Despite advances in technology, diagnosis is primarily clinically based, supported by ancillary tests such as ECG, chest x-ray, B-type natriuretic peptide (BNP), and echocardiogram.[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
[32]Heart Failure Society of America. Executive summary: HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194.
http://www.ncbi.nlm.nih.gov/pubmed/20610207?tool=bestpractice.com
The sensitivity of clinical assessment in identifying left ventricular systolic dysfunction is approximately 81% but the specificity is only 47%. The specificity of this diagnosis is improved to 69% by addition of ECG and to 92% by addition of chest x-ray.[33]Gillespie ND, McNeill G, Pringle T, et al. Cross sectional study of contribution of clinical assessment and simple cardiac investigations to diagnosis of left ventricular systolic dysfunction in patients admitted with acute dyspnoea. BMJ. 1997 Mar 29;314(7085):936-40.
http://www.bmj.com/cgi/content/full/314/7085/936
http://www.ncbi.nlm.nih.gov/pubmed/9099117?tool=bestpractice.com
Point-of-care lung ultrasound may be used as an alternative to chest x-ray in the emergency setting in conjunction with medical history and physical exam.[34]American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute heart failure syndromes. Jun 2022 [internet publication].
https://www.acep.org/globalassets/new-pdfs/clinical-policies/acute-heart-failure-syndrome-clinical-policy.pdf
[35]Qaseem A, Etxeandia-Ikobaltzeta I, Mustafa RA, et al. Appropriate use of point-of-care ultrasonography in patients with acute dyspnea in emergency department or inpatient settings: a clinical guideline from the American College of Physicians. Ann Intern Med. 2021 Jul;174(7):985-93.
https://www.acpjournals.org/doi/10.7326/M20-7844
http://www.ncbi.nlm.nih.gov/pubmed/33900792?tool=bestpractice.com
Other tests (e.g., cardiac catheterization with hemodynamic measurements, computed tomography [CT], and cardiac magnetic resonance [CMR] imaging) can be used when noninvasive tests and echocardiographic images are suboptimal or when an unusual cause of heart failure is suspected, and for diagnosis of specific cardiomyopathies.[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[36]Ezekowitz JA, O'Meara E, McDonald MA, et al. 2017 comprehensive update of the Canadian Cardiovascular Society guidelines for the management of heart failure. Can J Cardiol. 2017 Nov;33(11):1342-433.
https://www.onlinecjc.ca/article/S0828-282X(17)30973-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29111106?tool=bestpractice.com
History and risk factors
A careful history should be taken for causes of acute heart failure, such as myocardial ischemia, uncontrolled hypertension, significant valvular disease (both stenosis and regurgitation, or endocarditis), atrial fibrillation, other arrhythmias, infection, anemia, hyper- or hypothyroidism, pulmonary embolism, and precipitating factors causing exacerbation of chronic heart failure such as dietary indiscretion with excessive salt intake, nonadherence to medication regimen, use of medications with negative inotropic effect (e.g., verapamil, diltiazem) or medications that promote sodium retention, and excessive alcohol or drug intake.[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
A clinical scoring system is sometimes useful for the diagnosis of acute heart failure.[36]Ezekowitz JA, O'Meara E, McDonald MA, et al. 2017 comprehensive update of the Canadian Cardiovascular Society guidelines for the management of heart failure. Can J Cardiol. 2017 Nov;33(11):1342-433.
https://www.onlinecjc.ca/article/S0828-282X(17)30973-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29111106?tool=bestpractice.com
Symptoms
Heart failure presents with dyspnea (including orthopnea or paroxysmal nocturnal dyspnea), cough, decreased exercise tolerance, leg edema, fatigue, and generalized weakness. Sometimes the patient may present with predominant symptoms of the underlying condition, such as chest pain, syncope, palpitations, or viral prodrome.
Signs
Common signs include central cyanosis, tachycardia, elevated jugular venous pressure, displaced apex beat, third heart sound (S3), crepitations or pleural effusion, hepatomegaly, ascites, edema, and cool peripheries. The presence of these signs depends upon the duration, acuity, and the underlying cause of heart failure.[37]Renier W, Winckelmann KH, Verbakel JY, et al. Signs and symptoms in adult patients with acute dyspnea: a systematic review and meta-analysis. Eur J Emerg Med. 2018 Feb;25(1):3-11.
http://www.ncbi.nlm.nih.gov/pubmed/29252938?tool=bestpractice.com
Patients with end-stage heart failure may exhibit most of these clinical signs, whereas those in the early phase of the illness may have minimal signs.
Patients with advanced heart failure can be classified clinically into four hemodynamic profiles.[38]Nohria A, Lewis E, Stevenson LW. Medical management of advanced heart failure. JAMA. 2002 Feb 6;287(5):628-40.
http://jama.ama-assn.org/cgi/content/full/287/5/628
http://www.ncbi.nlm.nih.gov/pubmed/11829703?tool=bestpractice.com
These profiles, which are based on hemodynamic principles of presence or absence of elevated filling pressure (wet or dry) and perfusion that is adequate or critically limited (warm or cold), include:[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
Warm and dry
Warm and wet
Cold and dry
Cold and wet.
Patients with pulmonary edema present with severe respiratory distress with reduced oxygen saturation (usually <90% on room air) and crackles or wheezes on lung exam (“wet”) but may or may not be hemodynamically compromised (“cold” or “warm”). Patients with hemodynamic compromise, systolic BP less than 90 mmHg, or a drop of mean arterial pressure of more than 30 mmHg with a pulse rate over 60 bpm and/or low urine output (<0.5 ml/kg/hour), with or without evidence of organ congestion, are considered to be in cardiogenic shock (“cold”) but may or may not present with concomitant acute pulmonary edema (“wet” or “dry”).
Immediate investigations
An ECG and chest x-ray should be performed immediately in all patients with suspected acute heart failure.[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
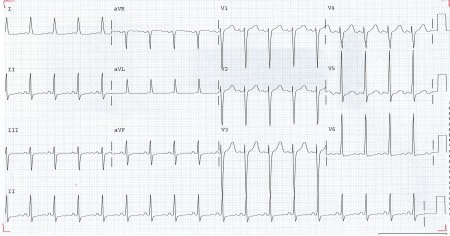
ECG findings are commonly related to the underlying pathologies and include presence of Q waves, ST-T changes, left ventricular hypertrophy (LVH), bundle branch block, and atrial fibrillation. ECG abnormality is found in almost all cases of heart failure. If the ECG is completely normal then alternate diagnosis should be considered.[39]Khan NK, Goode KM, Cleland JG, et al. Prevalence of ECG abnormalities in an international survey of patients with suspected or confirmed heart failure at death or discharge. Eur J Heart Fail. 2007 May;9(5):491-501.
http://www.ncbi.nlm.nih.gov/pubmed/17218150?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: ECG showing left ventricular hypertrophy with sinus tachycardiaFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].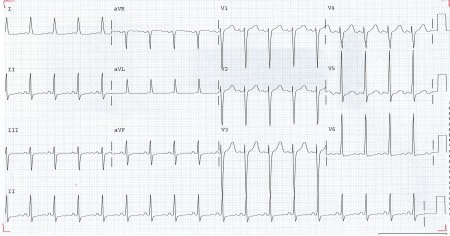
Chest x-ray may show cardiac enlargement (cardiothoracic ratio [CTR] >50%); however, there is poor correlation between the CTR and presence of heart failure, as the heart size may be normal in patients with diastolic dysfunction, acute valvular regurgitation as part of infective endocarditis, or acute myocardial infarction. An enlarged CTR may also be seen in the absence of heart failure (e.g., pericardial effusion and LVH).
In most cases, evaluation of the lung fields will show signs of pulmonary congestion, initially in the upper zones, then in the horizontal fissures, followed by pulmonary edema and pleural effusion.[Figure caption and citation for the preceding image starts]: Chest x-ray of acute pulmonary edema showing increased alveolar markings, fluid in the horizontal fissure, and blunting of the costophrenic anglesFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Chest x-ray of acute pulmonary edema showing increased alveolar markings and bilateral pleural effusionsFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray of acute pulmonary edema showing increased alveolar markings and bilateral pleural effusionsFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].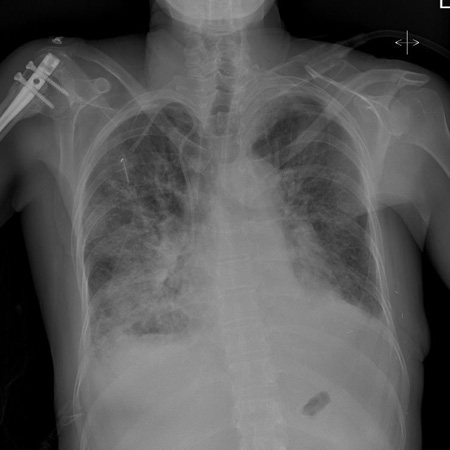
The radiologic findings have to be taken in the context of the clinical picture, as pulmonary infiltrates and congestion, in some cases, may be due to noncardiac causes such as acute respiratory distress syndrome or alveolar hemorrhage.
Chest x-rays rarely may show pericardial calcification, prosthetic valves, or valvular calcification. Such findings may be helpful in identifying the possible underlying etiology for heart failure.
Point-of-care lung ultrasound may be used as an alternative to chest x-ray when the equipment is available and clinicians are proficient in its use, alongside medical history and physical exam.[34]American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute heart failure syndromes. Jun 2022 [internet publication].
https://www.acep.org/globalassets/new-pdfs/clinical-policies/acute-heart-failure-syndrome-clinical-policy.pdf
[40]Čelutkienė J, Lainscak M, Anderson L, et al. Imaging in patients with suspected acute heart failure: timeline approach position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020 Feb;22(2):181-95.
https://onlinelibrary.wiley.com/doi/10.1002/ejhf.1678
http://www.ncbi.nlm.nih.gov/pubmed/31815347?tool=bestpractice.com
The following blood tests should be requested when patients present with suspected acute heart failure:[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
Hemoglobin: may identify anemia as a contributing factor.
Thyroid function tests: both hypothyroidism and hyperthyroidism can cause heart failure.
B-type natriuretic peptide (BNP): measurement of serum BNP level in patients with symptoms of heart failure is useful to support or exclude the diagnosis, and is recommended for patients hospitalized with heart failure to establish prognosis.[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
The addition of BNP or N-terminal pro-BNP (NT-proBNP) to clinical assessment significantly enhances the accuracy of diagnosis and effectiveness of acute management.[41]Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002 Jul 18;347(3):161-7.
http://www.nejm.org/doi/full/10.1056/NEJMoa020233#t=article
http://www.ncbi.nlm.nih.gov/pubmed/12124404?tool=bestpractice.com
[42]Mueller C, Scholer A, Laule-Kilian K, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med. 2004 Feb 12;350(7):647-54.
http://www.nejm.org/doi/full/10.1056/NEJMoa031681#t=article
http://www.ncbi.nlm.nih.gov/pubmed/14960741?tool=bestpractice.com
BNP is also helpful in differentiating a cardiac from a pulmonary cause of dyspnea.[43]Morrison LK, Harrison A, Krishnaswamy P, et al. Utility of a rapid B-natriuretic peptide assay in differentiating congestive heart failure from lung disease in patients presenting with dyspnea. J Am Coll Cardiol. 2002 Jan 16;39(2):202-9.
http://www.ncbi.nlm.nih.gov/pubmed/11788208?tool=bestpractice.com
A BNP >500 picograms/mL in a patient with dyspnea points to heart failure as the likely cause, whereas a BNP <100 picograms/mL makes heart failure unlikely. An elevated BNP level is a predictor of in-hospital mortality in patients with acute decompensated heart failure.[44]Fonarow GC, Peacock WF, Phillips CO, et al. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007 May 15;49(19):1943-50.
http://www.ncbi.nlm.nih.gov/pubmed/17498579?tool=bestpractice.com
However, an elevated BNP level should only be taken in the context of the clinical picture as it may be increased in a variety of other conditions, such as atrial fibrillation, pulmonary embolism, or sepsis.[45]Burke MA, Cotts WG. Interpretation of B-type natriuretic peptide in cardiac disease and other comorbid conditions. Heart Fail Rev. 2007 Mar;12(1):23-36.
http://www.ncbi.nlm.nih.gov/pubmed/17345160?tool=bestpractice.com
In patients presenting with suspected acute heart failure, a finding of BNP <100 picograms/mL, NT-proBNP <300 picograms/mL, and mid-regional pro-atrial natriuretic peptide (MR-proANP) <120 picograms/mL makes the diagnosis of acute heart failure unlikely.[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
Diagnostic accuracy can be improved by combining NT-proBNP assessment with other clinical variables using a validated clinical decision support tool.
CODE-HF tool
Opens in new window[46]Lee KK, Doudesis D, Anwar M, et al. Development and validation of a decision support tool for the diagnosis of acute heart failure: systematic review, meta-analysis, and modelling study. BMJ. 2022 Jun 13;377:e068424.
https://www.bmj.com/content/377/bmj-2021-068424
http://www.ncbi.nlm.nih.gov/pubmed/35697365?tool=bestpractice.com
Cardiac enzymes: >50% of patients with cardiogenic pulmonary edema (but without evidence for myocardial infarction) have elevated troponin T levels.[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[47]Perna ER, Macin SM, Parras JI, et al. Cardiac troponin T levels are associated with poor short- and long-term prognosis in patients with acute cardiogenic pulmonary edema. Am Heart J. 2002 May;143(5):814-20.
http://www.ncbi.nlm.nih.gov/pubmed/12040342?tool=bestpractice.com
Elevated troponin T levels in patients with acute heart failure may reflect subendocardial ischemia due to elevated left ventricular end diastolic pressure. In patients with acute cardiogenic pulmonary edema, a troponin T level ≥0.1 micrograms/L (≥0.1 ng/mL) is a powerful independent predictor and is associated with poor long-term survival.[47]Perna ER, Macin SM, Parras JI, et al. Cardiac troponin T levels are associated with poor short- and long-term prognosis in patients with acute cardiogenic pulmonary edema. Am Heart J. 2002 May;143(5):814-20.
http://www.ncbi.nlm.nih.gov/pubmed/12040342?tool=bestpractice.com
One systematic review and meta-analysis showed a strong association between high sensitive cardiac troponin and the development of incident heart failure.[48]Evans JDW, Dobbin SJH, Pettit SJ, et al. High-sensitivity cardiac troponin and new-onset heart failure: a systematic review and meta-analysis of 67,063 patients with 4,165 incident heart failure events. JACC Heart Fail. 2018 Mar;6(3):187-97.
http://www.ncbi.nlm.nih.gov/pubmed/29331272?tool=bestpractice.com
Other recommended initial baseline blood tests include serum electrolytes, blood urea nitrogen, serum creatinine, glucose, lipid profile, liver function tests (including albumin), and iron studies.[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
[49]El Iskandarani M, El Kurdi B, Murtaza G, et al. Prognostic role of albumin level in heart failure: a systematic review and meta-analysis. Medicine (Baltimore). 2021 Mar 12;100(10):e24785.
https://journals.lww.com/md-journal/fulltext/2021/03120/prognostic_role_of_albumin_level_in_heart_failure_.27.aspx
http://www.ncbi.nlm.nih.gov/pubmed/33725833?tool=bestpractice.com
Echocardiogram is an integral part of the evaluation in a patient with acute heart failure and should be performed as soon as possible to presentation.[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
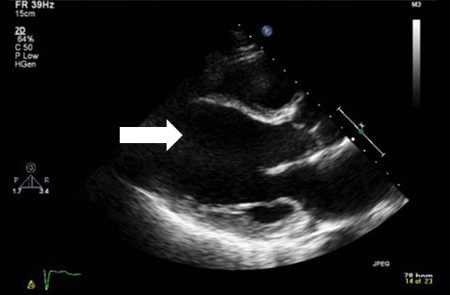
It is required to assess chamber size, ventricular function (systolic and diastolic), ventricular wall thickness, valvular function, and the pericardium. [Figure caption and citation for the preceding image starts]: Systolic image of dilated left ventricle (arrow); note there is no change from diastolic imageFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].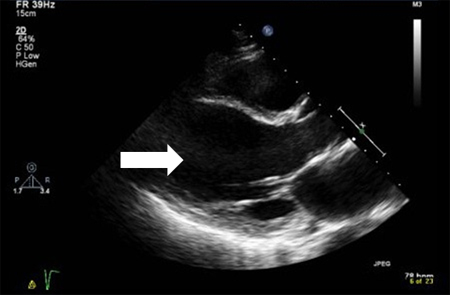 [Figure caption and citation for the preceding image starts]: Diastolic image of dilated left ventricle (arrow)From the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Diastolic image of dilated left ventricle (arrow)From the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].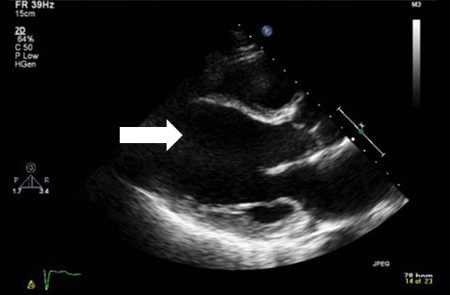
Subsequent investigations
Left heart cardiac catheterization (coronary angiogram) is needed in cases where significant coronary artery disease is thought to be a contributing factor.[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
Routine use of right heart catheterization and pulmonary artery catheter monitoring is not recommended. However, invasive hemodynamic evaluation or monitoring is helpful if:[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
Systolic blood pressure (SBP) remains low or symptoms persist despite treatment
Fluid status, perfusion, or systemic or pulmonary vascular resistance is uncertain
Renal function worsens with therapy
Parenteral vasoactive agents are required.
A cardiac CT coronary angiogram is a noninvasive technique to visualize the coronary anatomy in patients with heart failure with low to intermediate pre-test probability of coronary artery disease or those with equivocal noninvasive stress tests, in order to exclude the diagnosis of coronary artery disease.
Endomyocardial biopsy is not recommended for routine evaluation of acute heart failure, but is indicated in patients with rapidly progressive clinical heart failure or worsening ventricular dysfunction that persists despite appropriate medical treatment, where clinical findings suggest acute myocarditis, or where a myocardial infiltrative process (e.g., light chain amyloidosis) or cardiac rejection after heart transplantation is suspected.[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
Cardiovascular magnetic resonance (CMR) imaging can be used when noninvasive tests and echocardiographic images are suboptimal or when an unusual cause of heart failure is suspected, and for diagnosis of specific cardiomyopathies.[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
[36]Ezekowitz JA, O'Meara E, McDonald MA, et al. 2017 comprehensive update of the Canadian Cardiovascular Society guidelines for the management of heart failure. Can J Cardiol. 2017 Nov;33(11):1342-433.
https://www.onlinecjc.ca/article/S0828-282X(17)30973-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29111106?tool=bestpractice.com
Single-photon emission CT (SPECT) or positron emission tomography (PET) may be useful in assessing ischemia and myocardial viability. 3,3-diphosphono-1,2-propanodicarboxylic acid (DPD) scintigraphy may be useful for the detection of transthyretin cardiac amyloidosis.[1]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[2]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
Measuring the concentration of certain biomarkers can provide important information about disease severity and helps not only in the detection and diagnosis of heart failure but also in management and prognosis. In addition to natriuretic peptides and troponin, useful biomarkers include soluble suppressor of tumorigenicity 2, interleukin-6, cystatin-C, galectin-3, and procalcitonin.[50]Chow SL, Maisel AS, Anand I, et al. Role of biomarkers for the prevention, assessment, and management of heart failure: a scientific statement from the American Heart Association. Circulation. 2017 May 30;135(22):e1054-91.
https://www.doi.org/10.1161/CIR.0000000000000490
http://www.ncbi.nlm.nih.gov/pubmed/28446515?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Chest x-ray of acute pulmonary edema showing increased alveolar markings and bilateral pleural effusionsFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray of acute pulmonary edema showing increased alveolar markings and bilateral pleural effusionsFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].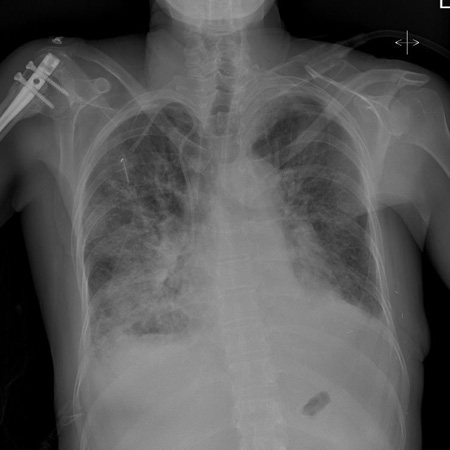
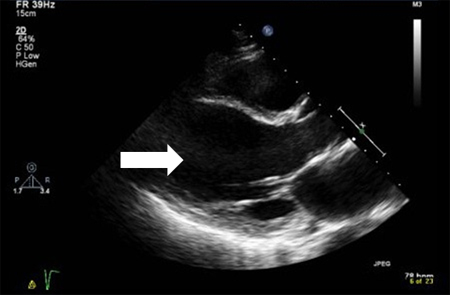 [Figure caption and citation for the preceding image starts]: Diastolic image of dilated left ventricle (arrow)From the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Diastolic image of dilated left ventricle (arrow)From the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].