Around 90% of infections are asymptomatic or result in a mild influenza-like illness.[11]Centers for Disease Control and Prevention. CDC Yellow Book 2024: travel associated infections and diseases. Section 5: Histoplasmosis. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/histoplasmosis
For immunocompetent patients with mild flu-like symptoms, in the appropriate epidemiologic setting, the diagnosis of histoplasmosis may be obvious.
For other patients presenting with more persistent respiratory symptoms or for immunocompromised patients however, comprehensive evaluation that includes history, physical exam, and assessment of clinical, radiologic, and laboratory evidence of dissemination should be sought.
History
A thorough social and occupational history should be obtained. Histoplasma capsulatum is endemic to the Ohio, Mississippi, and Missouri River valleys in the US, as well as to Central and South America.[3]Cano MV, Hajjeh RA. The epidemiology of histoplasmosis: a review. Semin Respir Infect. 2001 Jun;16(2):109-18.
http://www.ncbi.nlm.nih.gov/pubmed/11521243?tool=bestpractice.com
[4]Thompson GR 3rd, Le T, Chindamporn A, et al. Global guideline for the diagnosis and management of the endemic mycoses: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology. Lancet Infect Dis. 2021 Dec;21(12):e364-74.
http://www.ncbi.nlm.nih.gov/pubmed/34364529?tool=bestpractice.com
[16]Mata-Essayag S, Colella MT, Rosello A, et al. Histoplasmosis: a study of 158 cases in Venezuela, 2000-2005. Medicine (Baltimore). 2008 Jul;87(4):193-202.
http://www.ncbi.nlm.nih.gov/pubmed/18626302?tool=bestpractice.com
Cave exploring, close proximity to bird roosts or bats, demolition and excavation, and gathering and cutting wood are all associated with infection. This information will assist in establishing the amount of exposure to the fungal spores, although an exposure history is not always present in affected individuals. In light of increasing spread of this organism outside its current geographic boundaries, a diagnosis of histoplasmosis should be considered in the appropriate clinical context even in the absence of a typical travel history.[6]Mazi PB, Sahrmann JM, Olsen MA, et al. The Geographic Distribution of Dimorphic Mycoses in the United States for the Modern Era. Clin Infect Dis. 2022 Nov 11 [Epub ahead of print].
http://www.ncbi.nlm.nih.gov/pubmed/36366776?tool=bestpractice.com
The patient may have a drug history or comorbid condition that may contribute to an immunocompromised state.
The patient may have an underlying lung disease (e.g., emphysema). Chronic lung disease is a risk factor for the development of chronic pulmonary histoplasmosis.[26]Wheat LJ, Wass J, Norton J, et al. Cavitary histoplasmosis occurring during two large urban outbreaks. Analysis of clinical, epidemiologic, roentgenographic, and laboratory features. Medicine (Baltimore). 1984 Jul;63(4):201-9.
http://www.ncbi.nlm.nih.gov/pubmed/6738342?tool=bestpractice.com
[27]Wheat LJ, Conces D, Allen SD, et al. Pulmonary histoplasmosis syndromes: recognition, diagnosis, and management. Semin Respir Crit Care Med. 2004 Apr;25(2):129-44.
http://www.ncbi.nlm.nih.gov/pubmed/16088457?tool=bestpractice.com
Because of its high morbidity and mortality, the possibility of disseminated fungal infection should be considered early in the disease course of patients with underlying impaired cellular immunity (e.g., AIDS/HIV infection, chronic immunosuppressive therapy such as tumor necrosis factor (TNF)-alpha antagonists and corticosteroids), neutropenia, age <2 years, chronic lung disease, and graft-versus-host disease, as well as stem cell and solid organ transplant recipients.[19]Schwartz RS, Mackintosh FR, Schrier SL, et al. Multivariate analysis of factors associated with invasive fungal disease during remission induction therapy for acute myelogenous leukemia. Cancer. 1984 Feb 1;53(3):411-9.
http://www.ncbi.nlm.nih.gov/pubmed/6581852?tool=bestpractice.com
[20]Assi M, Martin S, Wheat LJ, et al. Histoplasmosis after solid organ transplant. Clin Infect Dis. 2013 Dec;57(11):1542-9.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3814825
http://www.ncbi.nlm.nih.gov/pubmed/24046304?tool=bestpractice.com
[21]Kauffman CA, Freifeld AG, Andes DR, et al. Endemic fungal infections in solid organ and hematopoietic cell transplant recipients enrolled in the Transplant-Associated Infection Surveillance Network (TRANSNET). Transpl Infect Dis. 2014 Apr;16(2):213-24.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5664161
http://www.ncbi.nlm.nih.gov/pubmed/24589027?tool=bestpractice.com
Physical exam
Latent asymptomatic pulmonary histoplasmosis
Acute respiratory histoplasmosis (symptoms <4 weeks)
Patients present with flu-like symptoms (e.g., fever, headache, malaise, abdominal pain, weight loss, dry or nonproductive cough, chest pain, fatigue, arthralgias).[1]Wheat LJ, Freifeld AG, Kleiman MB, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007 Oct 1;45(7):807-25.
https://academic.oup.com/cid/article/45/7/807/541502
http://www.ncbi.nlm.nih.gov/pubmed/17806045?tool=bestpractice.com
Findings on examination are usually unremarkable. Chest auscultation may be normal; scattered crackles and bronchial breathing may be heard in some patients.
Acute respiratory histoplasmosis (symptoms >4 weeks)
Symptoms persisting for >4 weeks may indicate that the patient is developing progressive disseminated disease, which may be arrested by effective therapy.
In patients with more severe respiratory symptoms, distant breath sounds may be heard during auscultation over a lung cavity.
Chronic pulmonary histoplasmosis
This occurs in patients with underlying lung disease (e.g., emphysema).
Infiltration of the upper lobes of one or both lungs can occur with cavitation.
The most common manifestations are productive cough, weight loss, fevers, malaise, and possibly hemoptysis.
Chronic pulmonary disease resembles tuberculosis and can worsen over months or years.
Mediastinal histoplasmosis
Results from involvement of mediastinal lymph nodes, which coalesce to form mass-like lesions.
Often asymptomatic, though symptoms can result from impingement on mediastinal structures such as the esophagus and bronchus.
Fibrosis of the mediastinum can occur as a late complication in some patients, with associated invasion of vital structures.
Disseminated histoplasmosis
Occurs primarily in immunocompromised patients, especially in patients with HIV infection.[1]Wheat LJ, Freifeld AG, Kleiman MB, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007 Oct 1;45(7):807-25.
https://academic.oup.com/cid/article/45/7/807/541502
http://www.ncbi.nlm.nih.gov/pubmed/17806045?tool=bestpractice.com
Impaired cellular immunity from primary immunodeficiency, or secondary to TNF-alpha antagonists or immunosuppressive therapy, increases the risk of progressive, disseminated, life-threatening histoplasmosis.[14]Deepe GS Jr. Modulation of infection with Histoplasma capsulatum by inhibition of tumor necrosis factor-alpha activity. Clin Infect Dis. 2005 Aug 1;41(suppl 3):S204-7.
https://academic.oup.com/cid/article/41/Supplement_3/S204/369190
http://www.ncbi.nlm.nih.gov/pubmed/15983901?tool=bestpractice.com
[18]Wallis RS, Broder M, Wong J, et al. Reactivation of latent granulomatous infections by infliximab. Clin Infect Dis. 2005 Aug 1;41(suppl 3):S194-8.
https://academic.oup.com/cid/article/41/Supplement_3/S194/368817
http://www.ncbi.nlm.nih.gov/pubmed/15983899?tool=bestpractice.com
Fever is the most common symptom; however, headache, anorexia, weight loss, and malaise are frequent complaints.
Extrapulmonary manifestations can be varied, including skin lesions, hepatosplenomegaly, abnormal liver enzymes, pancytopenia, gastrointestinal involvement, and a sepsis-like syndrome.[2]Wheat LJ, Connolly-Stringfield PA, Baker RL, et al. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore). 1990 Nov;69(6):361-74.
http://www.ncbi.nlm.nih.gov/pubmed/2233233?tool=bestpractice.com
Central nervous system dissemination of the disease may present as a brain lesion or meningitis.
In patients with advanced HIV/AIDS, histoplasmosis pneumonia usually occurs in conjunction with disseminated disease and presents with symptoms of pulmonary infection that are more acute and more severe than those seen in other patient groups.
Investigations
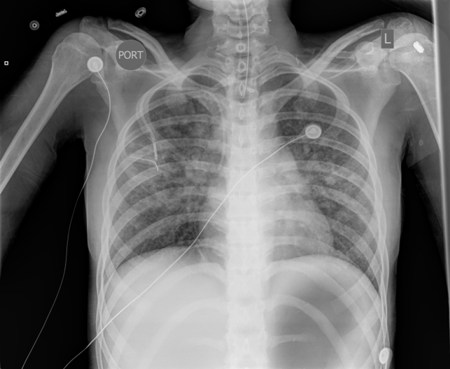
Chest x-ray
This should be performed in all patients. Even with mild disease, chest x-ray will assist in determining the extent of pulmonary involvement and help distinguish the disease from influenza and community-acquired pneumonia.
Calcified granulomas may be seen; these represent healed foci of previous infection with the fungus (focal infiltrates).
Unilateral or bilateral interstitial or reticulonodular infiltrates, nodules, mediastinal or hilar lymphadenopathy, and cavitary lesions are common findings. Pleural effusions are uncommon.
HIV-infected and immunocompromised patients with pulmonary histoplasmosis may present with diffuse bilateral reticulonodular infiltrates indistinguishable from pneumocystis pneumonia.[2]Wheat LJ, Connolly-Stringfield PA, Baker RL, et al. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore). 1990 Nov;69(6):361-74.
http://www.ncbi.nlm.nih.gov/pubmed/2233233?tool=bestpractice.com
In both immunocompromised and immunocompetent patients, the presence of diffuse interstitial infiltrates on chest x-ray warrants evaluation for disseminated fungal histoplasmosis. [Figure caption and citation for the preceding image starts]: Chest x-ray of a patient with histoplasmosis, demonstrating bilateral diffuse reticulonodular infiltratesFrom the personal collection of Dr David L. Goldman [Citation ends].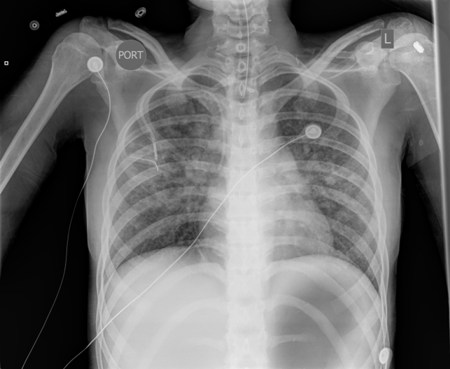
Computed tomography (CT) scan
In immunosuppressed patients, where the index of suspicion for a fungal process is high and the chest x-ray is normal, a CT scan should be a part of the initial evaluation.
The CT scan will assist in determining the extent of dissemination.[Figure caption and citation for the preceding image starts]: Lung CT scan showing classic "snowstorm" appearance of acute histoplasmosisPublic Health Image Library, US Centers for Disease Control and Prevention [Citation ends].
Laboratory studies can serve as a basis for diagnosis with compatible clinical and radiographic findings. Each test has certain limitations that should be recognized before use. Samples may be taken from sputum, urine, serum, bronchoalveolar lavage (BAL), or cerebrospinal fluid (CSF). Usually sputum, urine, and serum are used, but if severe disease is indicated clinically and initial laboratory results are equivocal, then BAL and CSF samples may be used to confirm the diagnosis.
Culture
Fungal cultures are the gold standard test to confirm the diagnosis, but can be technically challenging and time consuming.[28]Hage CA, Carmona EM, Epelbaum O, et al. Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019 Sep 1;200(5):535-50.
https://www.atsjournals.org/doi/full/10.1164/rccm.201906-1185ST?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/31469325?tool=bestpractice.com
Cultures are most useful in patients with chronic pulmonary histoplasmosis or disseminated disease. Patients with acute diffuse pneumonia and disseminated histoplasmosis have a high fungal burden; sputum fungal cultures are usually positive in 60% to 85% of cases.[29]Wheat LJ. Improvements in diagnosis of histoplasmosis. Expert Opin Biol Ther. 2006 Nov;6(11):1207-21.
http://www.ncbi.nlm.nih.gov/pubmed/17049017?tool=bestpractice.com
[30]Wheat LJ, Garringer T, Brizendine E, et al. Diagnosis of histoplasmosis by antigen detection based upon experience at the histoplasmosis reference laboratory. Diagn Microbiol Infect Dis. 2002 May;43(1):29-37.
http://www.ncbi.nlm.nih.gov/pubmed/12052626?tool=bestpractice.com
By contrast, patients with acute localized pulmonary disease have a low fungal burden; in these patients, sputum culture has a sensitivity of only 15%.
The fungus grows slowly and may take up to 4 to 6 weeks to grow in culture. Samples may be taken from sputum or BAL.
In patients with disseminated disease (e.g., patients with AIDS), culture of the blood using lysis centrifugation bottles increases diagnostic sensitivity when compared with standard culture techniques. Bone marrow culture may also be useful in patients with disseminated disease.[25]National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and the Infectious Diseases Society of America. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: histoplasmosis. Sep 2019 [internet publication].
https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/histoplasmosis
[Figure caption and citation for the preceding image starts]: Slant cultures growing Histoplasma capsulatum colonies on 2 different kinds of agarDr Lenore Haley, Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].
BAL culture has a sensitivity of 89% in patients with AIDS.[31]Wheat LJ, Connolly-Stringfield P, Williams B, et al. Diagnosis of histoplasmosis in patients with the acquired immunodeficiency syndrome by detection of Histoplasma capsulatum polysaccharide antigen in bronchoalveolar lavage fluid. Am Rev Respir Dis. 1992 Jun;145(6):1421-4.
http://www.ncbi.nlm.nih.gov/pubmed/1596012?tool=bestpractice.com
Antigen detection: enzyme immunoassay
This test provides a rapid diagnosis and is based on the detection of H capsulatum galactomannan. It is useful for patients who are severely ill.[32]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 5 Mar 2024 [Epub ahead of print].
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
It can use samples of serum, urine, BAL, and CSF. Antigen testing of urine or serum is recommended for the rapid diagnosis of suspected disseminated and acute pulmonary histoplasmosis, for which rapid initiation of treatment is paramount to improve outcomes.[4]Thompson GR 3rd, Le T, Chindamporn A, et al. Global guideline for the diagnosis and management of the endemic mycoses: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology. Lancet Infect Dis. 2021 Dec;21(12):e364-74.
http://www.ncbi.nlm.nih.gov/pubmed/34364529?tool=bestpractice.com
[28]Hage CA, Carmona EM, Epelbaum O, et al. Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019 Sep 1;200(5):535-50.
https://www.atsjournals.org/doi/full/10.1164/rccm.201906-1185ST?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/31469325?tool=bestpractice.com
[32]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 5 Mar 2024 [Epub ahead of print].
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
[33]World Health Organization. Guidelines for diagnosing and managing disseminated histoplasmosis among people living with HIV. 1 April 2020 [internet publication].
https://www.who.int/publications/i/item/9789240006430
[34]Smith DJ, Free RJ, Thompson Iii GR, et al. Clinical testing guidance for coccidioidomycosis, histoplasmosis, and blastomycosis in patients with community-acquired pneumonia for primary and urgent care providers. Clin Infect Dis. 2023 Oct 6:ciad619.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciad619/7295325
http://www.ncbi.nlm.nih.gov/pubmed/37802909?tool=bestpractice.com
[35]Centers for Disease Control and Prevention. Fungal diseases: clinical testing guidance for coccidioidomycosis, histoplasmosis, and blastomycosis in patients with community-acquired pneumonia. Nov 2023 [internet publication].
https://www.cdc.gov/fungal/diagnosticalgorithms.html
Patients with acute diffuse pneumonia and disseminated histoplasmosis have a high fungal burden, and the urine antigen test is positive in 75% of patients.[29]Wheat LJ. Improvements in diagnosis of histoplasmosis. Expert Opin Biol Ther. 2006 Nov;6(11):1207-21.
http://www.ncbi.nlm.nih.gov/pubmed/17049017?tool=bestpractice.com
[30]Wheat LJ, Garringer T, Brizendine E, et al. Diagnosis of histoplasmosis by antigen detection based upon experience at the histoplasmosis reference laboratory. Diagn Microbiol Infect Dis. 2002 May;43(1):29-37.
http://www.ncbi.nlm.nih.gov/pubmed/12052626?tool=bestpractice.com
By contrast, patients with acute localized pulmonary disease have a low fungal burden, and the urine antigen test is positive in only approximately 30% of patients.[36]Williams B, Fojtasek M, Connolly-Stringfield P, et al. Diagnosis of histoplasmosis by antigen detection during an outbreak in Indianapolis, Ind. Arch Pathol Lab Med. 1994 Dec;118(12):1205-8.
http://www.ncbi.nlm.nih.gov/pubmed/7979915?tool=bestpractice.com
Sensitivity of antigen detection in urine is comparable to or better than in serum.[37]Fandiño-Devia E, Rodríguez-Echeverri C, Cardona-Arias J, et al. Antigen detection in the diagnosis of histoplasmosis: a meta-analysis of diagnostic performance. Mycopathologia. 2016 Apr;181(3-4):197-205.
http://www.ncbi.nlm.nih.gov/pubmed/26559429?tool=bestpractice.com
It is especially useful in making the diagnosis in immunocompromised patients or in those who are severely ill and may not have developed an antibody response.[36]Williams B, Fojtasek M, Connolly-Stringfield P, et al. Diagnosis of histoplasmosis by antigen detection during an outbreak in Indianapolis, Ind. Arch Pathol Lab Med. 1994 Dec;118(12):1205-8.
http://www.ncbi.nlm.nih.gov/pubmed/7979915?tool=bestpractice.com
Antigen detection has a sensitivity of 85% and specificity of 92% in BAL specimens.[38]Hage CA, Davis TE, Egan L, et al. Diagnosis of pulmonary histoplasmosis and blastomycosis by detection of antigen in bronchoalveolar lavage fluid using an improved second-generation enzyme-linked immunoassay. Respir Med. 2007 Jan;101(1):43-7.
https://www.resmedjournal.com/article/S0954-6111(06)00228-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/16753290?tool=bestpractice.com
For patients with AIDS and disseminated histoplasmosis, the sensitivity of antigen detection in BAL fluid appears to be comparable with that in blood.[31]Wheat LJ, Connolly-Stringfield P, Williams B, et al. Diagnosis of histoplasmosis in patients with the acquired immunodeficiency syndrome by detection of Histoplasma capsulatum polysaccharide antigen in bronchoalveolar lavage fluid. Am Rev Respir Dis. 1992 Jun;145(6):1421-4.
http://www.ncbi.nlm.nih.gov/pubmed/1596012?tool=bestpractice.com
Serum antigen levels decrease within the first 2 weeks of therapy, while urine antigen levels may persist in low concentrations for many months before they disappear.[39]Fojtasek MF, Kleiman MB, Connolly-Stringfield P, et al. The Histoplasma capsulatum antigen assay in disseminated histoplasmosis in children. Pediatr Infect Dis J. 1994 Sep;13(9):801-5.
http://www.ncbi.nlm.nih.gov/pubmed/7808850?tool=bestpractice.com
Antigen levels can be used to monitor patients’ progress while they are receiving antifungal therapy; antigen levels decrease with effective therapy whereas an increase predicts relapse.[28]Hage CA, Carmona EM, Epelbaum O, et al. Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019 Sep 1;200(5):535-50.
https://www.atsjournals.org/doi/full/10.1164/rccm.201906-1185ST?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/31469325?tool=bestpractice.com
Serology (antibody detection): immunodiffusion precipitin test
Antibody testing is recommended for immunocompetent patients with suspected pulmonary histoplasmosis.[28]Hage CA, Carmona EM, Epelbaum O, et al. Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019 Sep 1;200(5):535-50.
https://www.atsjournals.org/doi/full/10.1164/rccm.201906-1185ST?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/31469325?tool=bestpractice.com
The result is positive in 90% of symptomatic patients with acute pulmonary histoplasmosis and nearly 100% with chronic pulmonary histoplasmosis. This test is relatively sensitive but has some limitations because of cross-reactivity.
Measurable antibodies appear 4 to 8 weeks after acute infection and last for 12 to 18 months. This may explain why serology may be negative initially but then positive 1 month later.
Background seropositivity in endemic areas is low; therefore, the immunodiffusion test has a high sensitivity and specificity even in endemic regions.[40]Wheat J, French ML, Kohler RB, et al. The diagnostic laboratory tests for histoplasmosis: analysis of experience in a large urban outbreak. Ann Intern Med. 1982 Nov;97(5):680-5.
http://www.ncbi.nlm.nih.gov/pubmed/6814316?tool=bestpractice.com
The result is reported as the presence of M or H bands.[29]Wheat LJ. Improvements in diagnosis of histoplasmosis. Expert Opin Biol Ther. 2006 Nov;6(11):1207-21.
http://www.ncbi.nlm.nih.gov/pubmed/17049017?tool=bestpractice.com
H and M antigens are glycoproteins released by the fungus. The M band is found in approximately 76% of patients with acute pulmonary histoplasmosis. The H band is seen in only 20% of infected patients but is associated with severe acute pulmonary histoplasmosis, disseminated infection, and cavitary disease.[29]Wheat LJ. Improvements in diagnosis of histoplasmosis. Expert Opin Biol Ther. 2006 Nov;6(11):1207-21.
http://www.ncbi.nlm.nih.gov/pubmed/17049017?tool=bestpractice.com
The M band tends to persist longer than the H band. Its presence can be indicative of acute, chronic or resolved infection.
In patients with AIDS, the sensitivity of serologic tests, including the immunodiffusion test, is reduced to 70%.[2]Wheat LJ, Connolly-Stringfield PA, Baker RL, et al. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore). 1990 Nov;69(6):361-74.
http://www.ncbi.nlm.nih.gov/pubmed/2233233?tool=bestpractice.com
Likewise, the sensitivity of serology is likely to be decreased in other conditions associated with immunosuppression (e.g., organ transplantation or chronic corticosteroid administration).
Serology (antibody detection): complement fixation assay
Antibody testing is recommended for immunocompetent patients with suspected pulmonary histoplasmosis.[28]Hage CA, Carmona EM, Epelbaum O, et al. Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019 Sep 1;200(5):535-50.
https://www.atsjournals.org/doi/full/10.1164/rccm.201906-1185ST?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/31469325?tool=bestpractice.com
[32]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 5 Mar 2024 [Epub ahead of print].
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
This test is quicker and more sensitive than the immunodiffusion test (95% versus 90%) but has a lower specificity due to cross-reactive antibodies induced by other mycotic infections (e.g., coccidioidomycosis, blastomycosis).[40]Wheat J, French ML, Kohler RB, et al. The diagnostic laboratory tests for histoplasmosis: analysis of experience in a large urban outbreak. Ann Intern Med. 1982 Nov;97(5):680-5.
http://www.ncbi.nlm.nih.gov/pubmed/6814316?tool=bestpractice.com
It uses H capsulatum yeast and mycelial antigens.
Sensitivity may be decreased in immunocompromised individuals.[32]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 5 Mar 2024 [Epub ahead of print].
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
Titers between 1:8 and 1:16 are considered low positive and must be interpreted in a clinical context. Titers ≥1:32 or a fourfold rise in titer are diagnostic of acute infection.[41]Guimarães AJ, Nosanchuk JD, Zancopé-Oliveira RM. Diagnosis of histoplasmosis. Braz J Microbiol. 2006 Jan;37(1):1-13.
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2863343
http://www.ncbi.nlm.nih.gov/pubmed/20445761?tool=bestpractice.com
Serology (antibody detection): enzyme immunoassay
Antibody testing is recommended for immunocompetent patients with suspected pulmonary histoplasmosis.[28]Hage CA, Carmona EM, Epelbaum O, et al. Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019 Sep 1;200(5):535-50.
https://www.atsjournals.org/doi/full/10.1164/rccm.201906-1185ST?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/31469325?tool=bestpractice.com
[32]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 5 Mar 2024 [Epub ahead of print].
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
Commercially available assay that provides quantitative measurement of histoplasmosis specific-immunoglobulin (Ig)G and IgM levels.
In one limited clinical study, this assay was reported to be more sensitive than both complement fixation assays and immunodiffusion assays in the diagnosis of acute pulmonary histoplasmosis.[42]Richer SM, Smedema ML, Durkin MM, et al. Improved diagnosis of acute pulmonary histoplasmosis by combining antigen and antibody detection. Clin Infect Dis. 2016 Apr 1;62(7):896-902.
https://academic.oup.com/cid/article/62/7/896/2463002
http://www.ncbi.nlm.nih.gov/pubmed/26797210?tool=bestpractice.com
Combined use of this assay with antigen detection may enhance the diagnosis of acute pulmonary histoplasmosis.[32]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 5 Mar 2024 [Epub ahead of print].
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
[42]Richer SM, Smedema ML, Durkin MM, et al. Improved diagnosis of acute pulmonary histoplasmosis by combining antigen and antibody detection. Clin Infect Dis. 2016 Apr 1;62(7):896-902.
https://academic.oup.com/cid/article/62/7/896/2463002
http://www.ncbi.nlm.nih.gov/pubmed/26797210?tool=bestpractice.com
Limitations include cross-reactivity with antibodies to other fungi and decreased sensitivity in immunocompromised individuals.[32]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 5 Mar 2024 [Epub ahead of print].
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
Complete blood count
The results will assist in confirming or rejecting the possibility of disseminated disease.
Immunocompetent patients with histoplasmosis pneumonia may demonstrate only mild anemia.
Patients with progressive disseminated histoplasmosis may have evidence of anemia, neutropenia, pancytopenia, and thrombocytopenia due to disseminated infection involving the reticuloendothelial system.
Liver function tests (LFTs)
These are helpful at baseline if treatment is to be azole antifungals, because of the drugs' risk of hepatotoxicity.
Elevated LFTs in the setting of histoplasmosis infection suggest the presence of disseminated disease.
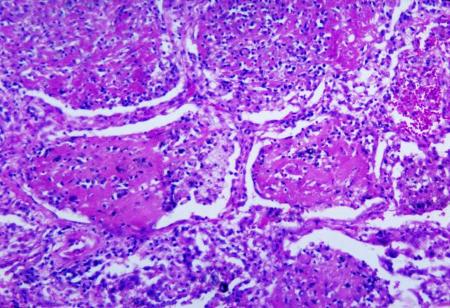
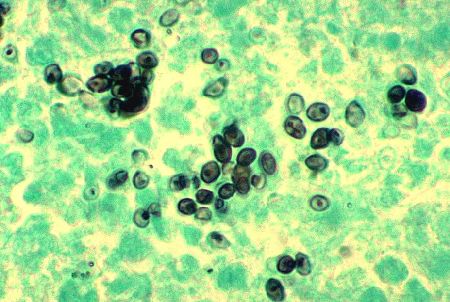
Biopsy
Tissue should be obtained whenever possible to allow for histopathologic diagnosis via fungal stains and fungal culture.[4]Thompson GR 3rd, Le T, Chindamporn A, et al. Global guideline for the diagnosis and management of the endemic mycoses: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology. Lancet Infect Dis. 2021 Dec;21(12):e364-74.
http://www.ncbi.nlm.nih.gov/pubmed/34364529?tool=bestpractice.com
On examination H. capsulatum appear as relatively small (2-4 microns), ovoid, intracellular yeast. Granulomatous inflammation may be caseating or non-caseating.
Periodic acid-Schiff or Grocott methenamine silver staining may be used.[4]Thompson GR 3rd, Le T, Chindamporn A, et al. Global guideline for the diagnosis and management of the endemic mycoses: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology. Lancet Infect Dis. 2021 Dec;21(12):e364-74.
http://www.ncbi.nlm.nih.gov/pubmed/34364529?tool=bestpractice.com
Sensitivity of histopathology will vary according to the burden of disease and degree of immunosuppression.[4]Thompson GR 3rd, Le T, Chindamporn A, et al. Global guideline for the diagnosis and management of the endemic mycoses: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology. Lancet Infect Dis. 2021 Dec;21(12):e364-74.
http://www.ncbi.nlm.nih.gov/pubmed/34364529?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Methenamine silver stain revealing Histoplasma capsulatum fungi in lung tissue Dr Edwin P. Ewing, Jr., Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].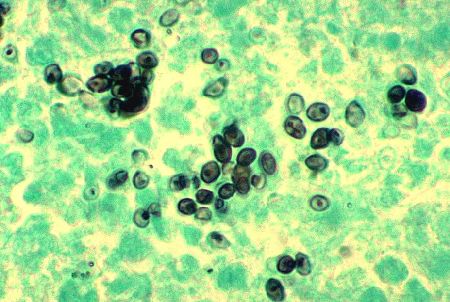 [Figure caption and citation for the preceding image starts]: Histopathologic changes associated with histoplasmosis of the lungDr Martin Hicklin, Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].
[Figure caption and citation for the preceding image starts]: Histopathologic changes associated with histoplasmosis of the lungDr Martin Hicklin, Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].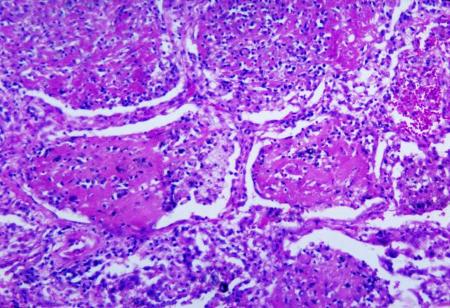
Typical laboratory findings
Acute pulmonary histoplasmosis (symptoms <4 weeks)
Acute pulmonary histoplasmosis (symptoms >4 weeks)
Chronic pulmonary histoplasmosis
Disseminated disease
Sputum fungal cultures are positive in 60% to 85% cases. Serology is positive in most cases, though sensitivity may be adversely affected in immunocompromised patients. Antigen detection has a sensitivity of more than 90% for disseminated disease in immunocompromised patients.[43]Hage CA, Ribes JA, Wengenack NL, et al. A multicenter evaluation of tests for diagnosis of histoplasmosis. Clin Infect Dis. 2011 Sep;53(5):448-54.
https://www.doi.org/10.1093/cid/cir435
http://www.ncbi.nlm.nih.gov/pubmed/21810734?tool=bestpractice.com
Bone marrow examination may provide a rapid method of diagnosis in patients with disseminated disease, especially patients with AIDS.[25]National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and the Infectious Diseases Society of America. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: histoplasmosis. Sep 2019 [internet publication].
https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/histoplasmosis


 [Figure caption and citation for the preceding image starts]: Histopathologic changes associated with histoplasmosis of the lungDr Martin Hicklin, Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].
[Figure caption and citation for the preceding image starts]: Histopathologic changes associated with histoplasmosis of the lungDr Martin Hicklin, Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].