Approach
History and physical examination are nonspecific, and the patient is often asymptomatic.
History
In a symptomatic patient, exertional dyspnea, easy fatigability, and nonexertional chest pain are the most common symptoms. The patient may also complain of palpitations, diaphoresis, paroxysmal nocturnal dyspnea, and orthopnea. A history of left-sided heart failure and other valve pathologies such as mitral stenosis and endocarditis may be present.
A thorough history regarding previous cardiac surgeries and pulmonary valvuloplasty should be obtained, including repair of tetralogy of Fallot and Ross procedure (with prosthetic pulmonary valve or homograft valve replacement).
Physical examination
Jugular venous pressure may be elevated and a prominent right ventricular (RV) anterior precordial lift present. Most commonly, a short, low-pitched diastolic decrescendo murmur and systolic murmur may be heard along the left sternal border.[6]
Although the likelihood of isolated right-sided heart failure secondary to pulmonary regurgitation is low, it should be considered in patients with lower extremity edema, hepatomegaly, and ascites.
Tests
ECG may show incomplete right bundle branch block and right axis deviation, findings consistent with right ventricular dilation that occurs either while in a compensated volume overload state or in a decompensated pressure overload state. In a compensated state of pressure overload, right ventricular hypertrophy may be present by ECG criteria that include the following: tall R wave in V1 or qR in V1; R wave greater than S wave in V1; R wave progression reversal in the precordial leads; inverted T wave in the anterior precordial leads; right axis deviation and right atrial enlargement. In pulmonary regurgitation after repair of tetralogy of Fallot, QRS prolongation may be found.
A transthoracic echocardiogram (TTE) can be used to assess severity, mechanism, etiology, RV size and function, other valvular abnormalities, and RV systolic pressure, and should be ordered in all patients in whom pulmonary regurgitation is suspected.[7] Although the pulmonary valve leaflets are often difficult to visualize by TTE, color flow imaging is most often used for detection of pulmonary regurgitation (PR). Severity of PR is usually assessed by the diameter of the jet at its origin immediately below the valve, in the right ventricular outflow tract (RVOT), on the parasternal short axis view. A jet width that occupies >65% of the RVOT is suggestive of severe PR.[8] The continuous-wave Doppler profile of the PR jet in the parasternal short axis view is also fundamental in assessing the presence and severity of PR by TTE. Where mild pulmonary regurgitation will have slow deceleration, the continuous-wave Doppler signal of severe pulmonary regurgitation will have a steep deceleration returning to baseline by the end of diastole.[9] Occasionally a transesophageal echocardiogram (TEE) may be needed to better assess the severity and etiology of pulmonary regurgitation.[7] In general, if TTE indicates severe pulmonary regurgitation, then a TEE would be recommended to better assess the degree and cause of regurgitation. TEE is also indicated in cases where pulmonary regurgitation is suspected but availability of TTE is limited. Rarely, the pulmonary valve leaflets may be difficult to visualize by TEE in the mid-esophageal position as the valve lies in the far field, but may be better characterized from the transgastric views. The development of 3-dimensional TEE is also improving visualization of these areas.
Catheterization and angiocardiography are less helpful in this setting because they may falsely elevate the quantity of pulmonary regurgitation as the catheter is crossing the pulmonary valve. Other imaging modalities, such as chest x-ray, magnetic resonance imaging (MRI), and computed tomography (CT), are also useful to identify pulmonary anatomy and the cause of pulmonary regurgitation and to quantify the degree of regurgitation. Additionally, MRI can measure pulmonary regurgitant fraction, RV end-diastolic and end-systolic volumes, and RV ejection fraction.[10][11] In patients where the decision to treat pulmonary regurgitation is being considered, an MRI and/or CT may be extremely helpful. Cardiac MRI is now considered the reference standard for quantification of PR, RV size, and RV function in patients with repaired tetralogy of Fallot. The advantages of cardiac MRI over other imaging modalities in these patients include accurate and reproducible measurements of the above-mentioned parameters, excellent image quality in patients with a wide range of body sizes, and the absence of radiation making it a good choice for longitudinal follow-up.[7][12] CT may be an alternative in patients with contraindications to MRI, such as pacemakers or other metallic implants.[7]
In patients with chronic pulmonary regurgitation, cardiopulmonary exercise testing may be a useful test to assess objective functional capacity and to follow patients longitudinally for changes over time related to worsening RV function.[Figure caption and citation for the preceding image starts]: Short axis echocardiographic view in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle, and short axis echocardiographic view reveals that the right ventricle is largeFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Short axis echocardiographic view in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle, and short axis echocardiographic view reveals a small right ventricleFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Short axis echocardiographic view in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle, and short axis echocardiographic view reveals a small right ventricleFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].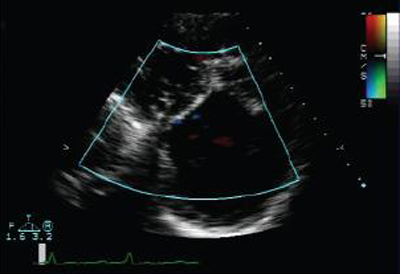 [Figure caption and citation for the preceding image starts]: Doppler echocardiogram in a patient with pulmonary regurgitation following repair of tetralogy of Fallot, revealing a non-obstructed right ventricular outflow tract. The patient has a restrictive right ventricleFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Doppler echocardiogram in a patient with pulmonary regurgitation following repair of tetralogy of Fallot, revealing a non-obstructed right ventricular outflow tract. The patient has a restrictive right ventricleFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].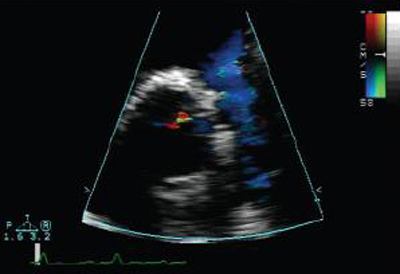 [Figure caption and citation for the preceding image starts]: Doppler echocardiogram in a patient with pulmonary regurgitation following repair of tetralogy of Fallot, revealing a nonobstructed right ventricular outflow tract. The patient has a nonrestrictive right ventricleFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Doppler echocardiogram in a patient with pulmonary regurgitation following repair of tetralogy of Fallot, revealing a nonobstructed right ventricular outflow tract. The patient has a nonrestrictive right ventricleFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].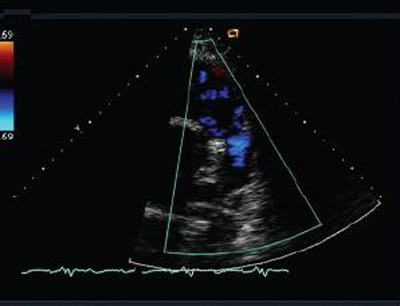 [Figure caption and citation for the preceding image starts]: Doppler in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a nonrestrictive right ventricle, and an ‘‘A’’ wave is not seen in the pulmonary artery Doppler spectrumFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Doppler in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a nonrestrictive right ventricle, and an ‘‘A’’ wave is not seen in the pulmonary artery Doppler spectrumFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].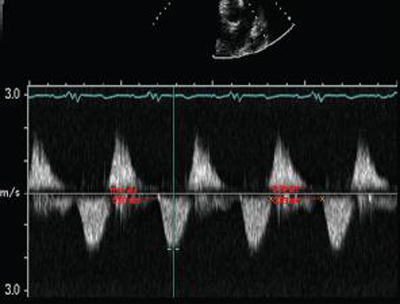 [Figure caption and citation for the preceding image starts]: Doppler in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle, and Doppler shows evidence of restriction with an antegrade "A" wave in the pulmonary arteryFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Doppler in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle, and Doppler shows evidence of restriction with an antegrade "A" wave in the pulmonary arteryFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Chest x-ray in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle and the heart is smallFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle and the heart is smallFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].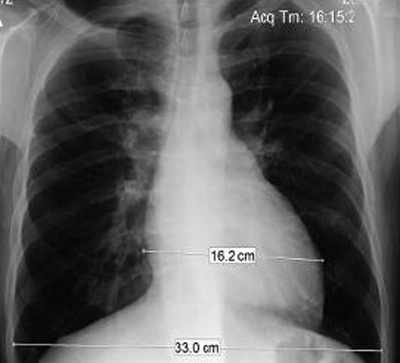 [Figure caption and citation for the preceding image starts]: Chest x-ray in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a nonrestrictive right ventricle and the heart is largeFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a nonrestrictive right ventricle and the heart is largeFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].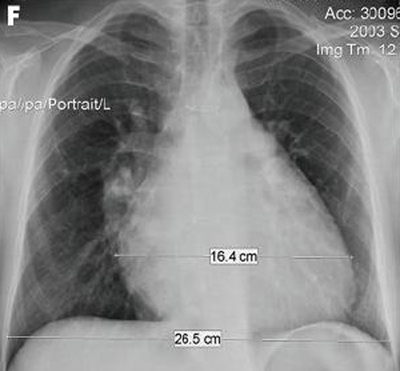 [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging (MRI) in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle, and MRI shows decreased right ventricular volumeFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging (MRI) in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a restrictive right ventricle, and MRI shows decreased right ventricular volumeFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].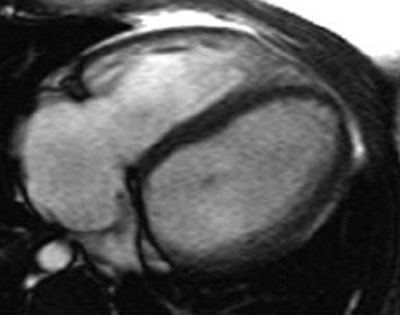 [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging (MRI) in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a nonrestrictive right ventricle, and MRI shows that the right ventricle is dilatedFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging (MRI) in a patient with pulmonary regurgitation following repair of tetralogy of Fallot. The patient has a nonrestrictive right ventricle, and MRI shows that the right ventricle is dilatedFrom: Chaturvedi RR, Redington AN. Heart. 2007 Jul;93(7):880-9; used with permission [Citation ends].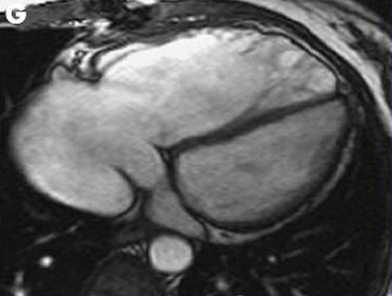
Use of this content is subject to our disclaimer