Approach
There are no pathognomonic features that suggest polycystic ovary syndrome (PCOS), and it is largely a diagnosis of exclusion.
History
Common features include hirsutism (affecting 60%), acne (20%), and scalp hair loss (5%); irregular and infrequent periods (often <8 per year); weight gain; and infertility.[3]
Symptoms typically begin at the time of puberty and, in younger women, may be difficult to distinguish from the irregular menses that often occur in the first year after menarche.[50][51] Up to 85% of menses are anovulatory during the first year after menarche, and up to 60% in the third year; increased body mass index is a predictor of persistent anovulation. If oral contraceptives were begun at a young age, symptoms may be masked until therapy is stopped, which may delay the presentation and diagnosis.
While criteria for PCOS during adolescence are controversial, guidelines recommend that both oligo-ovulation and hyperandrogenism must be present to diagnose PCOS in a teenager:[52][53][54]
Infrequent/reduced menstrual bleeding or amenorrhea should be present for at least 2 years after menarche (or primary amenorrhea at age 15 years or >3 years after breast development).[53][55] Oligo- or anovulation may manifest irregular as menstrual bleeding, defined as >90 days for any one cycle 1 year post menarche; <21 or >45 days for those 1 to <3 years post menarche; <21 days to >35 days or <8 cycles per year for those ≥3 years post menarche to perimenopause.[53]
Physical exam
Hirsutism is the most characteristic physical exam finding. Acne and/or alopecia may be present. The degree of hyperandrogenism is typically mild to moderate. Frank virilization is rare.
Hirsutism can be quantified using the modified Ferriman-Gallwey score, with levels ≥4-6 indicating hirsutism.[53] It is important to ask about excess hair growth, because women often use methods of mechanical or local hair removal. Thus, the physical exam may not disclose hirsutism.
Acne may be masked by acne therapy. Severe acne persisting beyond adolescence may be more indicative of PCOS.
Typically, scalp hair loss in PCOS is at the vertex and crown, with relatively intact frontal hairline. Hair on the sides of the head may be preserved.
Body mass index and waist circumference should be assessed in all women with PCOS.[57] Depending on culture and ancestry, 30% to 80% of women with PCOS are overweight or obese, with central obesity (waist-to-hip ratio >0.85 or waist circumference >88 cm).
Women may have elevated blood pressure as a part of the hypertension sometimes associated with this syndrome.
Acanthosis nigricans, usually subtle, may be seen more in obese women with PCOS. [Figure caption and citation for the preceding image starts]: Acanthosis nigricans involving the axilla of an obese white womanFrom the collection of Melvin Chiu, MD, UCLA; used with permission [Citation ends].

Sweating or oily skin may occur.
Investigations
Hirsutism present
The diagnosis of PCOS can be made when infrequent/reduced menstrual bleeding also exists.
If infrequent/reduced menstrual bleeding is not present in a hirsute woman, evaluate for presence or absence of ovulation (by luteal-phase progesterone measurement or basal body temperature monitoring). Anovulatory cycling may occur, particularly in hirsute women. If such measures are consistent with anovulation, PCOS may be diagnosed in hirsute women.
If the hirsute woman has ovulatory cycles, the next step is to perform a transvaginal ultrasound to examine the ovaries. If polycystic ovarian morphology is documented, then PCOS can be diagnosed. In adults, pelvic ultrasound may be replaced by serum anti-Mullerian hormone (AMH) levels.[53]
Polycystic ovaries are present in 75% of women with PCOS, but are also seen in up to 25% of normal women and women with other endocrinopathies such as congenital adrenal hyperplasia, hyperprolactinemia, or hypothalamic amenorrhea.[3]
Ultrasound should be done in the early follicular phase (day 3-5) after a spontaneous or progestin-withdrawal-induced menstruation, or randomly in women with infrequent/reduced menstrual bleeding. If evidence of a dominant follicle (>10 mm) or a corpus luteum is seen, the ultrasound should be repeated at the next cycle.[2]
Polycystic ovarian morphology is a risk factor for ovarian hyperstimulation syndrome in women undergoing ovulation induction (with clomiphene or gonadotropins). Therefore, an ultrasound before ovulation induction may be useful.
If endometrial thickening is found, an endometrial biopsy is indicated to determine whether endometrial hyperplasia or cancer is present. Routine ultrasound screening for endometrial thickness is not recommended.[53]
It should be noted that ovarian volume and follicular number decrease with age, so standard criteria may not be applicable to women >40 years of age.[58] Also, multifollicular ovaries may be observed during puberty, subsiding once the normal menstrual pattern is established.[52]
In one meta-analysis, the pooled sensitivity of AMH for diagnosis of PCOS was 0.78 (95% CI: 0.74 to 0.81) and pooled specificity was 0.87 (95% CI: 0.84 to 0.90).[59] However, there was substantial heterogeneity between studies and optimal cut-off values have not been defined.[59]
Consider adolescents with only hyperandrogenism (and no irregular cycles) “at risk” of PCOS and reassess later.[53] Ultrasound and AMH levels are not recommended for diagnosis of PCOS in adolescents due to poor specificity in this age group.[53]
[Figure caption and citation for the preceding image starts]: Polycystic ovarian ultrasoundFrom the collection of Dr M. O. Goodarzi; used with permission [Citation ends].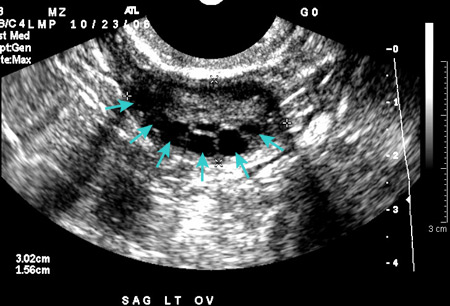
Hirsutism absent
If hirsutism is not present, serum androgens should be measured to evaluate for hyperandrogenism. The most commonly measured androgens are total and free testosterone and dehydroepiandrosterone sulfate (DHEAS). Biochemical hyperandrogenism is best assessed by calculated free testosterone, free androgen index, calculated bioavailable testosterone, or by high quality testosterone assays such as liquid chromatography tandem mass spectrometry or extraction/chromatography affinity immunoassays.[53] If any of these are elevated, the diagnostic sequence is the same as when hirsutism is present.
Levels >2 standard deviations above the mean qualifies as a positive test. Testosterone levels are difficult to measure in women; even assays using liquid chromatography mass spectrometry exhibit poor precision at the low levels characteristically found in women.[60] Additionally, many laboratory reference ranges for androgens in women did not carefully exclude women with PCOS.[61][62]
Hyperandrogenemia is present in 60% to 80% of women with PCOS: 70% have elevated free testosterone, 40% have elevated total testosterone, 25% have elevated dehydroepiandrosterone sulfate.[3] In obese women, sex hormone-binding globulin levels are low, resulting in elevated free testosterone and often normal total testosterone.
Androgen level tests should be performed in the follicular phase (in cycling women), in the morning, and at least 3 months after cessation of any hormonal therapies. An exception to these hormonal therapies is a cyclic progestin.[63]
If hirsutism is not present, all androgen levels are normal, and there is a history of infrequent/reduced menstrual bleeding, an ovarian ultrasound or serum AMH measurement should be performed in adults.[53] Combined with such a history, polycystic ovarian morphology allows a diagnosis of PCOS to be made (Rotterdam criteria only).[2]
Consider adolescents with only irregular cycles (and no hyperandrogenism) “at risk” of PCOS and reassess later.[53] Ultrasound and AMH levels are not recommended for diagnosis of PCOS in adolescents due to poor specificity.[53]
Levels of androstenedione or DHEAS may be checked if other androgens are normal, but these have lower specificity and DHEAS has greater age-associated decrease.[53] Androstenedione measurement may increase the number of women identified as hyperandrogenemic by 10%.[3] The American College of Obstetricians and Gynecologists PCOS guideline suggests evaluating DHEAS is of little value except in cases of rapid virilization.[64]
Checking dehydroepiandrosterone is of little value.
Tests in all women
Thyroid-stimulating hormone, prolactin, and 17-hydroxyprogesterone should be measured in all women to exclude disorders that may resemble PCOS (thyroid dysfunction, hyperprolactinemia, and 21-hydroxylase-deficient adrenal hyperplasia, respectively).[53][64] However, low-level prolactin elevations (20-30 ng/mL) are common in PCOS without associated galactorrhea or pituitary adenoma on imaging.
In uncertain cases, elevated luteinizing hormone (LH)/follicle-stimulating hormone (FSH) ratio may support a diagnosis of PCOS.
LH pulses are abnormally elevated (frequency and amplitude), leading to increased serum LH levels and LH/FSH ratio >3 in only two-thirds of women with PCOS. LH/FSH ratio is elevated more often in lean women. This ratio is helpful only if positive, and is not diagnostic.
Checking LH and FSH is also useful to rule out hypothalamic amenorrhea (levels low) or perimenopause/ovarian failure (levels high).
Given the high frequency of insulin resistance and metabolic syndrome in PCOS, an oral glucose tolerance test and fasting lipid panel should be performed in all women at diagnosis to evaluate metabolic risk factors.[53][64]
Diabetes is defined as fasting glucose ≥126 mg/dL, or 2-hour glucose ≥200 mg/dL.
Prevalence of abnormal glucose tolerance (impaired fasting glucose, impaired glucose tolerance, or diabetes) is as high as 40% in women with PCOS.[5] In one meta-analysis, the odds of prevalent impaired glucose tolerance was 3.3, and of prevalent diabetes 2.9, in women with PCOS.[65]
All women should be screened for impaired glucose tolerance with an oral glucose tolerance test. Those with normal glucose tolerance should be rescreened at least every 2 years. Those with impaired glucose tolerance should be screened annually for type 2 diabetes.[66]
Assessment of insulin resistance/hyperinsulinemia is problematic, given variability in insulin assays and the need for population-specific normative ranges. However, insulin levels may be measured to give insight into whether insulin resistance is present. Fasting insulin >10 to 15 microunits/mL may suggest insulin resistance.
During the oral glucose tolerance test, a peak insulin of 100-150 microunits/mL may indicate mild insulin resistance, 150-300 microunits/mL moderate insulin resistance, and >300 microunits/mL severe insulin resistance.[67]
Fasting plasma glucose or hemoglobin A1c are less accurate than oral glucose tolerance testing, but may be considered as second-line alternatives if an oral glucose tolerance test cannot be performed.[53][68]
Use of this content is subject to our disclaimer