Approach
The most effective way to prevent vision impairment is with early diagnosis and preventive treatment. A high index of suspicion should exist in patients with a family history of glaucoma or who describe peripheral vision loss.[8][12]
People often do not notice symptoms, such as a decrease in peripheral vision that can manifest as bumping into objects that they could not see.[32] Often the visual change will be more vague, being described as one eye seeming weak or dim compared to the other.
Assessment of the intraocular pressure (IOP), optic disk, and visual fields should be performed in all patients attending routine ophthalmologic exam.[4][33] Diagnostic procedures should be performed by appropriately trained and supervised personnel. Despite widespread use, confrontation visual fields can easily miss subtle damage.
Signs of current or previous inflammation, iris blood vessels, or iris transillumination defects may suggest an underlying disease causing secondary glaucoma.
Untreated, there is a progressive decline from normal vision to blindness in patients with glaucoma. A patient may present at any point along this continuum.
[Figure caption and citation for the preceding image starts]: The progressive journey from normal vision to blindness in glaucoma. There is a transition over time from normal visual function to blindness in patients with glaucoma. (A) Clinical examination or fundus photography can demonstrate and document the progression of optic disk cupping and neuroretinal rim thinning over time, that develops secondary to retinal ganglion cell loss. (B) Optical coherence tomography imaging quantifies changes in the thickness of the innermost layer of the retina around the optic disk and macula region, which comprise retinal ganglion cells and their axons, and can compare these measurements to normative databases. This enables detection and monitoring of structural changes at the optic nerve head and macula that might have developed due to glaucomatous injury. Structural changes often precede deficits in visual function and therefore optical coherence tomography imaging facilitates the detection of glaucoma at an early stage of disease. (C) Visual field testing allows for the detection and monitoring of impairment of visual function during the disease course. Early glaucoma is often asymptomatic as there is a threshold of retinal ganglion cell loss below which functional damage might not be detectable. (D) Even in the presence of substantial visual field defects, patients with glaucoma might remain asymptomatic as the brain can fill in the perceived picture using saccades and sensory inputs from the fellow eye. This means that patients might feel that their vision is normal until the very late stages of diseaseJayaram H, et al. Lancet 2023 Nov 11; 402(10414): 1788-801. doi: 10.1016/S0140-6736(23)01289-8. Epub 2023 Sep 21; used with permission [Citation ends].
Tonometry
Regular measurement at routine ophthalmologic exams is essential. The most common method is Goldmann tonometry. However, this procedure underestimates IOP in patients with thin corneas and overestimates IOP in patients with thick corneas.[12]
IOP measurement alone is not sufficient to determine the presence or absence of glaucoma because patients can have glaucoma with normal IOP. Conversely, patients with IOP above 21 mmHg do not necessarily have glaucoma (but should be considered to be at higher risk).
Gonioscopy
Gonioscopy is an essential exam. It is performed during slit-lamp exam by placing a mirrored lens on the surface of the eye to visualize the anterior chamber angle between the cornea and iris, and to assess fluid drainage. Typically, no obstruction is seen in open-angle glaucoma, differentiating the condition from angle-closure glaucoma, where an obstruction may exist.[1]
Retinal and optic disk visualization
The retina and optic disk should be visualized through direct and/or indirect ophthalmoscopy. Slit-lamp exam of the retina is usually carried out by an ophthalmologist.
Optimal exam requires pupil dilatation with eye drops. However, if narrow angles or angle-closure glaucoma are suspected and present, dilation could trigger additional pressure elevation.[34]
Direct ophthalmoscopy shines and reflects light onto the eye interior to provide a clear view of the retina and optic disk, with high magnification. It is the usual method of disk exam by nonophthalmologists. Indirect ophthalmoscopy provides a three-dimensional view of the retina and can show diagnostic optic disk cupping or indentation, but with limited magnification. Both instruments, used together, provide optimal information.
The ocular exam is normal apart from the characteristic damage to the optic nerve that manifests as a loss of nerve fibers and an increased cup-to-disk ratio. Neuroretinal fiber loss, notching of the optic nerve, and nasalization of blood vessels can also occur.
Pallor of the optic nerve and rim can be observed. A very pale optic rim is not typical for glaucoma and suggests other types of optic neuropathy.
Visual field exam
If glaucoma is suspected, an automated visual field test should be performe.[12][33] The pattern of field loss depends on the type of glaucoma.
In primary open-angle glaucoma, the visual field loss is usually peripheral with initial sparing of central vision. Closed-angle glaucoma may start from more central or paracentral defects. Glaucoma defects typically start horizontally, with defects that split down the vertical midline suggesting central defects in the brain or posterior visual pathway. It will usually correspond with the appearance of the optic nerve head (i.e., loss of the neuroretinal rim inferiorly will produce a superior visual defect). If a visual field test is needed but cannot be ordered, an ophthalmology referral is indicated.
First-time test takers often perform worse than on subsequent exam. The patient's alertness influences results; therefore, new scotomas are always confirmed by repeating the test on a different day.
Optical coherence tomography and digital imaging
Digital imaging of the optic nerve head, retinal nerve fiber layer, and macula is documented at baseline and follow-up to provide quantitative information of change that supplements, but does not replace, clinical exam.[8][13][33]
Optical coherence tomography (OCT) is the most widely used imaging modality for the diagnosis and monitoring of glaucoma. It provides digital images that can be used for several calculations and detailed comparison with the ophthalmologic exam. OCT has high sensitivity and specificity for glaucoma. Other imaging options include confocal scanning laser ophthalmoscopy and scanning laser polarimetry.[35][36]
Ongoing monitoring through serial scans is crucial to differentiate normal structural variants from glaucoma and to monitor disease progression over time. Serial OCT can:
Detect nerve fiber layer loss before visual field loss develops.[8][13] Preperimetric glaucoma will appear as changing structural alterations in the optic nerve head, macula, and parapapillary retinal nerve fiber layer before functional change occurs.
Document an increase in the cup-to-disk ratio.[1] For example, large optic nerve heads associated with myopia may have prominent cupping and still be normal, while hypoplastic optic nerve heads may have significant damage but retain small cups. Images of the optic nerve head can also show changes to the nerve rim (e.g., localized rim loss [notch], diffuse or concentric rim loss, larger cup-to-disk ratio). Images are repeated and compared each time a clinical change is detected.[Figure caption and citation for the preceding image starts]: Fundus photograph of normal optic nerve headCollection of Robert B. Avery, MD, PhD [Citation ends].
 [Figure caption and citation for the preceding image starts]: Photograph showing optic disk cupping. An increase in cup-to-disk ratio over time may indicate glaucoma.Collection of Robert B. Avery, MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Photograph showing optic disk cupping. An increase in cup-to-disk ratio over time may indicate glaucoma.Collection of Robert B. Avery, MD, PhD [Citation ends].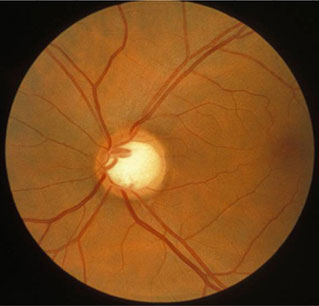
Help to analyze and monitor the thickness of the nerve fiber layer. Thicker tissue is healthier tissue. When structural thinning is observed, it may indicate normal variation or preperimetric glaucoma. Data regarding the thickness of the nerve fiber layer and any thinning are crucial for both diagnosis and follow-up evaluation.[8]
Be used to perform macular assessments with automated identification of the retinal ganglion cell layer or complex. This provides even greater sensitivity and earlier detection of both the disease and any deterioration.[37]
In cases where visual field testing is not possible due to patient noncompliance or clinical status, some physicians may rely on structural information from nerve fiber layer analysis in conjunction with other features of glaucoma.
Pachymetry
Pachymetry provides measurement of corneal thickness. Can be performed by OCT.
Thin central corneal thickness is associated with a higher rate of progression from ocular hypertension to glaucoma, and a higher risk of glaucoma progression.[29] A thick cornea can falsely increase the IOP reading. A thin central corneal thickness can provide a misleadingly low value for the IOP.[38]
Use of this content is subject to our disclaimer