Approach
The management of cleft lip with or without cleft palate involves a multidisciplinary team providing comprehensive care of the condition's functional and esthetic issues from birth into adulthood.[40][42] In addition to making a timely diagnosis and referral, primary care pediatricians have an essential role in providing ongoing support to the child and to his or her family.[43]
Orofacial clefts are treated in discrete stages at specific ages, and the method of treatment is dependent on whether the deformity is a complete cleft lip and palate, an isolated cleft palate, an isolated unilateral cleft lip, or an isolated bilateral cleft lip. The timing and nature of the surgery is individualized to the child’s needs.[40] The goal of primary cleft lip repair is to restore normal function and anatomic features, and the goal of primary cleft palate repair is to achieve normal speech and swallow.[40]
A secondary lip repair (lip revision) is often required and can be performed at any age in order to correct unsightly lip esthetics, such as excessive scarring, asymmetric lip volume, or inadequate orbicularis oris continuity.
Complete cleft lip and palate
From birth to 3 months of age, affected infants receive support from the feeding nurse specialist, and airway management if required.
In wide (>1 cm) clefts, presurgical lip taping, oral appliance insertion, or presurgical nasal alveolar molding (PNAM) is also done between birth and 3 months of age prior to definitive cleft lip repair, which is performed as the second stage of cleft lip repair at 6 to 7 months of age. Infants with narrow (<1 cm) clefts receive definitive cleft lip repair without any prior presurgical procedure at around 3 months of age.
In the presence of Eustachian tube dysfunction, bilateral myringotomy and tympanostomy tube (T-tube) (Shepard type) placement is performed concurrently with definitive cleft lip repair.
Between 10 and 14 months of age, affected infants undergo palatoplasty and insertion of a long-lasting T-tube, with additional V-Y columellar advancement (lengthening of short columellar skin, performed by advancing skin from the central lip onto the columella with a V-shaped end and closing the lip, resulting in a Y configuration) in those with bilateral complete cleft lip and palate who have not received or responded to primary techniques (e.g., PNAM).
Between the ages of 2 and 5 years, speech and language therapy is initiated, with additional surgery aimed at improvement of speech for those who find initial therapy insufficient in the management of hypernasal speech.
If there is gross esthetic distortion or nostril stenosis with complete nasal obstruction, intermediate rhinoplasty is performed at any time after definitive cleft lip repair and prior to definitive septorhinoplasty.
Between the ages of 8 and 11 years, alveolar cleft bone grafting with preparatory orthodontics is performed.
Those with dentofacial malocclusion go on to receive definitive septorhinoplasty with additional orthodontics and orthognathic surgery at skeletal maturity.[Figure caption and citation for the preceding image starts]: Unilateral cleft lip and palate preoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
 [Figure caption and citation for the preceding image starts]: Unilateral cleft lip and palate postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
[Figure caption and citation for the preceding image starts]: Unilateral cleft lip and palate postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends]. [Figure caption and citation for the preceding image starts]: Bilateral cleft lip and palate preoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
[Figure caption and citation for the preceding image starts]: Bilateral cleft lip and palate preoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends]. [Figure caption and citation for the preceding image starts]: Bilateral cleft lip and palate postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
[Figure caption and citation for the preceding image starts]: Bilateral cleft lip and palate postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends]. [Figure caption and citation for the preceding image starts]: Unilateral cleft lip postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
[Figure caption and citation for the preceding image starts]: Unilateral cleft lip postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
Isolated cleft palate
From birth to 3 months of age, affected infants receive support from the feeding nurse specialist, and airway management if required.
Between 3 and 6 months of age, bilateral myringotomy and tympanostomy tube (T-tube) (Shepard type) placement is performed if Eustachian tube dysfunction is present.
Between 10 and 14 months of age, affected infants undergo palatoplasty and insertion of a long-lasting T-tube.
Between the ages of 2 and 5 years, speech and language therapy is initiated, with additional surgery aimed at improvement of speech for those who find initial therapy insufficient in the management of hypernasal speech.
Those with dentofacial malocclusion go on to receive preparatory orthodontics with or without orthognathic surgery at skeletal maturity.
Isolated cleft lip
From birth to 3 months of age, affected infants receive support from the feeding nurse specialist.
In wide (>1 cm) clefts, presurgical lip taping, oral appliance insertion, or presurgical alveolar molding (PNAM) is also done between birth and 3 months of age prior to definitive cleft lip repair, which is performed as the second stage of cleft lip repair at 6 to 7 months of age. Infants with narrow (<1 cm) clefts receive definitive cleft lip repair without any prior presurgical procedure at around 3 months of age.
Between 10 and 14 months of age, those with isolated bilateral cleft lip who have not received or responded to primary techniques (e.g., PNAM) undergo V-Y columellar advancement (lengthening of short columellar skin, performed by advancing skin from the central lip onto the columella with a V-shaped end and closing the lip, resulting in a Y configuration).
If there is gross esthetic distortion or nostril stenosis with complete nasal obstruction, intermediate rhinoplasty is performed at any time after definitive cleft lip repair and prior to definitive septorhinoplasty in select cases of lip clefting.
Those with isolated unilateral cleft lip go on to receive definitive septorhinoplasty at skeletal maturity.
In isolated bilateral cleft lip, between the ages of 8 and 11 years, alveolar cleft bone grafting with preparatory orthodontics is performed, and at skeletal maturity, definitive septorhinoplasty is performed with additional orthodontics and orthognathic surgery in the presence of dentofacial malocclusion.[Figure caption and citation for the preceding image starts]: Incomplete unilateral cleft lip preoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
 [Figure caption and citation for the preceding image starts]: Incomplete unilateral cleft lip postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
[Figure caption and citation for the preceding image starts]: Incomplete unilateral cleft lip postoperativelyFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
Specialized feeding
Neonates with any form of orofacial clefting may require extended postnatal hospitalization due to feeding difficulties, although NG tube feeding is seldom required.
Breastfeeding is possible with an isolated cleft lip. However, neonates with a cleft palate often cannot produce the negative pressures necessary for suction. Evidence-based guidelines exist for the use of breastfeeding in patients with CLP, both preoperatively and after cleft repair. These advocate both individualized support for nursing mothers and monitoring newborn weight gain and hydration status.[44][45]
Nasal regurgitation is addressed with upright positioning of the infant during breast and bottle feeding. Feeding nurse specialists teach parents how to optimize bottle feeding using specialized fissured nipples and bottles controlling the flow rate of pumped breast milk or formula. Soft-bodied bottles are squeezed in synchronization with infant sucking to reduce the effort of feeding and maximize the amount of feed entering the mouth. The infant should be burped during pauses, and feeding should not be continued for more than 30 minutes to avoid fatigue.
A Cochrane review of 5 randomized controlled trials examined various feeding interventions and their effects on weight of children at 6 weeks after surgery for repair of cleft lip and palate. While squeezable bottles appeared easier to use than rigid bottles, no differences in growth outcomes were noted. Maxillary plates also showed no evidence for improved growth at 6 weeks after surgery. Weak evidence exists to show that breastfeeding had a positive effect on weight gain after surgery when compared to spoon feeding.[46]
[  ]
]
The neonate will lose weight after birth (up to 10% of birth weight), but the birth weight is expected to be re-established within the first 2 postnatal weeks, and the infant should go on to gain at least 1 ounce per day thereafter.
Airway management
A small proportion of infants with complete cleft lip and palate and isolated cleft palate present with symptoms of severe airway obstruction requiring immediate airway management.
Neonates with Pierre Robin sequence (triad of cleft palate, microgenia, and glossoptosis) may have upper airway obstruction. This is initially treated noninvasively with prone positioning, nasopharyngeal trumpet, and/or nasal CPAP.[47] However, up to 23% of infants with micrognathia have a tongue-related obstruction requiring invasive intervention with endotracheal intubation if prone positioning, nasopharyngeal trumpet, and nasal CPAP are ineffective.[48] Surgical management of airway obstruction in micrognathia includes tongue lip adhesion, mandibular distraction osteogenesis (to move the base of tongue forward and open the airway), and tracheostomy, which should only be undertaken once all other options have been exhausted.[47]
A pediatric otolaryngologist can perform an airway evaluation with a dynamic flexible laryngoscopy to rule out other airway abnormalities and manage associated laryngopharyngeal reflux.[Figure caption and citation for the preceding image starts]: CT distraction osteogenesisFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].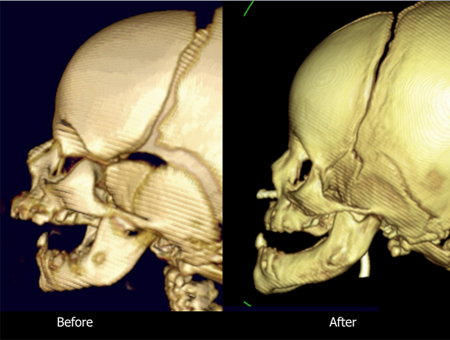
Presurgical lip taping, oral appliances, and presurgical alveolar molding (PNAM)
Wide (>1 cm) clefts in complete cleft lip and palate and isolated cleft lip require a 2-stage cleft lip repair. This involves presurgical lip taping, oral appliance insertion, or PNAM in order to narrow the cleft prior to definitive cleft lip repair.
Daily lip taping with steristrips and benzoin to enhance adherence (as feeding causes wetting of the tape) is undertaken by the parents following instruction, and is used to protect the cheek skin in both bilateral and unilateral cleft lip deformities.
Although a variety of oral devices has been described, the Latham device is used to actively reposition the lateral alveolar cleft segments while deprojecting the protruded premaxilla.[49] The merits of presurgical premaxillary positioning using an intraoral device are still debated.[50] Associated maxillary growth inhibition is often cited, although there are insufficient long-term data to support either side.[51][52][53]
PNAM is performed by the orthodontist and cleft surgeon.
An appliance is placed within the cleft and adjusted weekly to approximate the alveolar segments, thus reducing the width of the cleft alveolus and corresponding soft tissues of the cleft lip. This is done prior to surgical reconstruction with definitive cleft lip repair, which is delayed during PNAM.
The objectives of the PNAM technique are to elongate the columella, expand the cleft nasal mucosa, and improve nasal tip symmetry. It takes advantage of the plasticity of the elastic cartilage of the nose, surrounding soft tissues (skin, muscle, mucosa), and bony maxilla in the early neonatal period. Serum maternal estrogens in the infant are thought to induce a transient window of nasal cartilage pliability similar to that of the pubic symphysis in preparation for childbirth. Thus, PNAM should ideally be initiated within the first 6 postnatal weeks in order to utilize the early plasticity of the nasal cartilages.[54]
The PNAM appliance differs from traditional intraoral alveolar molding devices through the addition of nasal prongs.[55] An orthodontist adjusts the acrylic intraoral appliance by differential addition and removal of the leading edge of the maxillary segments at weekly appointments in order to move the alveolar segments together.[55] Nasal stents are added to the intraoral appliance when the alveolar segments are within 6 mm of one another. These stents are adjusted weekly to create a tissue expander effect on the length of the cleft-side columella and reposition the alar (from the Latin "ala" or wing; the soft tissue and cartilaginous components of the nostril, which includes the lower lateral [alar] cartilages) hooding. This is purported to lead to improved nasal appearance, limited maxillary growth disturbance, and fewer subsequent procedures.[56][57]
Parental compliance is the most important factor in the successful completion of the PNAM treatment program.[Figure caption and citation for the preceding image starts]: Taping of cleft lipFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
 [Figure caption and citation for the preceding image starts]: Presurgical nasoalveolar molding appliance in placeFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
[Figure caption and citation for the preceding image starts]: Presurgical nasoalveolar molding appliance in placeFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends]. [Figure caption and citation for the preceding image starts]: PNAM device in a unilateral cleft showing nasal conformer wire in the right nostrilFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
[Figure caption and citation for the preceding image starts]: PNAM device in a unilateral cleft showing nasal conformer wire in the right nostrilFrom the collection of Travis T. Tollefson, MD, FACS [Citation ends].
Definitive cleft lip repair
Narrow clefts (<1 cm) receive definitive cleft lip repair without any presurgical treatment (presurgical lip taping, oral appliance insertion, or PNAM).
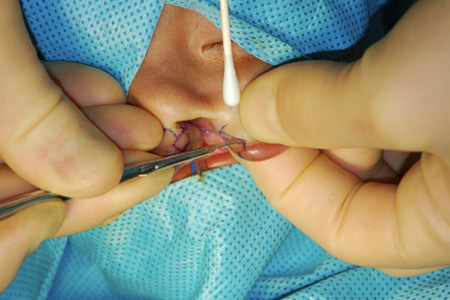
Repair of the unilateral or bilateral cleft lip involves approximation of the 2 sides of the cleft lip using precisely designed segments of tissue, creating exact proportions of the underlying oral mucosa, muscle, and lip contours. One Cochrane review suggests that the evidence supports the intraoperative use of an infraorbital nerve block during cleft lip repair to assist with postoperative pain management. Additional well-designed studies would be needed to compare pain management options.[58]
Unilateral cleft lip repair
Surgical approach to the repair of a unilateral cleft lip is similar to that of a bilateral cleft lip except for the inherent asymmetries of a unilateral defect.
The most important feature of unilateral cleft lip repair is creating symmetric lip contours by lengthening the medial lip segment using a variety of techniques, including rotation-advancement flaps (Millard), triangular (Tennison/Skoog) designs, geometric designs, or a subunit (Fisher) approach.
Bilateral cleft lip repair
The timing and technique for repair of the bilateral cleft lip are related to the extent of the deformity and surgeon preference. Numerous techniques have been described, including those of Millard, Cutting, and Mulliken.[Figure caption and citation for the preceding image starts]: Unilateral cleft lip repair showing rotation-advancement designFrom: Senders CW, Sykes JM. Cleft palate. In: Smith JD, Bumsted RM, eds. Pediatric facial plastic and reconstructive surgery. New York, NY: Raven Press; 1993:162 [Citation ends].
Intermediate rhinoplasty
Although infrequently performed, alterations to the cleft lip nasal deformity can be made with intermediate rhinoplasty at any time after definitive cleft lip repair and prior to definitive septorhinoplasty in select cases of lip clefting: for example, where there is gross esthetic distortion or nostril stenosis with complete nasal obstruction.
Intermediate rhinoplasty can be performed using an external or endonasal surgical approach. The nasal cartilages and soft tissue of the nostril can be treated with suturing and repositioning. Most surgeons delay septal surgery until skeletal maturity is reached, to minimize growth impairment of the nose and maxilla.
Bilateral myringotomy and tympanostomy tube (T-tube) placement
Infants with a cleft palate often have Eustachian tube dysfunction. Bilateral myringotomy and T-tube (Shepard type) placement is performed following tympanograms and head and neck surgery assessment if there is evidence of Eustachian tube dysfunction.
Audiometry is undertaken before and after T-tube placement.
Palatoplasty, long-lasting T-tube placement, and V-Y columellar advancement
The placement of longer-lasting T-tubes following bilateral myringotomy is performed concurrently with palatoplasty (cleft palate repair).
Audiometry is undertaken before and after T-tube placement.
Chronic otorrhea is managed with antibiotic drops or tube change if biofilm accumulation is suspected. Any hearing loss not improved with T-tube placement is treated with hearing amplification following neuro-otologic consultation to consider the various available options (e.g., hearing aid, FM system, softband bone-anchored hearing aid, cochlear implant).
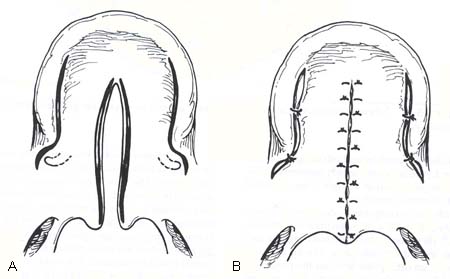
Palatoplasty may be undertaken as a 1- or (rarely) 2-stage repair, and is performed through creation of oral tissue flaps from the palate and rotation of these palatal flaps to allow 3-layer closure (oral mucosa, soft palate muscles, and nasal layer).
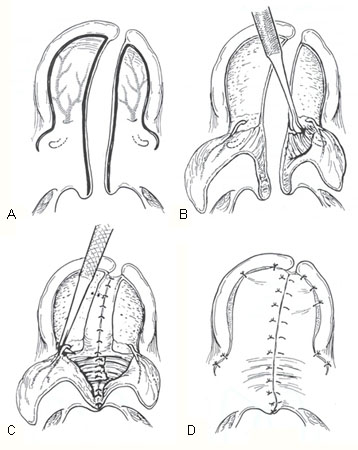
The 2-flap technique is the mainstay of unilateral palatoplasty, with the addition of a vomer (bony component of the nasal septum inferior to the perpendicular plate of the ethmoid bone and posterior to the quadrangular cartilage of the anterior nasal septum) dissection in bilateral palatoplasty. A smaller secondary cleft palate is closed using a von Langenbeck, 3-flap (pushback, Veau-Wardill-Kilner), or Furlow double-opposing Z-plasty, depending on surgeon preference.[59][60][61][Figure caption and citation for the preceding image starts]: Cleft palate repair showing von Langenback designFrom: Senders CW, Sykes JM. Cleft palate. In: Smith JD, Bumsted RM, eds. Pediatric facial plastic and reconstructive surgery. New York, NY: Raven Press; 1993:162 [Citation ends].
 [Figure caption and citation for the preceding image starts]: Cleft palate repair showing 3-flap palatoplasty designFrom: Senders CW, Sykes JM. Cleft palate. In: Smith JD, Bumsted RM, eds. Pediatric facial plastic and reconstructive surgery. New York, NY: Raven Press; 1993:162 [Citation ends].
[Figure caption and citation for the preceding image starts]: Cleft palate repair showing 3-flap palatoplasty designFrom: Senders CW, Sykes JM. Cleft palate. In: Smith JD, Bumsted RM, eds. Pediatric facial plastic and reconstructive surgery. New York, NY: Raven Press; 1993:162 [Citation ends]. [Figure caption and citation for the preceding image starts]: Cleft palate repair showing Furlow double-opposing Z-plasty designFrom: Senders CW, Sykes JM. Cleft palate. In: Smith JD, Bumsted RM, eds. Pediatric facial plastic and reconstructive surgery. New York, NY: Raven Press; 1993:162 [Citation ends].
[Figure caption and citation for the preceding image starts]: Cleft palate repair showing Furlow double-opposing Z-plasty designFrom: Senders CW, Sykes JM. Cleft palate. In: Smith JD, Bumsted RM, eds. Pediatric facial plastic and reconstructive surgery. New York, NY: Raven Press; 1993:162 [Citation ends].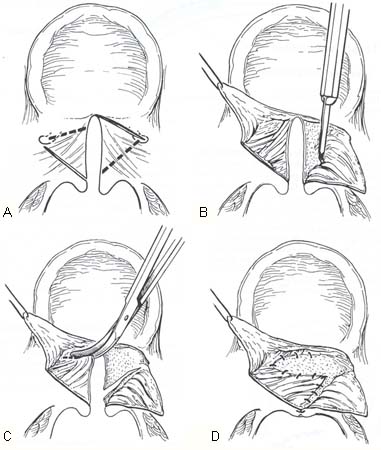
The 2-flap technique is undertaken as follows: after the palate is marked with the chosen design, the oral mucosal flap is incised down to the palatal bones and elevated in a subperiosteal plane. The greater palatine vessels are preserved and the flaps are mobilized to allow the oral layers to contact one another medially. The muscles of the soft palate (tensor veli palatini and levator veli palatini) are dissected to allow tension-free closure after the nasal layers are incised and closed. Absorbable sutures are used in closure, with attention given to minimizing tension on the suture lines by appropriate flap mobilization. [Figure caption and citation for the preceding image starts]: Cleft palate repair showing 2-flap palatoplasty designFrom: Senders CW, Sykes JM. Cleft palate. In: Smith JD, Bumsted RM, eds. Pediatric facial plastic and reconstructive surgery. New York, NY: Raven Press; 1993:162 [Citation ends].
Historically, a 2-stage (Schweckendiek) repair was undertaken. The first stage involved repair of the soft palate with placement of a prosthetic obturator for several years before completing the hard palate repair. The philosophy behind this technique was that maxillary growth would be improved without the development of early scarring around the palatal bony shelves.
The type of palatoplasty (2 flap vs Furlow palatoplasty) has no effect on the incidence of otitis media or postoperative audiogram results.[62] Furlow palatoplasty has been shown to exhibit less velopharyngeal insufficiency (VPI) but increased incidence of fistula.[63]
V-Y columellar advancement (lengthening of short columellar skin, performed by advancing skin from the central lip onto the columella with a V-shaped end and closing the lip, resulting in a Y configuration) is undertaken concurrently in complete bilateral cleft lip and palate and isolated bilateral cleft lip where primary techniques (e.g., PNAM) have not been done or have been unsuccessful.
Speech and language therapy
Speech dysfunction related to orofacial clefting is complex and should be analyzed with the input of a speech and language pathologist. Between the ages of 2 and 5 years, children with complete cleft lip and palate and isolated cleft lip therefore receive speech and language assessment with fluoroscopic speech examination and nasopharyngoscopy in order to observe for velopharyngeal insufficiency (VPI) or dysfunction (VPD). Speech and language therapy is instituted if VPD is present.
Secondary speech surgery
If hypernasal speech is not responsive to speech and language therapy, secondary speech surgery is warranted between the ages of 2 and 5 years, following a VPD evaluation by the surgeon and speech pathologist.
Surgical options for the treatment of VPD include a superiorly based pharyngeal flap or dynamic pharyngoplasty. One meta-analysis, performed in 2012, examined the incidence of persistent VPI associated with either pharyngeal flap surgery or sphincteroplasty. Results showed slightly less VPI with pharyngeal flap surgery.[64] Occasionally a palate-lengthening procedure (Furlow double-opposing Z-plasty) is performed. A patient with a submucous cleft palate may develop velopharyngeal dysfunction requiring surgical intervention. This may include a lengthening palatoplasty (Furlow double-opposing Z-plasty) or pharyngeal surgery (sphincter pharyngoplasty or pharyngeal flap procedure). Both are considered equally effective, although comparative studies have not yet been well-designed or powered enough to differentiate between the effectiveness.
Secondary speech surgery, which may be complicated by obstructive sleep apnea, is performed in 10% to 30% of cases of complete cleft lip and palate and isolated cleft palate.[20]
Alveolar cleft bone grafting with preparatory orthodontics
Preparatory orthodontic maxillary expansion is performed prior to alveolar cleft bone grafting with iliac crest bone on eruption of the key permanent dentition.
If maxillary segments and dentition on either side of the alveolar clefts are aligned, orthodontics can be postponed until bone grafting has been done and most of the permanent dental eruption is complete.
Orthodontics, orthognathic surgery, and definitive septorhinoplasty
Orthodontics and orthognathic surgery for dentofacial malocclusion, which may be necessary in order to obtain Angle Class I molar tooth relationships, are performed prior to definitive septorhinoplasty when the child has reached skeletal maturity. In Angle Class I occlusion (named after the orthodontist Edward Angle), there is a normal relationship between the maxillary and mandibular first molars with the mesiobuccal cusp of the maxillary first molar resting in the mesiobuccal groove of the mandibular first molar.
LeFort advancements are sometimes performed to adjust the dentofacial relationship, particularly in the case of midface hypoplasia. Although providing increased midface protrusion, it is important to note that a moderate amount of relapse in the horizontal and vertical plane does occur.[65]
Definitive septorhinoplasty is performed without orthodontics and orthognathic surgery in isolated unilateral cleft lip when the child has reached skeletal maturity.
Definitive septorhinoplasty is completed using an open approach in order to correct the asymmetric upper and lower lateral cartilages and realign the caudal septum that is deviated to the noncleft side. Symmetry of the alar base (the soft tissue and cartilaginous components of the nostril, which includes the lower lateral [alar] cartilages) is corrected with alar base excisions and, on the cleft side, is augmented with cartilage, bone, or allograft. Lateral crural strut grafting and nasal tip refining techniques (interdomal sutures and tip shield grafts) improve symmetry. Alar rim grafts and excision of nostril hooding are also effective in select cases. Osteotomies and dorsal refinement (excision or augmentation) are combined with spreader grafting between the upper lateral cartilages for enhanced support.
Use of this content is subject to our disclaimer