History and exam
Key diagnostic factors
common
cup-to-disk ratio >0.5
Increasing cup-to-disk ratio is associated with increased risk for developing open-angle glaucoma.[39][40]
A ratio of 0.7 may be a normal anatomic variant, while a ratio of 0.3 may indicate glaucoma if the ratio started at 0.1. Therefore, the change in cup-to-disk ratio is significant when determining damage.
Documenting an increase in cup-to-disk ratio is more meaningful than a cup-to-disk ratio determined at a single visit.[1][13][Figure caption and citation for the preceding image starts]: Photograph showing optic disk cupping. An increase in cup-to-disk ratio over time may indicate glaucoma.Collection of Robert B. Avery, MD, PhD [Citation ends].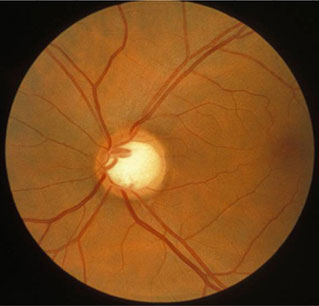 [Figure caption and citation for the preceding image starts]: Fundus photograph of normal optic nerve headCollection of Robert B. Avery, MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Fundus photograph of normal optic nerve headCollection of Robert B. Avery, MD, PhD [Citation ends].
notching of optic nerve cup
Good sensitivity and positive predictive value for glaucoma.[41]
symptomatic peripheral vision loss
Shown by missing areas in the field of vision (corresponding to disk appearances) in the absence of other identifiable causes, such as retinal detachment or strokes involving the visual pathways.
Indicates advanced disease.[13] Characteristic patterns of field loss in glaucoma include nasal defects or arcuate loss, often respecting the horizontal midline.
increased intraocular pressure
Common, but some patients may have a normal measurement at the time of diagnosis.[42]
scotomas
Found on visual field testing.
loss of nerve fiber layer
Used as a diagnostic factor (e.g., by optical coherence tomography).[13]
uncommon
optic disk hemorrhage
Appears on, or adjacent to, the optic nerve. Associated with normal-tension glaucoma.
Other diagnostic factors
common
corneal hysteresis
Generally low in glaucoma. Lower values may be associated with an increased risk of glaucoma progression.[29] Equipment is not widely available at present.
Risk factors
strong
intraocular pressure >21 mmHg
age >50 years
family history of glaucoma
genetic abnormalities
Mutations in the myocilin gene, which are present in 2% to 4% of patients with primary open-angle glaucoma, can lead to early-onset glaucoma and very high intraocular pressures.[13] Somatic mutations within myocilin may also accumulate with age and contribute to an increased risk for glaucoma.[16]
Glaucoma is a complex polygenic disease with multiple abnormalities reported in genes and novel single nucleotide polymorphisms.[23]
black ethnicity or Hispanic ethnicity
weak
diabetes mellitus
hypertension
Higher prevalence in patients with glaucoma.[27]
low ocular perfusion pressure
Risk of glaucoma may be increased risk in patients with either low diastolic (<50 mmHg) or low systolic (≤125 mmHg) perfusion pressure.[28]
thin central corneal thickness
Thin central corneal thickness is associated with higher progression rate from ocular hypertension to glaucoma, and a higher risk of glaucoma progression.[29]
corneal hysteresis
Corneal hysteresis refers to the corneal response to transient compression and release by an air-puff tonometer (i.e., the difference between the initial and rebound applanation pressure). Values may be lower in glaucoma, and lower values may be associated with an increased risk of glaucoma progression.[29]
Use of this content is subject to our disclaimer