Aortic stenosis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
clinically unstable
medical therapy or balloon valvuloplasty
The information in this treatment algorithm is largely based on recommendations from the American College of Cardiology/American Heart Association (ACC/AHA). For information on how recommendations from the UK National Institute for Health and Care Excellence (NICE) and the European Society of Cardiology/European Association for Cardio-Thoracic Surgery (ESC/EATC) differ, see Management Approach. Follow the recommended approach in your region.
All patients need to be stabilized prior to surgery or transcatheter aortic valve replacement (TAVR).
There has been concern that vasodilator therapy could be potentially dangerous, due to the possibility that a stenotic valve might permit only a fixed cardiac output, leading to hypotension. Vasodilator and beta-blocker therapy is not routinely given preoperatively on the day of surgery, although vasodilator therapy may be helpful for selected patients in closely monitored settings (e.g., ICU).
For patients with severe AS who are critically ill, need urgent noncardiac surgery, have cancer and an unclear long-term survival, are acutely symptomatic, or are in cardiogenic shock, balloon valvuloplasty is a reasonable option as a bridge to recovery and subsequent evaluation for surgical aortic valve replacement (SAVR) or TAVR.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
This is a percutaneous procedure done in the cardiac catheterization lab in which a balloon is forcefully inflated across the aortic valve to relieve stenosis. Unfortunately, restenosis rates are high at 6 months and there is no shown improvement in mortality following valvuloplasty. However, patients do generally experience improvement in hemodynamics and symptoms, which may provide an opportunity for more definitive care.[74]Letac B, Cribier A, Eltchaninoff H, et al. Evaluation of restenosis after balloon dilatation in adult aortic stenosis by repeat catheterization. Am Heart J. 1991 Jul;122(1 Pt 1):55-60.
http://www.ncbi.nlm.nih.gov/pubmed/2063763?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Balloon valvuloplasty fluoroscopy film that demonstrates valvuloplasty balloon inflated across a calcified aortic valveFrom the collection of David Liff, MD, Emory University Hospital; used with permission [Citation ends].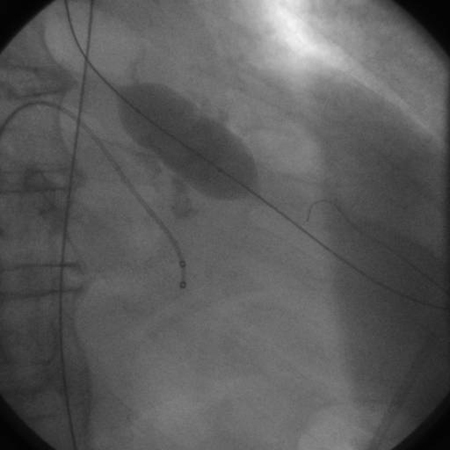
clinically stable: symptomatic
surgical aortic valve replacement
The ACC/AHA guidelines recommend surgical aortic valve replacement (SAVR) for symptomatic and asymptomatic patients with severe AS who meet an indication for aortic valve replacement (AVR) and who are <65 years of age or have a life expectancy >20 years. This includes patients with an LVEF <50%.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Prosthetic aortic valves used in surgical valve replacement may be mechanical or bioprosthetic.
AVR is recommended in symptomatic patients with severe AS, including those with low-flow/low-gradient severe AS with either a reduced left ventricular ejection fraction (LVEF) and persistent severe AS on low-dose dobutamine stress study, or a normal LVEF and evidence that valve obstruction is the most likely cause of symptoms.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term infective endocarditis antibiotic prophylaxis
Treatment recommended for ALL patients in selected patient group
Antibiotic prophylaxis for the prevention of infective endocarditis should be considered in patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts, before dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term anticoagulation
Treatment recommended for SOME patients in selected patient group
Anticoagulation with a vitamin K antagonist is indicated in patients who have had aortic valve replacement using prosthetic mechanical valves.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Direct oral anticoagulants (DOACs) are not recommended in patients requiring long-term anticoagulation for a mechanical valve regardless of coexisting atrial fibrillation.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Anticoagulation is not required if bioprosthetic valves are used, except in the presence of atrial fibrillation, where anticoagulation is indicated.
medical therapy
Treatment recommended for SOME patients in selected patient group
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
surgical OR transcatheter aortic valve replacement
The ACC/AHA guidelines recommend either surgery or transfemoral transcatheter aortic valve replacement (TAVR) for symptomatic patients with severe AS who are ages 65 to 80 years and have no contraindications to transfemoral TAVR, after shared decision-making based on the patient wishes, anatomic considerations, concomitant coronary artery disease and/or other valvular heart disease, comorbidities (e.g., frailty, dementia), and surgical risk.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term infective endocarditis antibiotic prophylaxis
Treatment recommended for ALL patients in selected patient group
Antibiotic prophylaxis for the prevention of infective endocarditis should be considered in patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts, before dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term anticoagulation
Treatment recommended for SOME patients in selected patient group
Anticoagulation with a vitamin K antagonist is indicated in patients who have had aortic valve replacement using prosthetic mechanical valves.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923 Direct oral anticoagulants (DOACs) are not recommended in patients requiring long-term anticoagulation for a mechanical valve regardless of coexisting atrial fibrillation.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Anticoagulation is not required if bioprosthetic valves are used, except in the presence of atrial fibrillation, where anticoagulation is indicated.
medical therapy
Treatment recommended for SOME patients in selected patient group
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
In patients who have undergone TAVR, renin-angiotensin system blocker therapy (ACE inhibitor or angiotensin receptor blocker) may be considered to reduce the long-term risk of all-cause mortality.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
transcatheter aortic valve replacement
The ACC/AHA guidelines recommend transcatheter aortic valve replacement (TAVR) in preference to surgery in symptomatic patients with severe AS who are: ages >80 years, or for younger patients with a life expectancy <10 years and no contraindication to transfemoral TAVR; of any age and have a high or prohibitive surgical risk, if the predicted post-TAVR survival is >12 months with an acceptable quality of life.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Surgical risk can be estimated using scoring systems such as the Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) and the EuroScore II.[46]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632. https://academic.oup.com/eurheartj/article/43/7/561/6358470 Society of Thoracic Surgeons: risk calculator Opens in new window These models utilize a variety of risk factors to predict postoperative outcome after valve surgery. Mortality estimates are used in conjunction with assessments of frailty, major organ system compromise, and procedure-specific impediments to classify each patient’s overall surgical risk: low risk; intermediate risk; high risk; prohibitive risk.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term infective endocarditis antibiotic prophylaxis
Treatment recommended for ALL patients in selected patient group
Antibiotic prophylaxis for the prevention of infective endocarditis should be considered in patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts, before dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term anticoagulation
Treatment recommended for SOME patients in selected patient group
Anticoagulation is not required if bioprosthetic valves are used, except in the presence of atrial fibrillation, where anticoagulation is indicated.
medical therapy
Treatment recommended for SOME patients in selected patient group
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
In patients who have undergone TAVR, renin-angiotensin system blocker therapy (ACE inhibitor or angiotensin receptor blocker) may be considered to reduce the long-term risk of all-cause mortality.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
clinically stable: asymptomatic
surgical OR transcatheter aortic valve replacement
The ACC/AHA guidelines recommend:
- Surgical aortic valve replacement (SAVR) in asymptomatic patients with severe AS and an LVEF <50%, who are ages <65 years or have a life expectancy >20 years.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923 Studies have reported significant differences in survival, beginning as early as 3 years post-valve replacement, between those with preoperative LVEF >50% and patients with LVEF <50%.[77]Schwarz F, Baumann P, Manthey J, et al. The effect of aortic valve replacement on survival. Circulation. 1982;66:1105-1110. http://circ.ahajournals.org/content/66/5/1105.full.pdf+html http://www.ncbi.nlm.nih.gov/pubmed/7127696?tool=bestpractice.com Delaying surgery in these patients may lead to irreversible LV dysfunction and worsened survival.
- Either surgical or transfemoral transcatheter aortic valve replacement (TAVR) in asymptomatic patients with severe AS and an LVEF <50%, who are 65 to 80 years of age and have no contraindications to transfemoral TAVR, after shared decision-making based on the patient wishes, anatomic considerations, concomitant coronary artery disease and/or other valvular heart disease, comorbidities (e.g., frailty, dementia), and surgical risk.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
- TAVR in preference to SAVR in asymptomatic patients with severe AS and LVEF <50% who are of any age and have: a life expectancy <10 years and no contraindication to transfemoral TAVR; a high or prohibitive surgical risk, if the predicted post-TAVR survival is >12 months with an acceptable quality of life.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Surgical risk can be estimated using scoring systems such as the Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) and the EuroScore II.[46]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632. https://academic.oup.com/eurheartj/article/43/7/561/6358470 Society of Thoracic Surgeons: risk calculator Opens in new window These models utilize a variety of risk factors to predict postoperative outcome after valve surgery. Mortality estimates are used in conjunction with assessments of frailty, major organ system compromise, and procedure-specific impediments to classify each patient’s overall surgical risk: low risk; intermediate risk; high risk; prohibitive risk.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term infective endocarditis antibiotic prophylaxis
Treatment recommended for ALL patients in selected patient group
Antibiotic prophylaxis for the prevention of infective endocarditis should be considered in patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts, before dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term anticoagulation
Treatment recommended for SOME patients in selected patient group
Anticoagulation with a vitamin K antagonist is indicated in patients who have had aortic valve replacement using prosthetic mechanical valves.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Direct oral anticoagulants (DOACs) are not recommended in patients requiring long-term anticoagulation for a mechanical valve regardless of coexisting atrial fibrillation.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Anticoagulation is not required if bioprosthetic valves are used, except in the presence of atrial fibrillation, where anticoagulation is indicated.
medical therapy
Treatment recommended for SOME patients in selected patient group
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
In patients who have undergone TAVR, renin-angiotensin system blocker therapy (ACE inhibitor or angiotensin receptor blocker) may be considered to reduce the long-term risk of all-cause mortality.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
surgical aortic valve replacement
The ACC/AHA guidelines recommend surgical aortic valve replacement (SAVR) in asymptomatic patients with severe AS and low surgical risk who have: an abnormal exercise test (i.e., decreased exercise tolerance [normalized for age and sex] or a fall in systolic blood pressure of ≥10 mmHg from baseline to peak exercise); very severe AS; rapid progression; elevated serum B-type natriuretic peptide (BNP) levels.
Surgical risk can be estimated using scoring systems such as the Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) and the EuroScore II.[46]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632. https://academic.oup.com/eurheartj/article/43/7/561/6358470 Society of Thoracic Surgeons: risk calculator Opens in new window These models utilize a variety of risk factors to predict postoperative outcome after valve surgery. Mortality estimates are used in conjunction with assessments of frailty, major organ system compromise, and procedure-specific impediments to classify each patient’s overall surgical risk: low risk; intermediate risk; high risk; prohibitive risk.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term infective endocarditis antibiotic prophylaxis
Treatment recommended for ALL patients in selected patient group
Antibiotic prophylaxis for the prevention of infective endocarditis should be considered in patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts, before dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term anticoagulation
Treatment recommended for SOME patients in selected patient group
Anticoagulation with a vitamin K antagonist is indicated in patients who have had aortic valve replacement using prosthetic mechanical valves.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Direct oral anticoagulants (DOACs) are not recommended in patients requiring long-term anticoagulation for a mechanical valve regardless of coexisting atrial fibrillation.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Anticoagulation is not required if bioprosthetic valves are used, except in the presence of atrial fibrillation, where anticoagulation is indicated.
medical therapy
Treatment recommended for SOME patients in selected patient group
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
consider surgical aortic valve replacement
Surgical aortic valve replacement (SAVR) may be considered in asymptomatic patients with severe AS and normal LV systolic function at rest and low surgical risk, when there is a progressive decrease in LVEF on at least three serial imaging studies to <60% without an alternative cause.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Surgical risk can be estimated using scoring systems such as the Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) and the EuroScore II.[46]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632. https://academic.oup.com/eurheartj/article/43/7/561/6358470 Society of Thoracic Surgeons: risk calculator Opens in new window These models utilize a variety of risk factors to predict postoperative outcome after valve surgery. Mortality estimates are used in conjunction with assessments of frailty, major organ system compromise, and procedure-specific impediments to classify each patient’s overall surgical risk: low risk; intermediate risk; high risk; prohibitive risk.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term infective endocarditis antibiotic prophylaxis
Treatment recommended for SOME patients in selected patient group
Antibiotic prophylaxis for the prevention of infective endocarditis should be considered in patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts, before dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term anticoagulation
Treatment recommended for SOME patients in selected patient group
Anticoagulation with a vitamin K antagonist is indicated in patients who have had aortic valve replacement using prosthetic mechanical valves.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Direct oral anticoagulants (DOACs) are not recommended in patients requiring long-term anticoagulation for a mechanical valve regardless of coexisting atrial fibrillation.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Anticoagulation is not required if bioprosthetic valves are used, except in the presence of atrial fibrillation, where anticoagulation is indicated.
medical therapy
Treatment recommended for SOME patients in selected patient group
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
consider concomitant prophylactic valve replacement
When patients with moderately stenotic valves undergo cardiac surgery, the decision to replace the valve is less clear cut than when there is severe stenosis. The increased risk of adding aortic valve replacement to the planned surgery needs to be balanced against the future likelihood of AS progressing to a severe, symptomatic state.
The ACC/AHA guidelines advise that aortic valve replacement with either transcatheter aortic valve replacement (TAVR) or surgical aortic valve replacement (SAVR) may be considered for asymptomatic patients with moderate AS who are undergoing other cardiac surgery.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term infective endocarditis antibiotic prophylaxis
Treatment recommended for SOME patients in selected patient group
Antibiotic prophylaxis for the prevention of infective endocarditis should be considered in patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts, before dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
long-term anticoagulation
Treatment recommended for SOME patients in selected patient group
Anticoagulation with a vitamin K antagonist is indicated in patients who have had aortic valve replacement using prosthetic mechanical valves.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Direct oral anticoagulants (DOACs) are not recommended in patients requiring long-term anticoagulation for a mechanical valve regardless of coexisting atrial fibrillation.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Anticoagulation is not required if bioprosthetic valves are used, except in the presence of atrial fibrillation, where anticoagulation is indicated.
medical therapy
Treatment recommended for SOME patients in selected patient group
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
In patients who have undergone TAVR, renin-angiotensin system blocker therapy (ACE inhibitor or angiotensin receptor blocker) may be considered to reduce the long-term risk of all-cause mortality.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
medical therapy and follow-up
Medical therapy for hypertension and hyperlipidemia is appropriate in patients with AS and hypertension and/or coronary artery disease.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923 Statin therapy is indicated for primary and secondary prevention of atherosclerosis in all patients with calcific AS on the basis of standard risk scores.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
Serial transthoracic echocardiograms are recommended every 3 to 5 years in asymptomatic patients with mild stenosis, and every 1 to 2 years in asymptomatic people with moderate stenosis.[26]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021 Feb 2;143(5):e72-227. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer