The diagnosis of chancroid is classically based on history, clinical features on physical exam, and isolation of the causative organism with culture.[44]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 2024 Mar 5:ciae104.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
However, it is important to note that clinical features are generally nonspecific, culture of the organism can be difficult, and mixed infections are common. Coinfection with herpes simplex virus (HSV) and syphilis must therefore be excluded in all patients with suspected chancroid.[45]Ndinya-Achola JO, Kihara KN, Fisher LD, et al. Presumptive specific clinical diagnosis of genital ulcer disease (GUD) in a primary health care setting in Nairobi. Int J STD AIDS. 1996 May-Jun;7(3):201-5.
http://www.ncbi.nlm.nih.gov/pubmed/8799783?tool=bestpractice.com
[46]Chapel TA, Brown WJ, Jeffres C, et al. How reliable is the morphological diagnosis of penile ulcerations? Sex Transm Dis. 1977 Oct-Dec;4(4):150-2.
http://www.ncbi.nlm.nih.gov/pubmed/594859?tool=bestpractice.com
[47]Behets FM, Andriamiadana J, Randrianasolo D, et al. Chancroid, primary syphilis, genital herpes, and lymphogranuloma venereum in Antananarivo, Madagascar. J Infect Dis. 1999 Oct;180(4):1382-5.
https://academic.oup.com/jid/article/180/4/1382/846878
http://www.ncbi.nlm.nih.gov/pubmed/10479178?tool=bestpractice.com
[48]Dangor Y, Ballard RC, da L Exposto F, et al. Accuracy of clinical diagnosis of genital ulcer disease. Sex Transm Dis. 1990 Oct-Dec;17(4):184-9.
http://www.ncbi.nlm.nih.gov/pubmed/2175951?tool=bestpractice.com
[49]Behets FM, Liomba G, Lule G, et al. Sexually transmitted diseases and human immunodeficiency virus control in Malawi: a field study of genital ulcer disease. J Infect Dis. 1995 Feb;171(2):451-5.
http://www.ncbi.nlm.nih.gov/pubmed/7844388?tool=bestpractice.com
[50]Htun Y, Morse SA, Dangor Y, et al. Comparison of clinically directed, disease specific, and syndromic protocols for the management of genital ulcer disease in Lesotho. Sex Transm Infect. 1998 Jun;74 Suppl 1:S23-8.
http://www.ncbi.nlm.nih.gov/pubmed/10023349?tool=bestpractice.com
History
A thorough history should be elicited in cases of suspected chancroid covering symptom, sexual, and travel history.
Symptom history
Patients will usually complain of a painful genital ulcer, inguinal tenderness, or, less commonly, purulent discharge. Inguinal tenderness is more common in men. Ulcers may be painless in women, especially if they occur on the vaginal walls or cervix.
Constitutional symptoms such as fever or rash are usually absent.[15]Spinola, SM. Chancroid and Haemophilus ducreyi. In: Holmes KK, Sparling PF, Stamm WE, et al, eds. Sexually transmitted diseases. 4th ed. New York, NY: McGraw-Hill, 2008:689-700. Women may present with more subtle symptoms such as dysuria, vaginal discharge, dyspareunia, hematochezia, or pain on defecation.
Symptoms typically appear 3-7 days after unprotected intercourse with an infected partner.[31]Lautenschlager S, Kemp M, Christensen JJ, et al. 2017 European guideline for the management of chancroid. Int J STD AIDS. 2017 Mar;28(4):324-9.
http://www.ncbi.nlm.nih.gov/pubmed/28081686?tool=bestpractice.com
The time from last sexual activity to symptom onset should be defined. Typically, there is no prodrome. Care is usually sought after the lesions ulcerate or become painful, or other symptoms develop.
Sexual history
Important features include the date of last sexual activity, history of unprotected sex with a person from an endemic region, condom use, contact with sex worker (self or partner), HIV status, history of other sexually transmitted infections, social history including drug and alcohol use, and the presence of any conditions that compromise the immune system.
Travel history
Physical exam
Ulcers usually measure 1-2 cm and have sharply demarcated borders with ragged, undermined edges and a friable base. The base may be covered with a grayish or yellow exudate. Induration is not present.
In men, the majority of ulcers are located on the prepuce or frenulum, or in the coronal sulcus. Less commonly, the glans, penile shaft, meatus, or anus is involved. Complications such as phimosis, urethral fistula, and secondary bacterial infection may also be present.[15]Spinola, SM. Chancroid and Haemophilus ducreyi. In: Holmes KK, Sparling PF, Stamm WE, et al, eds. Sexually transmitted diseases. 4th ed. New York, NY: McGraw-Hill, 2008:689-700.[17]Morse SA. Chancroid and Haemophilus ducreyi. Clin Microbiol Rev. 1989 Apr;2(2):137-57.
http://cmr.asm.org/content/2/2/137.long
http://www.ncbi.nlm.nih.gov/pubmed/2650859?tool=bestpractice.com
[51]Lewis DA. Chancroid: clinical manifestations, diagnosis, and management. Sex Transm Infect. 2003 Feb;79(1):68-71.
http://sti.bmj.com/content/79/1/68.full
http://www.ncbi.nlm.nih.gov/pubmed/12576620?tool=bestpractice.com
Urethral discharge may be seen but is uncommon.
In women, ulcers are usually on the fourchette, labia, vestibule, or clitoris. Larger periurethral ulcers may be present. The vaginal walls and cervix should be inspected, as these lesions are often painless and go unnoticed. Female patients are less likely to develop ulceration. Vaginal discharge may be present and complications such as rectovaginal or urethral fistula may be evident on exam.
Other types of ulcers include giant (>2 cm) or serpiginous ulcers, follicular ulcers, or papules with a raised border that resembles condyloma latum of secondary syphilis. Lesions may be <1 to 5 mm in diameter, resembling HSV lesions, and may form "kissing lesions" on opposing surfaces. Vesicles are not seen. Women are more likely to have spontaneous resolution of papules, whereas men are more likely to progress to the pustular stage.[35]Bong CT, Harezlak J, Katz BP, et al. Men are more susceptible than women to pustule formation in the experimental model of Haemophilus ducreyi infection. Sex Transm Dis. 2002 Feb;29(2):114-8.
http://www.ncbi.nlm.nih.gov/pubmed/11818898?tool=bestpractice.com
[36]Spinola SM, Bong CT, Faber AL, et al. Differences in host susceptibility to disease progression in the human challenge model of Haemophilus ducreyi infection. Infect Immun. 2003 Nov;71(11):6658-63.
http://iai.asm.org/content/71/11/6658.long
http://www.ncbi.nlm.nih.gov/pubmed/14573692?tool=bestpractice.com
Painful inguinal lymphadenitis is often present in about 50% of patients, mostly in men.[52]Ahmed J, Rawre J, Dhawan N, et al. Genital ulcer disease: a review. J Family Med Prim Care. 2022 Aug;11(8):4255-62.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9638565
http://www.ncbi.nlm.nih.gov/pubmed/36352984?tool=bestpractice.com
It is unilateral in approximately two-thirds of cases. In later stages, fluctuant lymphadenitis (buboes) may appear.
Extragenital lesions are rare, usually resulting from autoinoculation and affecting the thighs, fingers, oropharynx, or breast (in women).[15]Spinola, SM. Chancroid and Haemophilus ducreyi. In: Holmes KK, Sparling PF, Stamm WE, et al, eds. Sexually transmitted diseases. 4th ed. New York, NY: McGraw-Hill, 2008:689-700.[51]Lewis DA. Chancroid: clinical manifestations, diagnosis, and management. Sex Transm Infect. 2003 Feb;79(1):68-71.
http://sti.bmj.com/content/79/1/68.full
http://www.ncbi.nlm.nih.gov/pubmed/12576620?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Penile ulcers associated with chancroidAdapted from J. Miller, Public Health Image Library, CDC (1974) [Citation ends]. [Figure caption and citation for the preceding image starts]: Chancroid pustule resembling syphilisAdapted from Public Health Image Library, CDC (1971) [Citation ends].
[Figure caption and citation for the preceding image starts]: Chancroid pustule resembling syphilisAdapted from Public Health Image Library, CDC (1971) [Citation ends]. [Figure caption and citation for the preceding image starts]: Buboes associated with Haemophilus ducreyi infectionAdapted from S. Lindsley, Public Health Image Library, CDC (1971) [Citation ends].
[Figure caption and citation for the preceding image starts]: Buboes associated with Haemophilus ducreyi infectionAdapted from S. Lindsley, Public Health Image Library, CDC (1971) [Citation ends].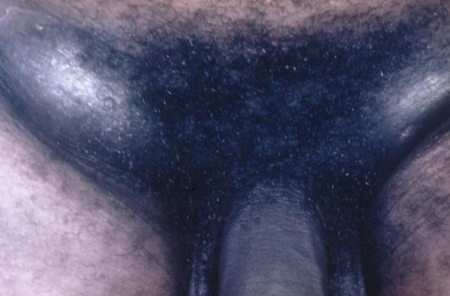
Testing for H ducreyi
The clinical diagnosis of chancroid is confirmed by swabbing genital lesions for culture to isolate H ducreyi colonies.[44]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 2024 Mar 5:ciae104.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
Sample collection should ideally be from the base of the lesion without surface genital skin as swabs from the ulcer base have a higher yield than those from the bubo.[53]British Association for Sexual Health and HIV. Guidance on STI testing, 2021 and 2023. May 2023 [internet publication].
https://www.bashh.org/resources/40/guidelines_guidance_on_sti_testing_2021_and_2023
Any urethral or vaginal discharge should also be swabbed.
Culture
The diagnostic standard for chancroid, in spite of relatively low sensitivity (53% to 92%) and the organism being fastidious and difficult to culture.[54]Dylewski J, Nsanze H, Maitha G, et al. Laboratory diagnosis of Haemophilus ducreyi: sensitivity of culture media. Diagn Microbiol Infect Dis. 1986 Mar;4(3):241-5.
http://www.ncbi.nlm.nih.gov/pubmed/3485507?tool=bestpractice.com
Specialized media are required to optimize growth. The recovery of H ducreyi is improved if culture is attempted in more than 1 type of media (MH-HB and/or GC-HgS). Vancomycin 3 micrograms/mL is added to inhibit growth of other bacteria.
Nucleic acid detection
There are no Food and Drug Administration (FDA)-approved polymerase chain reaction (PCR) tests for H ducreyi available in the US. However, some clinical laboratories have developed their own PCR test and have conducted CLIA verification studies in genital specimens.[55]Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8344968
http://www.ncbi.nlm.nih.gov/pubmed/34292926?tool=bestpractice.com
The sensitivity (98%) and specificity (>90%) for detection of chancroid are better than with other methods.[56]Morse SA, Trees DL, Htun Y, et al. Comparison of clinical diagnosis and standard laboratory and molecular methods for the diagnosis of genital ulcer disease in Lesotho: association with human immunodeficiency virus infection. J Infect Dis. 1997 Mar;175(3):583-9.
http://www.ncbi.nlm.nih.gov/pubmed/9041329?tool=bestpractice.com
[57]Totten PA, Kuypers JM, Chen CY, et al. Etiology of genital ulcer disease in Dakar, Senegal, and comparison of PCR and serologic assays for the detection of Haemophilus ducreyi. J Clin Microbiol. 2000 Jan;38(1):268-73.
http://jcm.asm.org/content/38/1/268.long
http://www.ncbi.nlm.nih.gov/pubmed/10618099?tool=bestpractice.com
[58]Patterson K, Olsen B, Thomas C, et al. Development of a rapid immunodiagnostic test for Haemophilus ducreyi. J Clin Microbiol. 2002 Oct;40(10):3694-702.
http://jcm.asm.org/content/40/10/3694.long
http://www.ncbi.nlm.nih.gov/pubmed/12354868?tool=bestpractice.com
[59]Chui L, Albritton W, Paster B, et al. Development of the polymerase chain reaction for diagnosis of chancroid. J Clin Microbiol. 1993 Mar;31(3):659-64.
http://jcm.asm.org/content/31/3/659.long
http://www.ncbi.nlm.nih.gov/pubmed/8458959?tool=bestpractice.com
Multiplex PCR tests have been developed that allow testing for several organisms simultaneously, including H ducreyi and HSV.[60]Orle KA, Gates CA, Martin DH, et al. Simultaneous PCR detection of Haemophilus ducreyi, Treponema pallidum, and herpes simplex virus types 1 and 2 from genital ulcers. J Clin Microbiol. 1996 Jan;34(1):49-54.
http://jcm.asm.org/content/34/1/49.long
http://www.ncbi.nlm.nih.gov/pubmed/8748271?tool=bestpractice.com
[61]Mackay IM, Harnett G, Jeoffreys N, et al. Detection and discrimination of herpes simplex viruses, Haemophilus ducreyi, Treponema pallidum, and Calymmatobacterium (Klebsiella) granulomatis from genital ulcers. Clin Infect Dis. 2006 May 15;42(10):1431-8.
https://academic.oup.com/cid/article/42/10/1431/278293
http://www.ncbi.nlm.nih.gov/pubmed/16619156?tool=bestpractice.com
These technologies are available primarily at reference labs. Due to the difficulties with culture, PCR should be considered the test of choice where available.[53]British Association for Sexual Health and HIV. Guidance on STI testing, 2021 and 2023. May 2023 [internet publication].
https://www.bashh.org/resources/40/guidelines_guidance_on_sti_testing_2021_and_2023
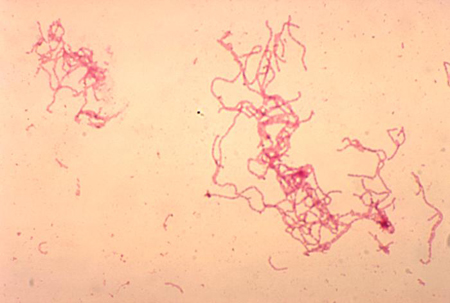
Gram staining
The classic appearance is of gram-negative coccobacilli or slender bacilli in a railroad or chaining pattern. The distinctive "school of fish" arrangement has long parallel columns between cells or long chains of cells. Gram staining is not a reliable finding (sensitivity 5% to 63%; specificity 51% to 99%) because of the polymicrobial flora of most genital ulcers.[62]Lewis DA. Diagnostic tests for chancroid. Sex Transm Infect. 2000 Apr;76(2):137-41.
http://sti.bmj.com/content/76/2/137.long
http://www.ncbi.nlm.nih.gov/pubmed/10858718?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Gram stain of Haemophilus ducreyiAdapted from G. Hammond, Public Health Image Library, CDC (1978) [Citation ends].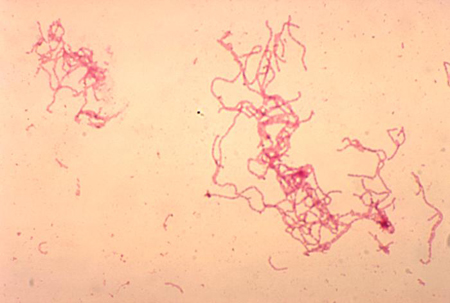
Serology
Additional laboratory investigations
Other tests for H ducreyi
Immunofluorescent detection: direct and indirect immunofluorescent testing of ulcer material has been done to detect H ducreyi. Monoclonal antibodies are designed to detect lipo-oligosaccharide or HbA antigens. However, these assays are not commercially available. Compared with culture, this method has a sensitivity as high as 93% for ulcer specimens, but the specificity is poor (63%).[2]Trees DL, Morse SA. Chancroid and Haemophilus ducreyi: an update. Clin Microbiol Rev. 1995 Jul;8(3):357-75.
http://cmr.asm.org/content/8/3/357.long
http://www.ncbi.nlm.nih.gov/pubmed/7553570?tool=bestpractice.com
Antimicrobial susceptibility testing: this can be done by agar dilution or E-test.[63]Alfa M. The laboratory diagnosis of Haemophilus ducreyi. Can J Infect Dis Med Microbiol. 2005 Jan;16(1):31-4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2095004
http://www.ncbi.nlm.nih.gov/pubmed/18159525?tool=bestpractice.com
It is not used routinely due to difficulty in culturing H ducreyi, lack of standardization, and lack of interpretive guidelines. Studies have shown in vitro resistance to tetracyclines, sulfonamides, penicillins, and amoxicillin/clavulanate. However, the majority of isolates remain susceptible to rifamycins, quinolones, macrolides, and streptomycin.[17]Morse SA. Chancroid and Haemophilus ducreyi. Clin Microbiol Rev. 1989 Apr;2(2):137-57.
http://cmr.asm.org/content/2/2/137.long
http://www.ncbi.nlm.nih.gov/pubmed/2650859?tool=bestpractice.com
[26]Rutanarugsa A, Vorachit M, Polnikorn N, et al. Drug resistance of Haemophilus ducreyi. Southeast Asian J Trop Med Public Health. 1990 Jun;21(2):185-93.
http://www.ncbi.nlm.nih.gov/pubmed/2237585?tool=bestpractice.com
[64]Roy-Leon JE, Lauzon WD, Toye B, et al. In vitro and in vivo activity of combination antimicrobial agents on Haemophilus ducreyi. J Antimicrob Chemother. 2005 Sep;56(3):552-8.
https://academic.oup.com/jac/article/56/3/552/691080
http://www.ncbi.nlm.nih.gov/pubmed/16046468?tool=bestpractice.com
[65]Knapp JS, Back AF, Babst AF, et al. In vitro susceptibilities of isolates of Haemophilus ducreyi from Thailand and from the United States to currently recommended and newer agents for the treatment of chancroid. Antimicrob Agents Chemother. 1993 Jul;37(7):1552-5.
http://aac.asm.org/content/37/7/1552.long
http://www.ncbi.nlm.nih.gov/pubmed/8363390?tool=bestpractice.com
Antimicrobial susceptibility testing is usually reserved for cases in which response to antibiotic therapy is poor.
Investigations to rule out an alternative or comorbid diagnosis
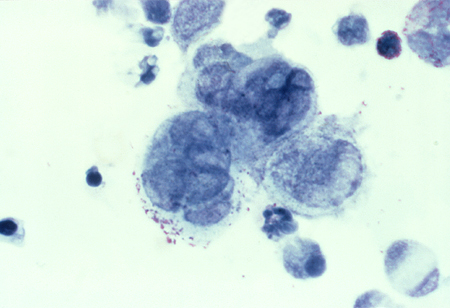
Detection of HSV: PCR or viral culture should be carried out to exclude HSV infection. A Tzanck smear of the biopsy can be used to diagnose HSV in ambiguous cases. It shows the characteristic appearance of multinucleated giant cells and epithelial cells containing eosinophilic intranuclear inclusion bodies. This test is only used if herpes is strongly suspected, and PCR testing and viral cultures are inconclusive.[Figure caption and citation for the preceding image starts]: Tzanck test specimen showing multinucleated giant cells, indicating the presence of herpes virusAdapted from J. Miller, Public Health Image Library, CDC (1975) [Citation ends].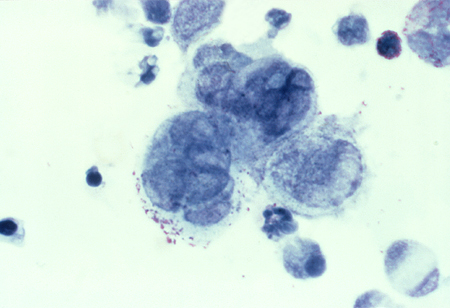 See Herpes simplex virus infection.
See Herpes simplex virus infection.
Detection of Treponema pallidum (syphilis): The most common approach is to use a treponemal test as the initial serologic test, followed by a nontreponemal test to confirm diagnosis and provide evidence of active disease or reinfection (i.e., a "reverse sequence screening algorithm").[66]Papp JR, Park IU, Fakile Y, et al. CDC laboratory recommendations for syphilis testing, United States, 2024. MMWR Recomm Rep. 2024 Feb 8;73(1):1-32.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10849099
http://www.ncbi.nlm.nih.gov/pubmed/38319847?tool=bestpractice.com
However, use of a traditional screening algorithm (initial investigation with a nontreponemal test followed by a treponemal test) is also acceptable. Dark-field microscopy of a lesion swab can provide a definitive diagnosis of syphilis, but it is not usually available outside of specialist settings. See Syphilis infection.
HIV testing: chancroid is an important cofactor in the transmission of HIV; therefore, HIV status should also be assessed as part of the diagnostic workup.[27]Mohammed TT, Olumide YM. Chancroid and human immunodeficiency virus infection--a review. Int J Dermatol. 2008 Jan;47(1):1-8.
https://onlinelibrary.wiley.com/doi/10.1111/j.1365-4632.2007.03435.x
http://www.ncbi.nlm.nih.gov/pubmed/18173591?tool=bestpractice.com
Local guidance for HIV testing varies. See HIV infection.
 [Figure caption and citation for the preceding image starts]: Chancroid pustule resembling syphilisAdapted from Public Health Image Library, CDC (1971) [Citation ends].
[Figure caption and citation for the preceding image starts]: Chancroid pustule resembling syphilisAdapted from Public Health Image Library, CDC (1971) [Citation ends]. [Figure caption and citation for the preceding image starts]: Buboes associated with Haemophilus ducreyi infectionAdapted from S. Lindsley, Public Health Image Library, CDC (1971) [Citation ends].
[Figure caption and citation for the preceding image starts]: Buboes associated with Haemophilus ducreyi infectionAdapted from S. Lindsley, Public Health Image Library, CDC (1971) [Citation ends].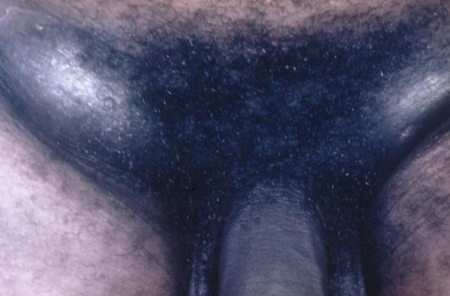
 See Herpes simplex virus infection.
See Herpes simplex virus infection.