG should be raised in patients with unexplained ASCVD.
neurological features
Patients with severe HTG due to chylomicronaemia occasionally have been reported to have confusion ('brain fog'), irritability, difficulty concentrating, and very rarely seizures.
uncommon
recurrent abdominal pain
Abdominal pain in patients with severe HTG due to chylomicronaemia may occur as a result of either pancreatic inflammation or hepatosplenomegaly from fat infiltration. HTG is a strong risk factor for pancreatitis, with 3% to 5% per year incidence for individuals with triglyceride (TG) >10 mmol/L (>885 mg/dL) and an exponential increase in risk with TG >20 mmol/L (>1770 mg/dL). Occasionally, severe vomiting has been observed to cause oesophageal rupture with gastrointestinal bleeding leading to anaemia.[4][52]
Risk factors
strong
family history of hyperlipidaemia
HTG, and especially chylomicronaemia, is often the result of an underlying genetic predisposition, which can be familial (autosomal recessive) or multifactorial (polygenic).[29][30] First-degree obligate heterozygote relatives of patients with familial chylomicronaemia syndrome can have triglyceride levels that range from either normal to mild-to-moderate HTG to severe HTG.[25] Intergenerational inheritance thus appears confusing because a simple dominant genetic model does not apply.[29] In multifactorial severe HTG, which can result from either heterozygous rare variants or accumulated common variants in a polygenic score, the inheritance pattern appears even more erratic and divergent from simple Mendelian rules.[29] HTG tends to cluster in families, although its expression in individual family members does not follow an obvious or classical pattern of segregation. Nonetheless, it is prudent to screen the lipid profile of close family members of an HTG patient.[29]
high saturated fat diet
This type of diet can increase triglyceride production and lead to HTG in predisposed individuals.[31] Monounsaturated fats, such as canola or olive oil, have been suggested as a better alternative to carbohydrates for replacing the calories provided by dietary saturated fats in some patients with HTG. More extreme diets, such as the ketogenic diet, have been shown to exacerbate hyperlipidaemia in certain patients.[32]
high carbohydrate or high glycaemic index diet
This type of diet can increase triglyceride production and lead to HTG in predisposed individuals.[33][34] Monounsaturated fats, such as canola or olive oil, have been suggested as a better alternative to carbohydrates for replacing the calories provided by dietary saturated fats in some patients with HTG. More extreme diets, such as the ketogenic diet, have been shown to exacerbate hyperlipidaemia in certain patients.[32]
excessive alcohol consumption
Excessive ethanol consumption (>1 and >2 units daily, respectively, for women and men), both acutely and chronically, can increase triglyceride production and suppress lipoprotein lipase activity, leading to HTG.[35]
family or personal history of overweight/obesity
Obesity is strongly associated with HTG and also has a strong but complex genetic component, independent of lipoprotein metabolism genes.[5] Elevated triglyceride (TG) is a component of the metabolic syndrome definition.[36] Close family members of a patient with HTG may report a history of obesity or overweight.[37] Weight reduction lowers triglyceride levels.[26]
family or personal history of diabetes
Both mild-to-moderate and severe HTG with chylomicronaemia can result secondarily from poor glycaemic control in patients with either type 1 or 2 diabetes.[21][26] Because both types of diabetes are themselves strongly genetic in nature, close family members of a patient with HTG may report a history of diabetes. Thus, first-degree relatives should be screened for both dyslipidaemia and diabetes.
insulin resistance
liver disease
There is a strong epidemiological and mechanistic relationship between HTG and metabolic dysfunction-associated steatotic liver disease (MASLD)/metabolic dysfunction-associated steatohepatitis (MASH) (previously known as non-alcoholic fatty liver disease and non-alcoholic steatohepatitis, respectively).[38] Triglyceride levels are increased due to overproduction of hepatic very low-density lipoproteins and levels can be improved concurrent with improvement of MASLD/MASH.[38]
renal disease
Nephrotic syndrome is associated with upregulation of production of hepatic apolipoprotein B-containing lipoproteins including very low-density lipoproteins, although total and low-density lipoprotein cholesterol are also increased.[39] Renal toxins in end-stage renal disease can suppress lipoprotein lipase activity, resulting in increased plasma triglyceride levels.[39]
HIV infection
HTG is the commonest lipid disturbance in patients with HIV, and can be very severe on occasion.[40][41] Multiple mechanisms underlie dyslipidaemia in these patients, including direct effects of the virus itself on metabolic pathways, and also the impact of antiretroviral therapy, particularly first-generation protease inhibitors, which can both increase production and impair breakdown of triglyceride-rich lipoprotein particles.[40][41]
use of certain drugs
A wide range of drugs can, through a variety of underlying mechanisms, result in HTG in some, but not all patients.[13] Examples of causative drugs include glucocorticoids, anabolic steroids, oral oestrogens, tamoxifen, thiazide and loop diuretics, non-cardioselective beta-blockers, isotretinoin, bexarotene, propofol, bile acid sequestrants, cyclophosphamide, asparaginase, capecitabine, interferon, tacrolimus, sirolimus, ciclosporin, protease inhibitors, and second-generation antipsychotic agents (e.g., clozapine, olanzapine).[5][13] There is individual variability in susceptibility to HTG secondary to drugs.[29] Certain genetically predisposed patients seem more likely to develop HTG with exposure to drugs associated with HTG.
weak
Cushing syndrome
A risk factor for HTG, mirroring the risk seen with use of exogenous glucocorticoids.[42]
inflammatory/immune disorders
organ transplant
A risk factor for HTG, possibly related to therapeutic use of glucocorticoids and immunosuppression.[46]
hypothyroidism
This is considered to contribute to HTG by reducing triglyceride clearance but is more commonly associated with hypercholesterolaemia.[47]
pregnancy
Plasma triglyceride levels normally increase during pregnancy, and usually this is not severe and does not result in complications. Rarely, severe gestational HTG can result in life-threatening complications including acute pancreatitis, hyperviscosity syndrome, and possibly pre-eclampsia.[48]
Use of this content is subject to our disclaimer