Tests
1st tests to order
ECG
Test
This is the most useful diagnostic test and should be ordered in all patients.
The classic ECG changes are global upwardly concave ST-segment (J-point) elevations with PR segment depressions in most leads with J-point depression and PR elevation in leads aVR and V1. If the patient is seen soon after symptom onset, PR depressions may be noted prior to ST elevation.
ECG changes occur in 60% of patients.[1] Temporal evolution of the ECG changes is highly variable. [Figure caption and citation for the preceding image starts]: ECG in a patient with acute pericarditis, showing diffuse ST-segment elevation in the precordial leads. There is also PR-segment depression in leads V2-V6 (arrows)Rathore S, Dodds PA. BMJ Case Reports 2009; doi:10.1136/bcr.2006.097071 [Citation ends].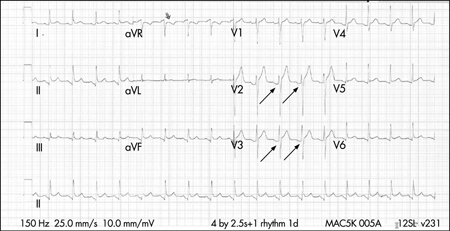
Result
upward concave ST-segment elevation globally with PR depressions
serum troponin
Test
Serum troponin can be ordered in all patients initially and serially.[12][15]
Elevated levels may be present and may reflect myocardial involvement (e.g., myopericarditis).
Plasma troponins are elevated in 35% to 50% of patients with pericarditis.
The magnitude of elevation correlates with extent of ST-segment elevation.
Levels can be in the range considered diagnostic of acute myocardial infarction in some patients. Levels return to normal within 1 to 2 weeks of diagnosis. Elevated levels do not appear to confer prognostic significance.
This test is not specific or sensitive.
Result
mildly elevated
pericardial fluid/blood culture
Test
Purulent pericarditis is immediately life-threatening and requires immediate confirmation of diagnosis via urgent pericardiocentesis.
Pericardial fluid should be tested for bacterial, fungal, and tuberculous causes, and blood should be drawn for culture.
Result
positive if infectious cause
erythrocyte sedimentation rate (ESR)
Test
Elevated ESR is consistent with an inflammatory state.[15]
Serial measurements may be helpful for monitoring disease activity and response to therapy.
Result
may be elevated
CRP
serum BUN
Test
Elevated levels of BUN (particularly >60 mg/dL) suggest a uremic cause.[15]
Result
elevated >60 mg/dL in renal failure
CBC
Test
Blood count does not provide definitive insight into the cause or management strategy. Leukocytosis with a marked shift to the left may be seen with purulent pericarditis or other infectious etiology.[15] Indicated before commencing colchicine therapy, which may cause neutropenia and bone marrow suppression.
Result
elevated white blood cells
chest x-ray
Test
Usually normal, unless a large pericardial effusion (>300 mL) is present, in which case the cardiothoracic ratio will be increased.[1]
Can also demonstrate concomitant lung pathology providing evidence of tuberculosis, fungal disease, pneumonia, or neoplasm that may be related to the disease.
Result
normal or water-bottle-shaped enlarged cardiac silhouette
echocardiography
Test
Indicated especially when cardiac tamponade is suspected. Can potentially help differentiate from acute coronary syndromes. Global ST elevations in the absence of left ventricular (LV) wall motion abnormalities and a trivial pericardial effusion supports the diagnosis of acute pericarditis. Insensitive to pericardial inflammation in dry pericarditis but is important in detecting pericardial effusions, which are found in up to 60% of cases and are generally small in size.[1][47][Figure caption and citation for the preceding image starts]: Echocardiogram in a baby with purulent pericarditis, showing a pericardial collection. LV = left ventricle, RV = right ventricleKaruppaswamy V, Shauq A, Alphonso N. BMJ Case Reports 2009; doi:10.1136/bcr.2007.136564 [Citation ends].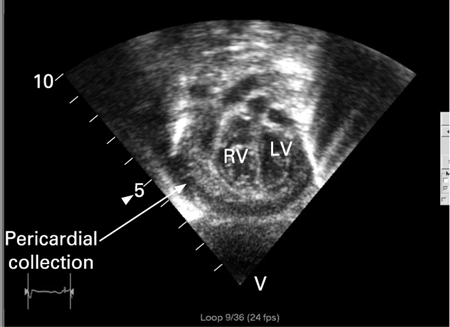
Result
may show a pericardial effusion; absence of LV wall motion abnormalities
Tests to consider
chest CT or cardiac MRI
Test
When the clinical presentation suggests other than uncomplicated pericarditis or the presentation is atypical, additional imaging with CT or MRI may be useful.[18][42][47]
May detect complications such as pericardial effusion or constrictive pericarditis, especially when the echocardiographic findings are inconclusive. Additional diagnostic information may also be obtained when there is associated chest trauma, particularly when penetrating; or in the setting of acute myocardial infarction, carcinoma, pulmonary or thoracic infection, or pancreatitis.
In cases of suspected constrictive pericarditis, CT and MRI provide accurate measurements of pericardial thickness and extent of pericardial thickening, which can be helpful for preoperative planning prior to pericardiectomy.[42][Figure caption and citation for the preceding image starts]: Chest CT showing a double layer of pericardial calcification in a 56-year-old male patient with idiopathic calcific constrictive pericarditisPatanwala I, Crilley J, Trewby PN. BMJ Case Reports 2009; doi:10.1136/bcr.06.2008.0015 [Citation ends]. [Figure caption and citation for the preceding image starts]: Chest CT in a baby with purulent pericarditis showing a pericardial collection with compression of the left (LV) and right (RV) ventriclesKaruppaswamy V, Shauq A, Alphonso N. BMJ Case Reports 2009; doi:10.1136/bcr.2007.136564 [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest CT in a baby with purulent pericarditis showing a pericardial collection with compression of the left (LV) and right (RV) ventriclesKaruppaswamy V, Shauq A, Alphonso N. BMJ Case Reports 2009; doi:10.1136/bcr.2007.136564 [Citation ends].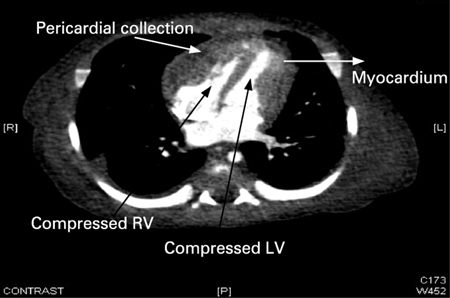
Result
pericardial effusion or constrictive pericarditis
pericardiocentesis/biopsy
Test
If tuberculous pericarditis is suspected, diagnostic accuracy can be improved with identification of the organism from pericardial fluid or pericardial biopsy.[43][44][45]
Adenosine deaminase activity within the pericardial effusion may also aid in the diagnosis as an adjunctive marker.[46]
Result
acid-fast bacilli, positive culture of Mycobacterium tuberculosis
Use of this content is subject to our disclaimer