History and exam
Key diagnostic factors
common
fever/chills
Most common presenting complaint.[7][21] Elderly or immunocompromised patients may present atypically, without fever.[7] Urgent evaluation for IE is important for any patient who presents with fever in conjunction with headache, meningeal signs, stroke symptoms, chest pain, dyspnea on exertion, orthopnea, or paroxysmal nocturnal dyspnea; and for any patient with unexplained fever who is at high risk of IE (e.g., congenital or acquired valvular disease, previous IE, prosthetic heart valves, congenital or heritable heart malformations, immunodeficiency, injection drug use).[20]
night sweats, malaise, fatigue, anorexia, weight loss, myalgias
Nonspecific constitutional symptoms.
weakness
The nature of weakness can be constitutional or focal. Systemic emboli should be suspected if patients present with asymmetric weakness consistent with stroke.
arthralgias
May represent a constitutional symptom or could be secondary to septic emboli to the affected joint.
headache
May represent a constitutional symptom or could be secondary to septic emboli.
shortness of breath
Dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea are features of congestive heart failure.
uncommon
meningeal signs
Secondary to septic emboli.
cardiac murmur
The classic new or worsening cardiac murmur is rare. Patients who develop new regurgitant murmurs are at increased risk of developing congestive heart failure.
Janeway lesions
Hemorrhagic, macular, painless plaques with a predilection for the palms and soles.[Figure caption and citation for the preceding image starts]: Janeway lesionsFrom the collection of Sanjay Sharma, St George’s University of London, UK; used with permission [Citation ends].
Osler nodes
Small, painful, nodular lesions usually found on the pads of the fingers or toes.[Figure caption and citation for the preceding image starts]: Osler nodeFrom the collection of Sanjay Sharma, St George’s University of London, UK; used with permission [Citation ends].
Roth spots
Oval, pale, retinal lesions surrounded by hemorrhage detected on fundoscopy.[Figure caption and citation for the preceding image starts]: Roth spotsFrom the collection of Sanjay Sharma, St George’s University of London, UK; used with permission [Citation ends].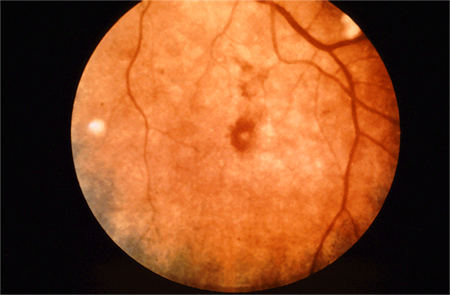
Other diagnostic factors
uncommon
splinter hemorrhages
May be noted in the nails of the upper and lower extremities. They are nonspecific.
cutaneous infarcts
May be noted in distal extremities. They are nonspecific.[Figure caption and citation for the preceding image starts]: Cutaneous infarctsFrom the collection of Sanjay Sharma, St George’s University of London, UK; used with permission [Citation ends].
chest pain
Can present with ischemic chest pain secondary to decompensated heart failure due to acute valvular regurgitation or coronary artery emboli.
back pain
Could represent discitis from septic emboli.
palatal petechiae
May be present.
Risk factors
strong
prior history of infectious endocarditis
presence of artificial prosthetic heart valves
certain types of congenital heart disease
Conditions meeting the American Heart Association criteria for being at highest risk of adverse outcome from endocarditis include: unrepaired cyanotic congenital heart disease, including palliative shunts and conduits; completely repaired congenital heart defect with prosthetic material or device placed by surgery or catheter intervention, during the first 6 months after the procedure; repaired congenital heart disease with residual defects at the site or adjacent to the site of a prosthetic device (which inhibit endothelialization); surgical or transcatheter pulmonary artery valve or conduit placement, such as Melody valve and Contegra conduit.[40]
The European Society of Cardiology classifies a patient as being at highest risk of developing IE if they have untreated cyanotic congenital heart disease, or congenital heart disease that has been repaired with a prosthetic material (including valved conduits or systemic-to-pulmonary shunts).[7]
The prevalence of congenital heart disease in adults has increased as a result of improved treatment options in childhood.[41]
postheart transplant (patients who develop a cardiac valvulopathy)
Regarded as one of the conditions associated with the highest risk of adverse outcome from endocarditis.[42]
immunocompromised state
Patients with compromised immune systems are more susceptible to infections, including IE. Many conditions can weaken the immune system including older age, poorly controlled diabetes, kidney disease, liver disease, malignancy, chronic steroid use, and history of solid organ transplantation.[21][43][44]
weak
presence of cardiac implanted electronic device or intravascular catheters (e.g., for hemodialysis)
acquired degenerative valve disease
There is good evidence that patients with congenital bicuspid aortic valvular stenosis are at increased risk; however, less evidence is available regarding degenerative aortic valvular stenosis.[7][21] Limited evidence suggests that mitral annular calcification can also act as a nidus for IE.[46]
mitral valve prolapse or bicuspid valve prolapse
The prevalence of mitral valve prolapse (MVP) in the general population is high, and patients with MVP have a three- to eight-times increased risk of IE compared to people with structurally normal hearts.[47]
Patients with MVP and those with bicuspid valve prolapse have a higher incidence of viridans group streptococci IE and IE from suspected odontologic origin than high-risk patients.[47][48] MVP with concomitant mitral regurgitation places patients at greater risk.[47] There is much debate regarding the efficacy of prophylaxis in patients with nonregurgitant MVP.[47]
hypertrophic cardiomyopathy
intravenous drug use
These patients are at greater risk of developing acute Staphylococcus aureus endocarditis.[3] One in every 10 invasive staphylococcal infections in the United States is attributable to intravenous drug use.[3]
Although tricuspid involvement has been shown to be significantly more frequent in endocarditis associated with intravenous drug use compared with no intravenous drug use, one study found that left-sided endocarditis was still more common than right-sided endocarditis in both groups.[14]
These patients have been shown to have worse clinical outcomes irrespective of drug use following surgery.[14]
chronic Q fever
Endocarditis is a serious complication of chronic Q fever. It typically affects middle-aged men with a history of significant exposure to animals and usually occurs in patients with preexisting valvular disease or who are immunocompromised.[50] Clinical presentation of chronic Coxiella burnetii endocarditis should be strongly considered in the differential diagnosis of culture negative endocarditis. A high index of suspicion in at-risk people with a fever of unknown origin, combined with serologic testing, ensures timely diagnosis.[50]
Use of this content is subject to our disclaimer