Etiology
Histoplasma capsulatum is a dimorphic fungus and a soil saprophyte. It exists as a mold below 95°F (35°C) and as a yeast at body temperature in animal and human hosts. Sporulation is enhanced by the presence of bird and bat excreta. Infection occurs when Histoplasma spores are inhaled from the environment.[11] The manifestations of infection depend on the inoculum size and underlying host immunity. Inhalational exposure to a large inoculum of infectious spores leads to symptomatic acute pulmonary histoplasmosis, while defects in cell-mediated immunity predispose to more persistent symptoms and possibly disseminated disease. The incubation period for acute pulmonary histoplasmosis is usually 1 to 3 weeks. Exposure in patients with underlying chronic lung disease leads to chronic pulmonary histoplasmosis.[Figure caption and citation for the preceding image starts]: Histoplasma capsulatum in a soil sample Dr Libero Ajello, Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].
Pathophysiology
Infection requires inhalation of Histoplasma spores (microconidia), which germinate into yeast-like forms within the alveoli. Yeast forms of Histoplasma are ingested by macrophages in the lungs and retain their ability to survive and proliferate within macrophages. Infected macrophages, via the regional lymphatics and bloodstream, participate in dissemination of the organism during early infection.[12][13] Specific immunity develops within 2 weeks of exposure in immunocompetent hosts, and sensitized T cells produce interleukin-12, tumor necrosis factor (TNF)-alpha, and interferon-gamma, which stimulate macrophages to kill the fungus.[14] Cellular immunity attained through previous exposure decreases the incidence and severity of symptomatic infections. Therefore, young children are affected more frequently than adults. Infection is localized in Histoplasma-containing granulomas, which are clinically silent and may be discovered incidentally on biopsy or autopsy. Chronic pulmonary histoplasmosis occurs in patients with underlying lung disease (e.g., emphysema); infiltration of the upper lobes of one or both lungs occurs with cavitation. Patients with altered cellular immunity or those treated with immunosuppressant therapy, including TNF-alpha antagonists, may develop progressive disseminated disease throughout the body as the result of reactivation of a latent infection.[15][Figure caption and citation for the preceding image starts]: Gross pathology specimen of lung showing cut surface of fibrocaseous nodule due to Histoplasma capsulatumPublic Health Image Library, US Centers for Disease Control and Prevention and ASCP Atlas of Clinical Mycology II [Citation ends].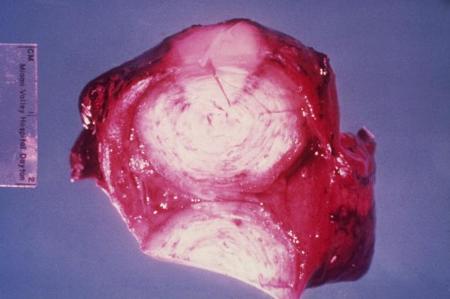
Classification
Types of histoplasmosis[1]
Depending on the host's resistance and immunocompetence, the disease takes one of the following forms:
Thoracic
Latent asymptomatic pulmonary histoplasmosis: low-intensity exposure to fungus in otherwise healthy people
Acute pulmonary histoplasmosis (symptoms <4 weeks): low-intensity exposure to fungus in otherwise healthy people; usually causes mild symptoms
Acute pulmonary histoplasmosis (symptoms >4 weeks): exposure to high fungal inocula in otherwise healthy people
Chronic pulmonary histoplasmosis: occurs in patients with underlying lung disease
Disseminated
Occurs primarily in those with underlying immunosuppressive disorders or in infants; the infection spreads to other organs from the lungs through the bloodstream.
Use of this content is subject to our disclaimer