Etiology
The overall causative agents in IE are well documented and have been relatively stable, based on population-based studies over time. The most common pathogens are listed below; these together with any underlying risk factors indicate the most likely causative organism:[2][7][21][23][25]
Staphylococcus aureus (31% of cases)
Viridans group streptococci
Streptococcus gallolyticus (formerly Streptococcus bovis)
Oral streptococci ( Streptococcus mitis, Streptococcus sanguinis, Streptococcus anginosus, Streptococcus salivarius, Streptococcus downei, and Streptococcus mutans)
Coagulase-negative staphylococci
Enterococci
Culture-negative Haemophilus species, Aggregatibacter, Cardiobacterium hominis, Eikenella corrodens, and Kingella species (HACEK)
Fungi
Haemophilus parainfluenzae
Coxiella burnetii
Brucella species
Known but rare causative organisms of IE include:[26][27][28][29][30][31][32][33][34]
Trophyerma whipplei
Actinomyces
Nocardia
Malassezia furfur
Serratia species
Enterobacter cloacae
Mycobacterium chimaera
Rothia
Acinetobacter species
Klebsiella species
Patients who develop native valve endocarditis in the absence of intravenous drug use commonly present with viridans group streptococci, enterococci, or staphylococci, with other pathogens being less frequent. Intravenous drug users often present with right-sided valvular involvement and are more likely to have S aureus, streptococci, gram-negative bacilli, or polymicrobial infections.[2][3]
Prosthetic valve endocarditis is most commonly caused by coagulase-negative staphylococci, S aureus, enterococci, or gram-negative bacilli.[7] It should be noted that early prosthetic valve endocarditis is often caused by Staphylococcus epidermidis.[2][7][Figure caption and citation for the preceding image starts]: Photomicrograph of Streptococcus viridans bacteria that had been grown in a blood cultureCDC/Dr Mike Miller; used with permission [Citation ends].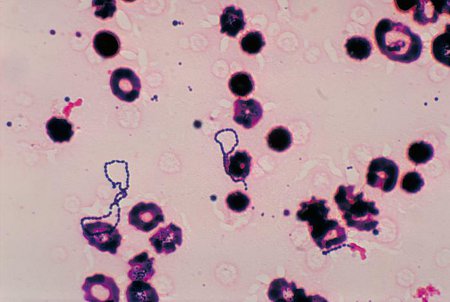
Pathophysiology
IE typically develops on the valvular surfaces of the heart, which have sustained endothelial damage secondary to turbulent blood flow. As a result, platelets and fibrin adhere to the underlying collagen surface and create a prothrombotic milieu. Bacteremia leads to colonization of the thrombus and perpetuates further fibrin deposition and platelet aggregation, which develops into a mature infected vegetation.[35]
Acute IE is usually associated with more virulent organisms, classically Staphylococcus aureus. Thrombus is formed by the offending organism and S aureus may invade endothelial cells and increase the expression of adhesion molecules as well as prothrombotic factors.[36]
Classification
Clinical classification[1]
Acute: typically develops over a period of days to weeks and is characterized by spiking fevers, tachycardia, fatigue, and progressive damage to cardiac structures.
Subacute: typically develops over the course of weeks to months. Often, patients will complain of vague constitutional symptoms.
Classification by nidus or location of infection
Native valve endocarditis (NVE)
Patients who develop NVE in the absence of intravenous drug use commonly present with viridans group streptococci, enterococci, or staphylococci, with other pathogens being less frequent. Intravenous drug users often present with right-sided valvular involvement and are more likely to have Staphylococcus aureus, streptococci, gram-negative bacilli, or polymicrobial infections.[2][3]
Prosthetic valve endocarditis (PVE)
Between 10% and 30% of all cases of IE occur in the context of prosthetic heart valves.[2][4] PVE is defined as being early or late depending on whether it arises within 1 year of valve replacement (early) or after 1 year (late). The focus is placed on the likely causative organisms involved at different time points in the disease process. Early PVE is often caused by S aureus or coagulase-negative staphylococci.[5][6][7] Late PVE tends to be caused by the same organisms as NVE, and nonsurgical treatment in this group may be effective.
Device-related endocarditis
The increasingly widespread use of cardiac implantable electronic devices (CIEDs) has contributed to the rising incidence of this complication, though it remains relatively rare overall.[8] Estimates of incidence vary but it is a serious complication that is often difficult to diagnose and carries with it significant mortality.[8][9][10][11]
Although clinically challenging, distinction should be made between local device infection and device-related IE. Device lead-associated endocarditis should be suspected in any CIED patient with systemic infection.[9][10][11] Patients with lead-associated endocarditis presenting less than 6 months after their most recent procedure are more likely to also have local device infection.[12] Those presenting after six months are more likely to have signs of systemic infection (such as fever, chills or sweats, or signs of sepsis) without evidence of local device infection.[9][12][13]
Risk factors for device-related IE include renal failure, hematoma at the site of implantation, diabetes mellitus, and anticoagulation.[9][10][11]
Right-sided endocarditis
Infections of right-sided heart valves make up 5% to 10% of the total cases of IE, and are commonly associated with intravenous drug users.[3][7][14]S aureus is the most common causative organism and accounts for 60% to 90% of cases.[15][16] The tricuspid valve is the most commonly affected, although the pulmonary valve is also susceptible to infection.[7]
Use of this content is subject to our disclaimer