Approach
Patients may present with features of the underlying cause of the hemolytic anemia and/or with signs of anemia such as fatigue, shortness of breath, and dizziness.[37] Association of symptoms with exposure to cold may suggest presence of cold agglutinins.
History
Full history should be taken, including a complete drug history to ascertain whether there is a drug-induced etiology. Ascertaining the time of onset may narrow the differential diagnosis. For example, an acute onset would indicate an acquired cause, whereas chronicity points more toward an inherited cause.
Physical exam
Exam may show signs of anemia, jaundice, or splenomegaly, but there are no signs specific to the condition.
Physical findings of the underlying causes are diverse and include generalized lymphadenopathy in cases of lymphoproliferative disease (chronic lymphocytic leukemia and non-Hodgkin lymphoma); specific cutaneous and joint signs in autoimmune disease (systemic lupus erythematosus [SLE], rheumatoid arthritis); fever in infectious causes; elevated blood pressure in a pregnant patient with preeclampsia or HELLP syndrome (hemolysis, elevated liver enzymes, low platelet count); and skeletal deformities in sickle cell anemia or thalassemia, due to increases in hematopoiesis and bone expansion during childhood.
Laboratory tests to determine the presence of hemolysis
The initial tests to perform are a complete blood count and comprehensive metabolic panel. Anemia with an increased mean corpuscular hemoglobin concentration is usually present in hemolysis (due to the increased corpuscular volume of reticulocytes). Red blood cell (RBC) destruction and release of hemoglobin results in an elevated lactate dehydrogenase and unconjugated bilirubin. Urinalysis will show hemoglobinuria in cases of intravascular hemolysis. Haptoglobin should be requested and will be low if hemolysis is present.
A peripheral blood smear is then required to confirm the presence of reticulocytes, and it will also provide differentiating information as to the cause of hemolysis. The presence of schistocytes suggests a microangiopathic process (disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, HELLP syndrome) or traumatic process (prosthetic heart valve, footstrike [march] hemolysis) as a cause. Spherocytes and elliptocytes may indicate hereditary spherocytosis and elliptocytosis. Blister or bite cells indicate the presence of oxidative damage to the cell. Spur cells are present in liver disease. RBC inclusions may be seen in infections such as malaria, babesiosis, and Bartonella infections. [Figure caption and citation for the preceding image starts]: Photomicrograph revealing the presence of what were determined to be numbers of intraerythrocytic Babesia sp. ring-form parasitesCDC/ Dr Mae Melvin [Citation ends].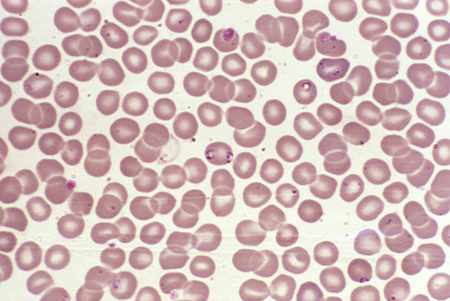 [Figure caption and citation for the preceding image starts]: A photomicrograph of a blood smear showing erythrocytes containing developing Plasmodium vivax parasitesCDC/ Dr Mae Melvin [Citation ends].
[Figure caption and citation for the preceding image starts]: A photomicrograph of a blood smear showing erythrocytes containing developing Plasmodium vivax parasitesCDC/ Dr Mae Melvin [Citation ends].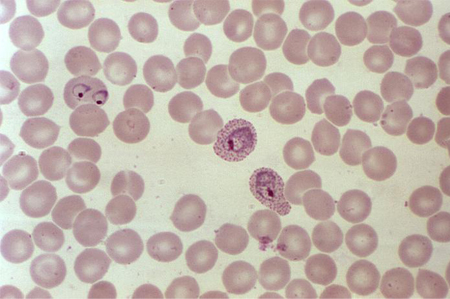
Subsequent testing for specific cause
Should be directed by the suspected diagnosis from clinical evaluation:
A positive direct antiglobulin test (Coombs) indicates the presence of immune causes of hemolytic anemia. The basic direct antiglobulin test typically detects autoantibodies to IgG and complement (C3d).[37][38]
Paroxysmal cold hemoglobinuria is diagnosed in patients with hemolysis (with direct antiglobulin test usually positive for C3 only) and a positive Donath-Landsteiner test.[37][38][39] False-negative results can be avoided by using an indirect method.[37]
Antinuclear antibody should be requested to evaluate for SLE.
Hb electrophoresis detects hemoglobinopathy. Do not repeat hemoglobin electrophoresis in patients who have a prior result, unless the results of interventional therapies are being monitored or to make a more specific diagnosis.[40]
Testing for glucose-6-phosphate dehydrogenase deficiency includes a fluorescent spot test followed by definitive assay of glucose-6-phosphate dehydrogenase activity by spectrophotometry.
Paroxysmal nocturnal hemoglobinuria is evaluated by flow cytometry for CD55/CD59.
Abnormal renal function in the presence of hemolysis suggests hemolytic uremic syndrome or thrombotic thrombocytopenic purpura.
Elevated liver function tests may indicate liver disease.
How to take a venous blood sample from the antecubital fossa using a vacuum needle.
Use of this content is subject to our disclaimer
