Medication-induced gynecomastia is common. Anabolic steroid usage, medications that reduce testosterone synthesis or impair testosterone action, medications that increase estrogen levels, hormone therapy for gender dysphoria, and prostate cancer treatment are strong risk factors for development of gynecomastia.
Gynecomastia can be physiologic in newborns and pubertal boys. Prepubertal boys with breast enlargement should undergo evaluation on a case-by-case basis. Environmental exposures causing gynecomastia can be very subtle.[47]Ramsey JT, Li Y, Arao Y, et al. Lavender products associated with premature thelarche and prepubertal gynecomastia: case reports and endocrine-disrupting chemical activities. J Clin Endocrinol Metab. 2019 Nov 1;104(11):5393-405.
https://academic.oup.com/jcem/article/104/11/5393/5544509
http://www.ncbi.nlm.nih.gov/pubmed/31393563?tool=bestpractice.com
[61]Braunstein GD. Environmental gynecomastia. Endocr Pract. 2008 May-Jun;14(4):409-11.
http://www.ncbi.nlm.nih.gov/pubmed/18558589?tool=bestpractice.com
[62]Felner EI, White PC. Prepubertal gynecomastia: indirect exposure to estrogen cream. Pediatrics. 2000 Apr;105(4):E55.
http://www.ncbi.nlm.nih.gov/pubmed/10742376?tool=bestpractice.com
Children are particularly vulnerable.
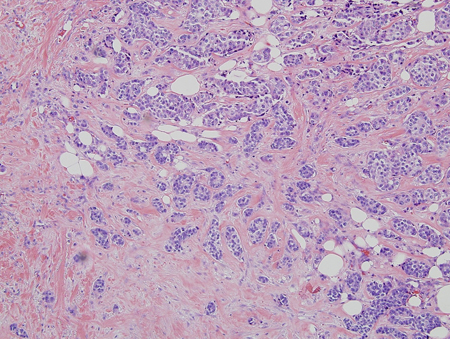
In overweight middle-aged and older men, gynecomastia is often asymptomatic and is found incidentally on physical examination. Usually no additional evaluation is needed in this setting. Symptomatic men are more likely to note irritation than pain, with chafing of the breast. [Figure caption and citation for the preceding image starts]: Gynecomastia evaluationFrom the collection of Catherine B. Niewoehner, MD [Citation ends].
History
The patient should be asked about the duration and course of symptoms. Rapid enlargement in the absence of new exposures raises concern for a hormone-secreting tumor.[27]Bromley HL, Dave R, Lord N, et al. Gynaecomastia: when and why to refer to specialist care. Br J Gen Pract. 2021 Apr;71(705):185-8.
https://bjgp.org/content/71/705/185.long
http://www.ncbi.nlm.nih.gov/pubmed/33771805?tool=bestpractice.com
The history should include the following.
Medication use: include nonprescription or medication bought over the internet, and nutritional supplements. Many medications are associated with gynecomastia, but establishing a causal relationship is difficult.[23]Nuttall FQ, Warrier RS, Gannon MC. Gynecomastia and drugs: a critical evaluation of the literature. Eur J Clin Pharmacol. 2015 May;71(5):569-78.
https://link.springer.com/article/10.1007%2Fs00228-015-1835-x
http://www.ncbi.nlm.nih.gov/pubmed/25827472?tool=bestpractice.com
Opportunities for children to obtain adult medications (including contraceptives) should be reviewed.
Environmental exposure: possible endocrine-disrupting chemicals, alcohol, marijuana, heroin, and cocaine.[27]Bromley HL, Dave R, Lord N, et al. Gynaecomastia: when and why to refer to specialist care. Br J Gen Pract. 2021 Apr;71(705):185-8.
https://bjgp.org/content/71/705/185.long
http://www.ncbi.nlm.nih.gov/pubmed/33771805?tool=bestpractice.com
[63]Braunstein GD. Causal relationship between smoking marijuana and gynecomastia remains unproven. Radiology. 2023 Jun;307(5):e223046.
https://pubs.rsna.org/doi/10.1148/radiol.223046
http://www.ncbi.nlm.nih.gov/pubmed/37278632?tool=bestpractice.com
Workplace and other environmental exposures to estrogens, phytoestrogens, and androgens should be considered.
Specific symptoms of hypogonadism: erectile dysfunction, decreased libido, loss of body hair, decreased strength. Any history indicating abnormal sexual development, including precocious puberty, should be elicited.
General past medical history: including possible malnutrition, should be evaluated.
Symptoms of hyperthyroidism: heat intolerance, weight loss, palpitations, tremor.
Liver impairment: such as cirrhosis (increasing abdominal girth, jaundice).
Renal insufficiency: loss of appetite, fluid retention, tiredness.
Physical exam
Includes: breast exam; assessment for being overweight; signs of hyperthyroidism, liver impairment, or renal insufficiency; and testicular exam.
Breast exam[11]Niewoehner CB, Nuttall FQ. Gynecomastia in a hospitalized male population. Am J Med. 1984 Oct;77(4):633-8.
http://www.ncbi.nlm.nih.gov/pubmed/6486139?tool=bestpractice.com
[16]Klang E, Kanana N, Grossman A, et al. Quantitative CT assessment of gynecomastia in the general population and in dialysis, cirrhotic, and obese patients. Acad Radiol. 2018 May;25(5):626-35.
http://www.ncbi.nlm.nih.gov/pubmed/29326049?tool=bestpractice.com
[27]Bromley HL, Dave R, Lord N, et al. Gynaecomastia: when and why to refer to specialist care. Br J Gen Pract. 2021 Apr;71(705):185-8.
https://bjgp.org/content/71/705/185.long
http://www.ncbi.nlm.nih.gov/pubmed/33771805?tool=bestpractice.com
Should be done in the supine position.
Thumb and forefinger are placed on the outer and inner breast margins and are brought together in a pincer movement along the chest wall until they reach a mound of firm breast tissue located concentrically under the nipple/areola.
The diameter is measured with a ruler or measuring tape.
A diameter 2 cm or less is considered normal in an adult.
If breast enlargement is due only to adipose tissue (pseudogynecomastia), resistance to palpation is felt only beneath the nipple. Gynecomastia can be unilateral (10% to 25%) and might be tender.[8]Nydick M, Bustos J, Dale JH Jr, et al. Gynecomastia in adolescent boys. JAMA. 1961 Nov 4;178:449-54.
http://www.ncbi.nlm.nih.gov/pubmed/14480779?tool=bestpractice.com
[11]Niewoehner CB, Nuttall FQ. Gynecomastia in a hospitalized male population. Am J Med. 1984 Oct;77(4):633-8.
http://www.ncbi.nlm.nih.gov/pubmed/6486139?tool=bestpractice.com
Malignancy is suspected if there is a unilateral eccentric mass; any nipple, areola, or skin abnormality (such as dimpling or breast discharge); or axillary adenopathy. If the clinical picture is suspicious for a malignant lesion, biopsy may be performed (in preference to imaging).[3]Kanakis GA, Nordkap L, Bang AK, et al. EAA clinical practice guidelines-gynecomastia evaluation and management. Andrology. 2019 Nov;7(6):778-93.
https://onlinelibrary.wiley.com/doi/10.1111/andr.12636
http://www.ncbi.nlm.nih.gov/pubmed/31099174?tool=bestpractice.com
Assessment for being overweight
Body mass index (BMI) 25 to 29.9 kg/m².
BMI ≥30 kg/m² (obese).
Before 18 years of age, being overweight is defined by 85th to 95th percentiles for BMI for age and sex; for obesity it is above 95th percentile.
Signs of hyperthyroidism, liver impairment, or renal insufficiency
Tremor, goiter (hyperthyroidism).
Ascites, spider angiomata (liver impairment).
Fluid retention, sallow skin color, tremors (renal insufficiency).
Testicular exam[39]Bagatell CJ, Bremner WJ. Androgens in men: uses and abuses. N Engl J Med. 1996 Mar 14;334(11):707-14.
http://www.ncbi.nlm.nih.gov/pubmed/8594431?tool=bestpractice.com
[40]Perry PJ, Lund BC, Deninger MJ, et al. Anabolic steroid use in weight lifters and body builders: an internet survey of drug utilization. Clin J Sport Med. 2005 Sep;15(5):326-30.
http://www.ncbi.nlm.nih.gov/pubmed/16162991?tool=bestpractice.com
[41]Friedl KE, Yesalis CE. Self-treatment of gynecomastia in bodybuilders who use anabolic steroids. Physician Sportsmed. 1989 Mar;17(3):67-79.
http://www.ncbi.nlm.nih.gov/pubmed/27413851?tool=bestpractice.com
Assess for small size, mass, or abnormal consistency.
Marked muscle development, small firm testicles, and adult acne suggest exogenous androgen exposure.
Decreased body hair, female fat distribution, decreased strength, or small or soft testicles suggest hypogonadism.
A mass may suggest human chorionic gonadotropin (hCG)-producing tumor or Leydig cell tumor.
Laboratory evaluation
If the cause of gynecomastia is not obvious, measurement of thyroid-stimulating hormone, creatinine, and liver function tests should follow.
If these are normal, luteinizing hormone (LH), testosterone, sex hormone binding globulin (SHBG), estradiol, beta-hCG, dehydroepiandrosterone-sulfate (DHEAS), and prolactin are measured. LH and testosterone have a diurnal rhythm and should be measured in the morning when levels are highest.[27]Bromley HL, Dave R, Lord N, et al. Gynaecomastia: when and why to refer to specialist care. Br J Gen Pract. 2021 Apr;71(705):185-8.
https://bjgp.org/content/71/705/185.long
http://www.ncbi.nlm.nih.gov/pubmed/33771805?tool=bestpractice.com
[64]Bhasin S, Brito JP, Cunningham GR, et al. Testosterone therapy in men with hypogonadism: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018 May 1;103(5):1715-44.
https://academic.oup.com/jcem/article/103/5/1715/4939465
http://www.ncbi.nlm.nih.gov/pubmed/29562364?tool=bestpractice.com
Testosterone is ideally measured by a specific assay such as liquid chromatography tandem mass spectrometry.[64]Bhasin S, Brito JP, Cunningham GR, et al. Testosterone therapy in men with hypogonadism: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018 May 1;103(5):1715-44.
https://academic.oup.com/jcem/article/103/5/1715/4939465
http://www.ncbi.nlm.nih.gov/pubmed/29562364?tool=bestpractice.com
A free testosterone level, measured by equilibrium dialysis, may be helpful in assessing the bioavailability of male hormone if total testosterone is equivocal.
No laboratory abnormality is found in the majority of patients with chronic gynecomastia found incidentally on physical exam, compared with 25% of cases with recent onset.[20]Braunstein GD. Gynecomastia. New Engl J Med. 1993 Feb 18;328(7):490-95.
http://www.ncbi.nlm.nih.gov/pubmed/8421478?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Hormones involved in male breast developmentFrom the collection of Catherine B. Niewoehner, MD [Citation ends].
Imaging
Breast imaging is indicated when the clinical exam is equivocal.[3]Kanakis GA, Nordkap L, Bang AK, et al. EAA clinical practice guidelines-gynecomastia evaluation and management. Andrology. 2019 Nov;7(6):778-93.
https://onlinelibrary.wiley.com/doi/10.1111/andr.12636
http://www.ncbi.nlm.nih.gov/pubmed/31099174?tool=bestpractice.com
[65]American College of Radiology. ACR appropriateness criteria: evaluation of the symptomatic male breast. 2018 [internet publication].
https://acsearch.acr.org/docs/3091547/Narrative
Suspicious features on ultrasound may prompt mammography.[65]American College of Radiology. ACR appropriateness criteria: evaluation of the symptomatic male breast. 2018 [internet publication].
https://acsearch.acr.org/docs/3091547/Narrative
[66]Billa E, Kanakis GA, Goulis DG. Imaging in gynecomastia. Andrology. 2021 Sep;9(5):1444-56.
https://onlinelibrary.wiley.com/doi/10.1111/andr.13051
http://www.ncbi.nlm.nih.gov/pubmed/34033252?tool=bestpractice.com
Breast ultrasound is recommended if surgery is planned for gynecomastia.[65]American College of Radiology. ACR appropriateness criteria: evaluation of the symptomatic male breast. 2018 [internet publication].
https://acsearch.acr.org/docs/3091547/Narrative
Testicular ultrasound should be ordered in patients with sudden gynecomastia onset (with or without a palpable testicular mass) and raised serum levels of estrogen, or raised beta-hCG, to rule out testicular tumor.[3]Kanakis GA, Nordkap L, Bang AK, et al. EAA clinical practice guidelines-gynecomastia evaluation and management. Andrology. 2019 Nov;7(6):778-93.
https://onlinelibrary.wiley.com/doi/10.1111/andr.12636
http://www.ncbi.nlm.nih.gov/pubmed/31099174?tool=bestpractice.com
[27]Bromley HL, Dave R, Lord N, et al. Gynaecomastia: when and why to refer to specialist care. Br J Gen Pract. 2021 Apr;71(705):185-8.
https://bjgp.org/content/71/705/185.long
http://www.ncbi.nlm.nih.gov/pubmed/33771805?tool=bestpractice.com
Abdominal CT or MRI should be performed if an adrenal adenoma or carcinoma is suspected based on elevations of DHEAS and estradiol, or clinical findings suggesting concomitant glucocorticoid and/or mineralocorticoid excess.[4]Narula HS, Carlson HE. Gynaecomastia-pathophysiology, diagnosis and treatment. Nat Rev Endocrinol. 2014 Nov;10(11):684-98.
http://www.ncbi.nlm.nih.gov/pubmed/25112235?tool=bestpractice.com
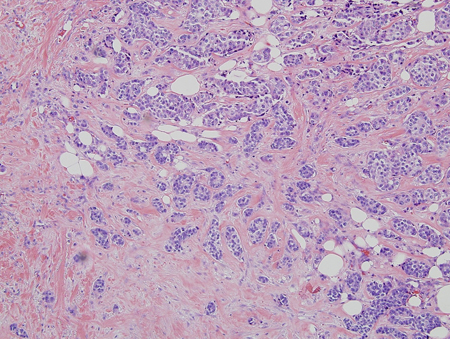
Biopsy
Biopsy is prompted by any irregular, rubbery, hard, fixed, or eccentric (not subareolar) mass; overlying nipple, areola, or skin abnormality; or axillary adenopathy. These findings are suggestive of breast cancer.[3]Kanakis GA, Nordkap L, Bang AK, et al. EAA clinical practice guidelines-gynecomastia evaluation and management. Andrology. 2019 Nov;7(6):778-93.
https://onlinelibrary.wiley.com/doi/10.1111/andr.12636
http://www.ncbi.nlm.nih.gov/pubmed/31099174?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Histology: breast cancer; nests of malignant ductal carcinoma invading tissue; 10X magnificationFrom Minneapolis Veterans Affairs Medical Center pathology collection [Citation ends].